The Role of Medicaid in Rural America
| Key Takeaways |
This brief describes Medicaid’s role for 52 million nonelderly children and adults living in the most rural areas in the United States and discusses how expansions or reductions in Medicaid could affect rural areas. It shows:
Additional action to expand Medicaid within the 19 states that have not yet adopted the Medicaid expansion would likely lead to further increases in coverage among individuals living in rural areas. These non-expansion states are home to 59% of nonelderly uninsured individuals living in rural areas. Conversely, cuts to Medicaid could disproportionately affect people living in rural areas given the large role of the program in these areas. |
Introduction
People in rural areas face unique challenges in health care coverage and access, including low density of providers and longer travel times to care, limited access to employer-sponsored coverage, and greater health care needs due to older age and lower income. Medicaid plays an important role in helping to address these challenges. This brief provides insight into the role of Medicaid in rural areas and discusses how expansions or reductions in Medicaid such as those currently under debate could affect rural areas. The analysis is based on data from the 2013-2015 American Community Survey and classifies counties as “rural” based on an Index of Relative Rurality (IRR). We group counties into quintiles of rurality and define those with the highest degree of rurality as “rural,” those with the lowest degree as “urban,” and those in the middle as “other.” While Medicaid provides assistance to many low-income elderly individuals, primarily as a wrap-around benefit to Medicare, this analysis focuses on its role in covering nonelderly children and adults. The analysis shows that Medicaid plays a particularly important role providing coverage in rural areas and that gains in Medicaid coverage have helped reduce the uninsured rate in rural areas. More detail on the methods underlying the analysis is available in the “methods” box at the end of the brief.
Where is Rural America and Who Lives There?
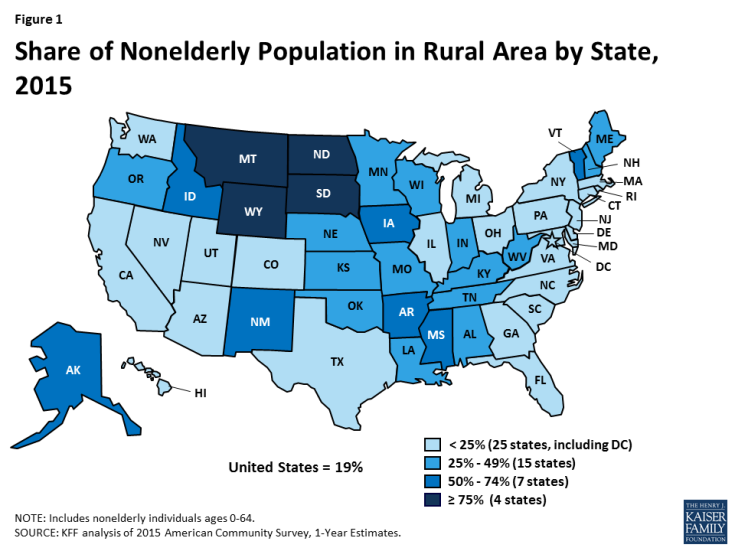
The nearly 20% of the nonelderly population, or 52 million people, who live in the most rural counties of America are spread across almost 2,500 counties that are heavily concentrated in the South and Midwest (Click here for a county level map). In contrast, the 20% of the nonelderly population (or 55 million people) who live in the most urban counties of America are spread across fewer than 70 counties that are heavily concentrated in the Northeast. Rurality varies widely by state (Figure 1 and Appendix Table 1). By the definition used in this brief, states such as Montana, North Dakota, and Wyoming are entirely rural, whereas states such as Connecticut, New York, and the District of Columbia have little to no rural area. In 11 states, more than half of the nonelderly population resides in a rural area (Montana, North Dakota, Wyoming, South Dakota, Vermont, New Mexico, Mississippi, Alaska, Iowa, Idaho, and Arkansas).
