Medicaid at 50
Low-Income Pregnant Women, Children and Families, and Childless Adults
Coverage
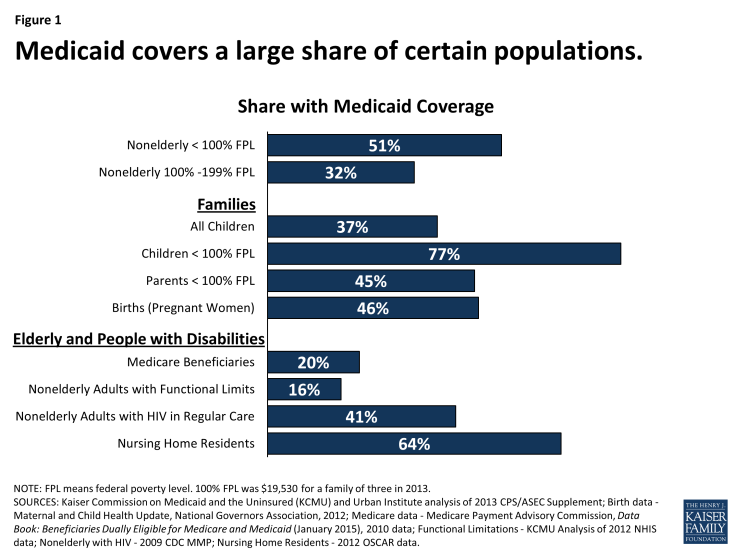
Medicaid’s most well-recognized role in our health care system is as a health coverage program for low-income pregnant women, children, and families. Currently, more than half the states provide Medicaid eligibility for pregnant women with incomes up to at least 200% of the federal poverty level (FPL) (about $40,000 for a family of three in 2015), and the Medicaid program finances almost half of all births. Roughly 33 million children, or more than 1 in 3, are covered by Medicaid (Figure 1).1 Medicaid plays an especially large coverage role for children of color, whose families are more likely to have low income compared to whites, and, as such, the program has reduced racial and ethnic disparities in children’s coverage. Medicaid also serves a large share of children with special health care needs.
Medicaid plays a major but much more limited coverage role for low-income nonelderly adults. In 2013, Medicaid covered over 75% of all children living below the poverty level but just 35% of adults in this income band. The reason for this disparity is two-fold. First, states have historically provided more restrictive eligibility for parents than for children. Second, until the ACA was enacted, nondisabled childless adults under age 65 were categorically excluded from Medicaid by federal law, no matter how poor they were. Prior to the ACA, some states pursued special federal waivers to cover some low-income childless adults under limited expansions of Medicaid. Demonstration waiver authority in section 1115 of the Social Security Act enables HHS to permit states to try approaches that are outside the statutory framework for Medicaid and still receive federal matching funds if the demonstration furthers the objectives of the Medicaid program.
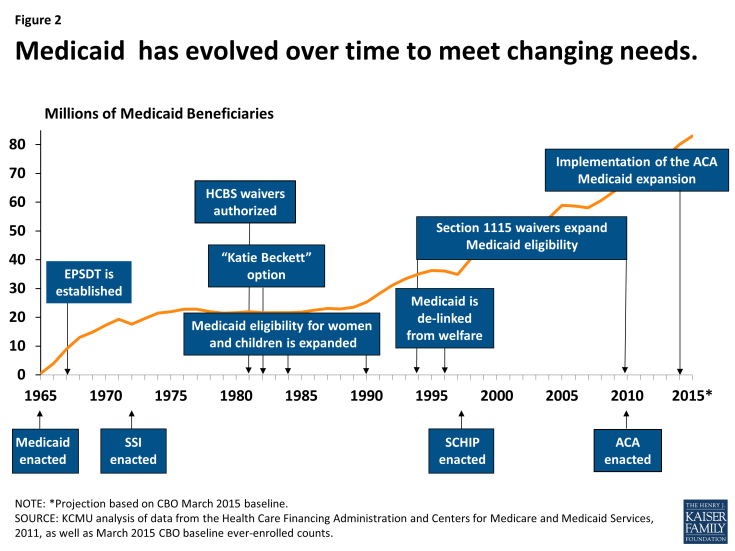
Medicaid’s role in providing health coverage for low-income pregnant women, children and families, and childless adults developed incrementally over time as both federal and state lawmakers expanded the program to cover broader segments of the uninsured population. Under the original 1965 Medicaid law, states were required to provide Medicaid eligibility to poor single parents and children receiving welfare through the Aid to Families with Dependent Children (AFDC) program, for which states set the income eligibility thresholds – frequently, well below 50% FPL. States were also granted broad flexibility to provide Medicaid to “medically needy” parents and children with income above the state’s AFDC threshold but high medical expenses relative to their income. Some states used this flexibility to extend coverage to more low-income families. The law also gave states an option to cover children in two-parent families with income up to the state’s AFDC threshold, regardless of whether the family was receiving welfare – so-called “Ribicoff children” for the Senator who authored the provision. This option was used widely by states to expand children’s coverage, and it can be seen as the kernel of later federal reforms that formally decoupled Medicaid eligibility from welfare status and recast Medicaid (for children, families, and, finally, childless adults) as an income-based health coverage program.