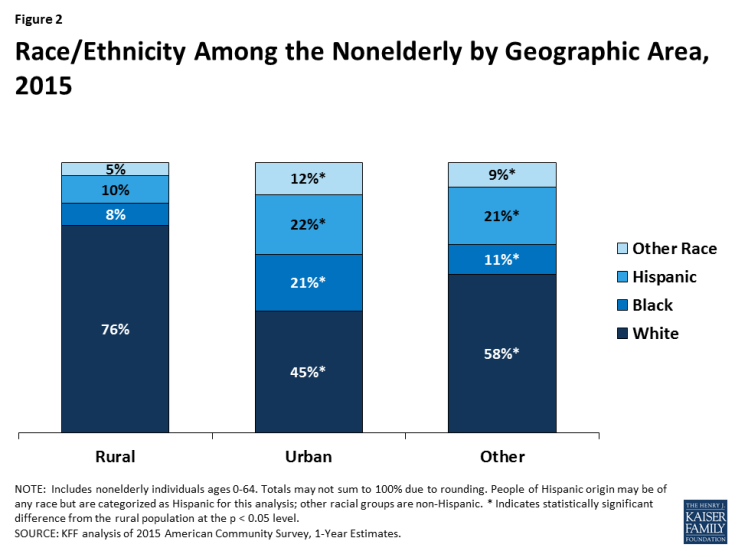
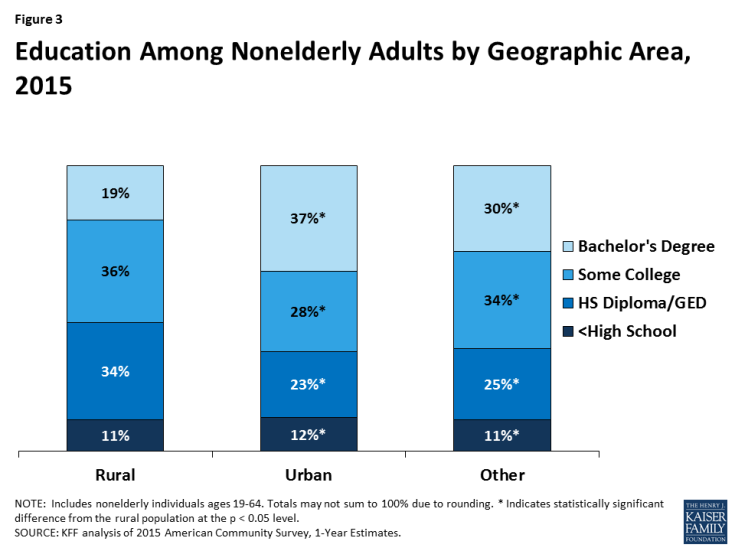
People living in rural areas are more likely to be older, White, and have lower levels of education compared to people living in other areas. A greater share of people living in rural areas are ages 65 and older than in urban and other areas (data not shown);1 however, there are not large differences in the age distribution of nonelderly individuals living in rural areas compared to those in urban and other areas (Appendix Table 2). Fewer than one quarter of individuals living in rural areas are people of color, compared to over half of people living in urban areas and four in ten people living in other areas (Figure 2). Similar to other areas of the US, nearly nine in ten people living in rural areas have at least a high school diploma or GED. However, fewer than two in ten people in rural areas have a Bachelor’s degree or higher, compared to nearly four in ten people in urban areas and three and ten people living in other areas of the US (Figure 3).
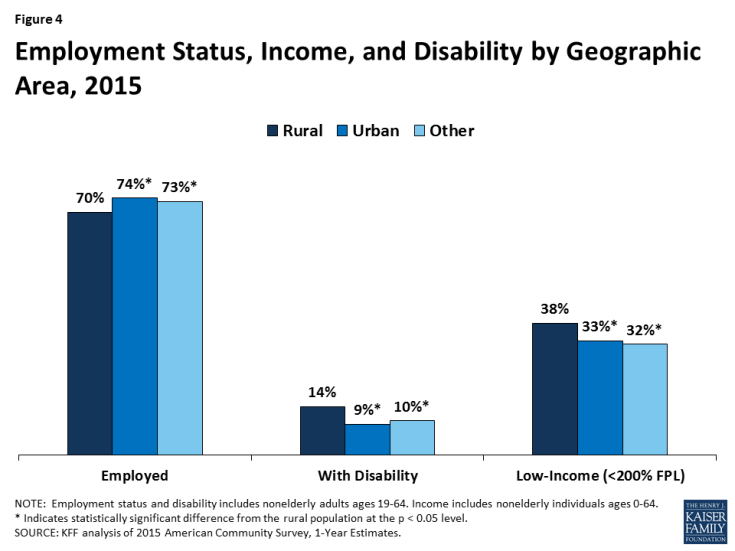
People living in rural areas are less likely to be in the labor force, more likely to have a disability, and more likely to be low-income than people living in other areas (Figure 4). A smaller share of nonelderly adults in rural areas are working than in urban and other areas (70% vs. 74% and 73%, respectively). Further, nonelderly adults living in rural areas are significantly more likely to have a disability (14%) than those in urban and other areas (9% and 10%, respectively; Figure 4). Reflecting their lower employment rate, nonelderly individuals living in rural areas are more likely than those in other areas to be low-income (below 200% of the federal poverty level or $40,320 per year for a family of three in 2017).