Over time, Congress, through stronger federal minimum requirements, and states, through their requests for and often vigorous take-up of new program options, built on the narrow early Medicaid platform to further expand and improve coverage for children and pregnant women (Figure 2). The Social Security Amendments of 1967 established the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program, Medicaid’s uniquely comprehensive benefit package for children up to age 21, which emphasizes early access to care and regular screenings to assess growth and development. The law required all states to cover EPSDT, overriding previous state-set limits on the amount, duration, and scope of services for children.2 In 1984, Congress moved to require rather than permit states to cover Ribicoff children under age 6 and, responding to concerns about rising infant mortality rates, required coverage of first-time pregnant women up to states’ AFDC thresholds as well.3 Subsequent legislation raised the federal minimum eligibility thresholds for both pregnant women and children, and many states chose to expand Medicaid eligibility beyond the federal minimum levels. In the late 1980s and early 1990s, in response to the still very low eligibility thresholds in place for pregnant women and children in some states, Congress required all states to cover pregnant women and children under age 6 with family income up to at least 133% FPL. Also, in 1989, EPSDT was significantly strengthened.4 In 1990, states were required to phase in Medicaid coverage for school-age children (age 6-18) with family income up to 100% FPL, an expansion that was completed in 2002, establishing Medicaid eligibility for all children in poverty nationwide.
In 1996, in a major federal overhaul of the welfare program, which is now known as Temporary Assistance for Needy Families (TANF), Congress de-linked Medicaid eligibility from welfare eligibility and gave states flexibility to expand income eligibility for Medicaid broadly to cover more working families. Severing Medicaid from its welfare roots fundamentally altered Medicaid, transforming it from a welfare program to a health coverage program for low-income children and families. In 1997, Congress built on Medicaid yet again, establishing the State Children’s Health Insurance Program (CHIP), which provides enhanced federal matching funds to states to cover low-income children above the cut-off for Medicaid through either an expansion of Medicaid or a separate CHIP program. Responding to the high federal match rate and interest in expanding coverage for children, states embraced CHIP and, for the first time, conducted vigorous outreach and enrollment campaigns. In many states, efforts to promote participation in CHIP carried over to Medicaid, marking a sea change in the program’s orientation, from gate-keeping to gate-opening, as far as children were concerned.
While the progression of Medicaid expansions resulted in broad coverage of low-income children, Medicaid coverage of their parents lagged far behind, and the categorical exclusion of most childless adults from Medicaid left even the poorest of these individuals without access to coverage. It was against this backdrop that the ACA ushered in the most recent era of Medicaid expansion. The health reform law expanded Medicaid eligibility to nonelderly adults with income up to a uniform federal threshold of 138% FPL (about $16,250 for an individual in 2015) and provided nearly full federal financing for the cost. This expansion established Medicaid as the health coverage program for nearly all low-income Americans under age 65 within the broader system the ACA created to cover the uninsured.
The ACA also raised the minimum Medicaid eligibility threshold for school-age children to the same level that applies for younger children, eliminating previous age-based differences in minimum eligibility standards, and extended Medicaid coverage for foster care children up to age 26 (paralleling the requirement that private insurers offering dependent coverage for children allow those up to age 26 to remain on their parent’s plan). In addition, the ACA required states to take far-reaching measures to modernize and streamline the Medicaid application, enrollment, and renewal processes to be coordinated with the new Marketplaces.
Unexpectedly, the Medicaid expansion to low-income adults hit a major hurdle in the Supreme Court’s landmark decision on the ACA in National Federation of Independent Business v. Sebelius.5 The Court ruled that the Medicaid expansion was unconstitutionally coercive and the decision limited the HHS Secretary’s enforcement authority, effectively making the expansion optional for states. As of this writing, 29 states and the District of Columbia have adopted the Medicaid expansion, including several recently, and other states are debating the issue, evidence that the picture may continue to evolve.
The federal and state expansions of Medicaid over the last five decades have had a dramatic impact on coverage of low-income children and adults in the U.S. In 2011, almost 33 million children and more than 18 million pregnant women, parents, and other nonelderly, nondisabled adults were enrolled in the program. The greatest impact of Medicaid and CHIP has been on children’s coverage. Between 1997 and 2012, the uninsured rate among children fell by half, from 14% to an historic low of 7%.6 Currently, more than half the states cover children with family income up to at least 250% FPL (about $50,000 for a family of three.)7 The ACA Medicaid expansion has brought coverage to millions of additional uninsured, nonelderly parents and childless adults in the states that have implemented it. Federal data show that, in September 2014, at least 4.6 million low-income adults were covered through the new adult expansion group in the 23 states for which data were available (of 27 states that had adopted the expansion by then).8 This figure does not include an estimated 1.2 million newly eligible adults in California or enrollment in three additional states that have adopted the expansion in the meantime.9
While Medicaid has been instrumental in reducing the number and share of low-income nonelderly Americans without health insurance, the ACA vision of Medicaid as a universal program for this population has yet to be fully realized. In 2013, over 7 million children remained uninsured, of whom an estimated 5.2 million would qualify for Medicaid or CHIP, pointing to needs for targeted outreach and enrollment efforts.10 A more substantial share of adults who would be eligible for Medicaid are not enrolled in the program, again a signal that more intensive and targeted efforts are needed to engage this hard-to-reach population.11 Also, Medicaid and CHIP income eligibility thresholds for children and nonelderly adults in the states not expanding Medicaid lag behind those in the states moving forward (Figure 3). Further, nearly 4 million poor adults in the non-expansion states fall into the “coverage gap” because their income is too high for Medicaid but too low to qualify for premium subsidies to purchase Marketplace coverage.12 Notably, Blacks, who reside in high numbers in many of the non-expansion states, disproportionately fall into the coverage gap.13
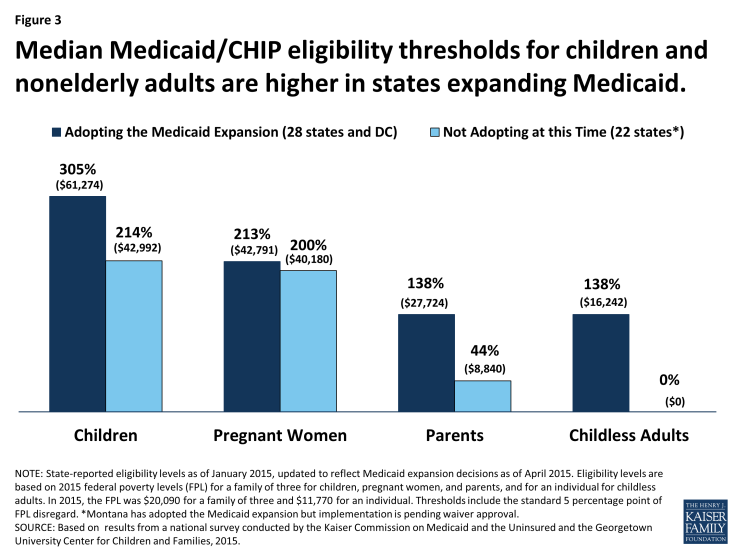
Figure 3: Median Medicaid/CHIP eligibility thresholds for children and nonelderly adults are higher in states expanding Medicaid.
Impact
The goal of Medicaid coverage is to facilitate access to care for low-income people and to provide financial protection against high out-of-pocket costs for health care. A large body of research shows that the program largely succeeds in this purpose. Still, there remain challenges for Medicaid in facilitating access to care. Many factors bear on access to care, including the scope of Medicaid benefits covered by states, limits on Medicaid premiums and cost-sharing, provider payment and participation in Medicaid, transportation and language barriers, and features of the larger health care ecosystem of which Medicaid is part.
Children
Medicaid’s EPSDT benefits for children up to age 21 are considered a model of pediatric coverage. EPSDT is unusually comprehensive and emphasizes early intervention, before preventable health problems become permanent. Its benefits include immunizations and other preventive and primary care services, prescription drugs, hospital care, vision, dental, and hearing services, diagnostic and treatment services, and all other services permitted under federal Medicaid law. Further, the medical necessity standard that governs EPSDT requires states to cover services to correct or ameliorate the effects of physical and mental illnesses and conditions for children. This expansive definition is designed to ensure robust access to care for low-income children, including access to services and supports such as medical equipment, speech, physical, and occupational therapy, and assistive technology for children with special needs.14 To ensure that financial barriers do not impede their access, premiums are prohibited in Medicaid for children below 150% FPL and cost-sharing is tightly restricted for all children. Although children make up nearly half of all Medicaid beneficiaries, they account for about 20% of Medicaid spending, a reflection of their relatively routine and low-cost health care needs and costs compared to others covered by the program, especially beneficiaries with disabilities and those over age 65.