Rural populations face longstanding and significant disparities in their health and access to health care. Previous research has shown that rural residents are more likely to report poorer physical and mental health and have higher rates of cigarette smoking, obesity, and physical inactivity compared to their urban counterparts.2 In addition, people living in rural areas face significant barriers to accessing care, including provider shortages, recent closures of rural hospitals, and high travel distances to providers.3
What role does Medicaid play in rural America?
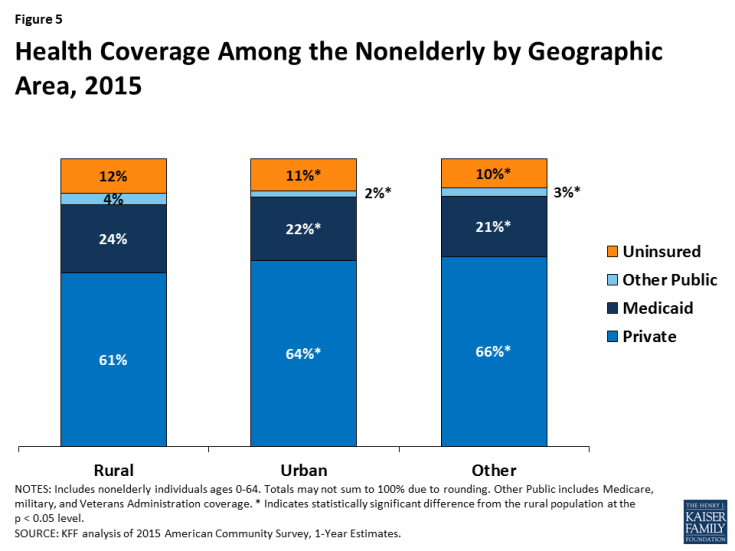
Medicaid plays a central role helping to fill gaps in private coverage in rural areas. Private insurance accounts for the largest share of health coverage among individuals in rural areas. However, nonelderly individuals in rural areas have a lower rate of private coverage compared to those in urban and other areas, reflecting greater employment in jobs that do not offer employer-sponsored health insurance4 and the lower labor force participation rate in rural areas (Figure 5). Medicaid helps fill this gap in private coverage, covering nearly one in four (24%) nonelderly individuals in rural areas, compared to 22% in urban areas and 21% in other areas. However, Medicaid coverage does not fully offset the gap in private coverage. As such, rural areas have a slightly higher nonelderly uninsured rate (12%) compared to urban (11%) and other areas (10%).
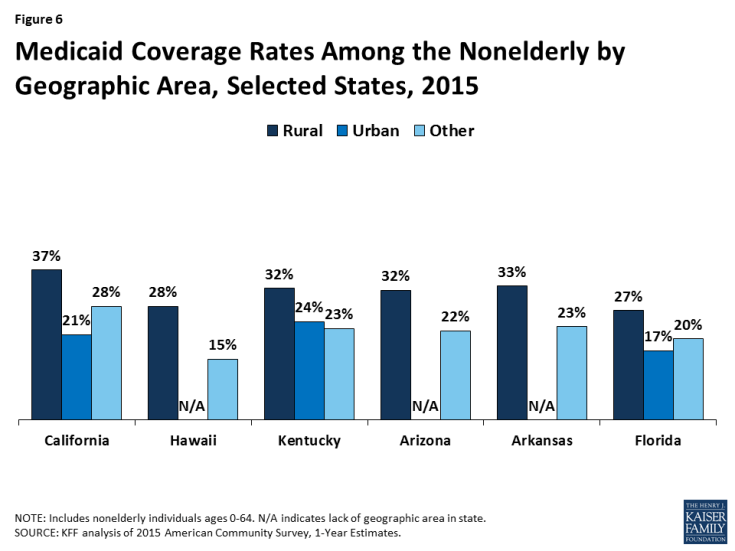
Within states, Medicaid generally plays a larger role in rural areas of the state compared to other areas. Medicaid coverage rates are higher in rural areas than in urban areas in 12 of the 19 states with both rural and urban areas (Appendix Table 3). Similarly, rural areas have a higher Medicaid coverage rate than other areas in 41 of the 43 states with both rural and other areas. In some states, the Medicaid coverage rate in rural areas is much higher than other areas. Figure 6 shows the six states with the largest differences in Medicaid coverage rates between rural and urban or other areas. For example, in California, the Medicaid coverage rate in rural areas is 16 percentage points higher compared to urban areas and in Hawaii there is a 13 percentage point difference between Medicaid coverage in rural and other areas. Similarly, in Arizona, Arkansas, and Florida, rural areas have a Medicaid coverage rate that is about ten percentage points higher than urban or other areas or the state.
How did Medicaid coverage in rural areas change under the ACA?