Strong access to primary care among children covered by Medicaid is well-documented (Figure 4).15 16 Nearly all children with Medicaid have a usual source of care, which research shows enhances access to and appropriate use of health care services.17 Compared to uninsured children, children with Medicaid are far more likely to have a usual source of care, visit physicians and dentists, and get recommended preventive care, and they are less likely to have unmet needs for medical, dental, and specialty care and prescription drugs. Furthermore, rates of access to preventive and primary care for children with Medicaid or CHIP are fairly comparable to those for children with employer-sponsored insurance (ESI) despite sharp differences between the health status and demographic and socioeconomic profiles of the two groups. When these differences are controlled, rates of access to specialist care are also similar between publicly insured children and those with ESI.18 Notably, children across the board, including those covered by Medicaid or other types of insurance, get preventive care at rates below recommended levels.
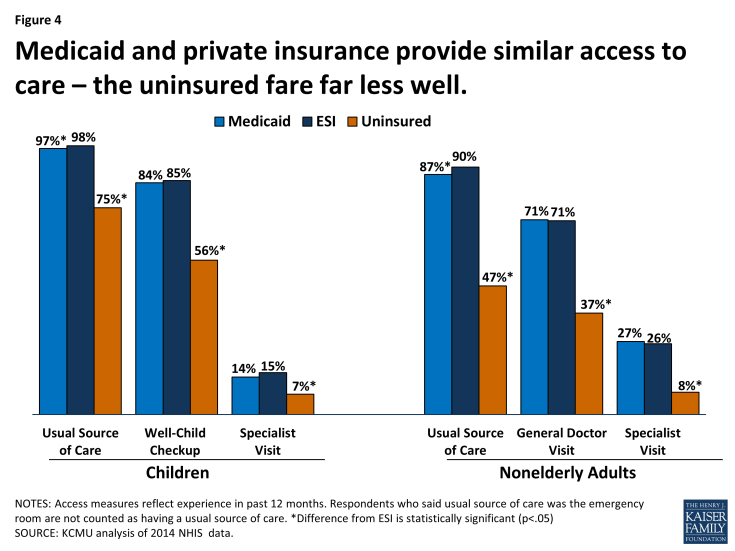
Figure 4: Medicaid and private insurance provide similar access to care – the uninsured fare far less well.
Children’s access to oral health services is a key concern in Medicaid. Since severe problems obtaining dental care for children enrolled in Medicaid came to light in the mid-2000s, CMS and the states have made targeted efforts and investments in this area. Although substantial improvements have resulted, in 2013, the share of Medicaid-enrolled children who received at least one preventive dental service a year exceeded 50% in only half the states.19 Children with private dental coverage are generally more likely to get preventive dental care, but, as with other preventive care, rates of preventive dental care are well below recommended levels for all children.20
While population-level findings on access to care in Medicaid indicate high performance overall, direct studies of access at a local level, using “secret shopper” techniques, show that children with Medicaid or CHIP are much more likely than privately insured children to be denied appointments with specialists and that they face longer waits when they do get appointments.21 These findings, which are consistent with lower rates of provider participation in Medicaid compared to private insurance, are informative about beneficiaries’ care-seeking experience and their more limited choice of providers, but it is important to consider them in the context of consistent evidence of high rates of realized access to care in the Medicaid program overall.22
A growing body of research provides evidence that Medicaid and CHIP coverage confer benefits on children beyond improved access to care. Studies show gains in children’s health and health behaviors, improved performance in school, fewer days of missed school due to illness or injury, and higher long-run educational attainment, including high-school completion, college attendance, and college graduation among children covered by Medicaid in their childhood and youth.23 24 25
Nonelderly Adults
Medicaid law authorizes comprehensive benefits for adults, including physician and hospital care, lab and x-ray services, prescription drugs, and non-emergency medical transportation. Medicaid benefits for reproductive care, including both maternity care and family planning services, and breast and cervical cancer screening and treatment, are extremely important for low-income women, who make up two-thirds of nonelderly adult enrollees, and Medicaid expansions to pregnant women are credited with reductions in infant mortality and low birth weights as well as improved health outcomes for children.26 Whereas federal EPSDT requirements establish a uniformly comprehensive Medicaid benefit package for children nationwide, states have substantial flexibility in defining Medicaid benefits for adults and the range and scope of adult benefits vary widely by state as a result. Benefits for adults in the new Medicaid expansion group must include the 10 categories of “essential health benefits” defined by the ACA, but states retain considerable flexibility to design them. Similar to children, nonelderly adults without disabilities are a low-cost Medicaid population. In 2011, nonelderly, nondisabled adults made up about one-quarter of Medicaid beneficiaries but accounted for a fairly small share of Medicaid spending (15%), reflecting both low Medicaid spending per enrollee and limited Medicaid eligibility for this population.
The empirical findings on adults’ access to care in Medicaid are largely positive. Because of its rigorous design, the recent Oregon Health Insurance Experiment provides particularly strong evidence of Medicaid’s impact. Taking advantage of a 2008 lottery that randomly allocated a limited number of new Medicaid “slots” for low-income uninsured adults, investigators compared access to care and selected health outcomes between the adults who won Medicaid coverage and the adults who did not. Study findings one and two years out from the lottery showed higher use of preventive services and other care, improved self-reported health, and reduced clinical depression among the adults who gained Medicaid coverage compared to the others.27 28 The risk of medical debt also declined significantly in the Medicaid group and catastrophic medical costs were virtually eliminated for them. On the other hand, the observed reductions in blood pressure, cholesterol levels, and blood glucose levels were not statistically significant. On this point, the researchers noted limitations in the study’s statistical power. A separate team of investigators, using cost-effectiveness analysis, found that the Oregon Medicaid expansion was a good public investment, providing a net financial return to society.29
The evidence from studies comparing Medicaid and privately insured adults’ access to care closely mirrors the evidence for children. The vast majority of adults in both insurance groups have a usual source of care. When health, demographic, and socioeconomic differences between the two groups are controlled, Medicaid adults are as likely as the privately insured to have received recommended preventive care, a general doctor visit, and a specialist visit in the past 12 months.30 Research shows that, compared to adults with similar characteristics who have ESI, adults covered by Medicaid have similar rates of delayed and unmet needs for medical care.31 32 Medicaid also affords greater financial protection from medical expenses; it has been projected that adult Medicaid beneficiaries’ out-of-pocket spending would increase more than three-fold if they were covered by ESI instead, even though their expected health care use would not be much different. Again mirroring the findings for children, direct studies of access to care for adults show that physicians are more willing to serve those with private insurance than those with Medicaid coverage.33 34 This pattern has led to concerns about provider availability in Medicaid as more adults gain coverage. Anticipating increased demand for services due to expanded coverage, the ACA temporarily raised Medicaid fees for many primary care services, which are typically very low, to Medicare fee levels to garner greater primary care physician participation in Medicaid. Findings that physician participation rates are higher in states with higher Medicaid payment rates relative to other payers suggest that provider payment rates may be an effective tool for leveraging increased access to care.35
Because major chronic illnesses are prevalent among Medicaid adults and securing access to care is arguably most challenging for those with the greatest needs, the experience of beneficiaries with chronic conditions is an important gauge of access in Medicaid. In this regard, a suite of studies has shown significant and clinically meaningful differences in access and care between nonelderly adults with Medicaid and those who are uninsured. One of the studies, which focused on diabetes, found that adults enrolled in Medicaid were less likely than their uninsured counterparts to report being unable to get needed care, had more office visits and filled more prescriptions, and were more likely to get key elements of recommended diabetes care. The companion analyses looking at cardiovascular disease, respiratory disease, and mental illness reached similar findings.36 37 38 39 40
The vast majority of adults who have ever received Medicaid benefits say that their overall experiences have been positive.41 At the same time, there are some areas of serious concern for adult access to care in Medicaid. In particular, while needs for behavioral health care are great among adult Medicaid beneficiaries and demand for these services is likely to grow with the Medicaid expansion, psychiatrist participation in the program is very low and there is a growing workforce crisis in the field of addiction treatment.42 43 Lack of access to dental care is also a major problem. Poor oral health is associated with chronic conditions including diabetes and heart disease and can also interfere with nutrition; poor or missing teeth adversely affect employability as well. Nonetheless, adult dental benefits are optional under federal Medicaid law and they are not included among the ACA’s essential health benefits for newly eligible adults. Most states cover limited or emergency-only dental services for adults, but dental care is very expensive and few Medicaid beneficiaries can afford to pay for it out-of-pocket. Many other benefits, such as eyeglasses and physical therapy, are also optional for adults, and states often drop or cut back on these benefits when they are facing tight budgets.