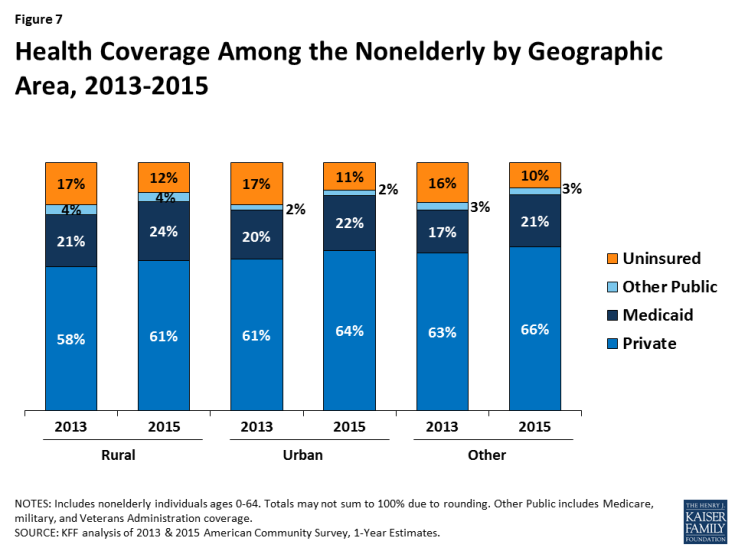
The share of people living in rural areas who are covered by Medicaid has grown under the ACA, corresponding with reductions in the uninsured rate. Rural areas experienced growth in Medicaid and private coverage that was similar to urban and other areas. In rural areas, the share of people with Medicaid and private coverage increased from 21% to 24% and 58% to 61% between 2013 and 2015, resulting in a decrease in the uninsured rate from 17% to 12%. Similarly, in urban and other areas, Medicaid and private coverage rates increased by 3 percentage points and uninsured rates decreased by 5 and 6 percentage points, respectively (Figure 7).
Rural areas in states that implemented the ACA Medicaid expansion to low-income adults experienced larger gains in coverage than those in non-expansion states. Prior to the ACA coverage expansion, which was implemented in 2014, rural areas in Medicaid expansion and non-expansion states had similar rates of Medicaid coverage. However, rural areas in non-expansion states had a lower rate of private coverage, which contributed to a higher uninsured rate for rural areas in non-expansion states (Figure 8). In rural areas, the Medicaid coverage rate in expansion states increased from 21% to 26% between 2013 and 2015, while it rose just one percentage point, from 20% to 21%, in non-expansion states. Reflecting the larger gains in Medicaid coverage in expansion states, the uninsured rate in rural areas within expansion states fell by nearly half from 16% to 9%. This reduction was nearly twice as large as the reduction in rural areas of non-expansion states. As a result, as of 2015, nonelderly individuals in rural areas within non-expansion states were nearly twice as likely to be uninsured as those within expansion states (15% vs. 9%).
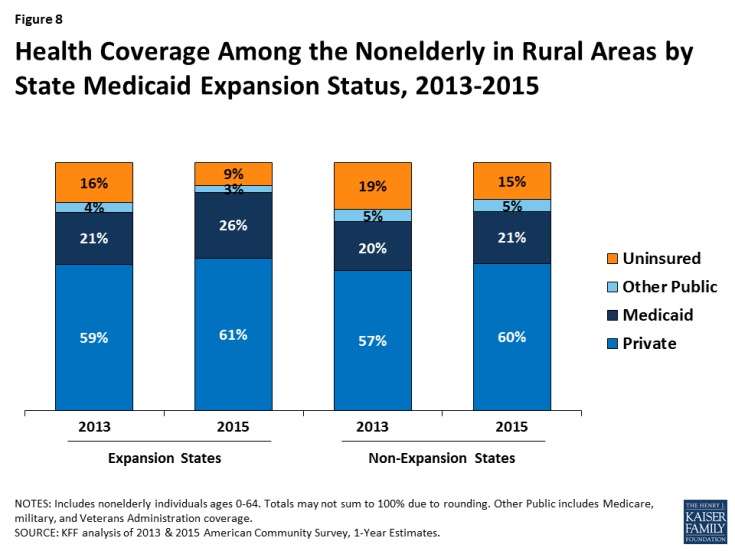
Figure 8: Health Coverage Among the Nonelderly in Rural Areas by State Medicaid Expansion Status, 2013-2015
Looking Ahead
These data illustrate that Medicaid plays a particularly important role in the most rural communities within our nation. This analysis shows that Medicaid helps fill gaps in private coverage within rural areas, helping to reduce disparities in coverage between rural areas and the rest of the nation. Medicaid coverage has grown in rural areas under the ACA, helping to reduce uninsured rates. However, states that expanded Medicaid experienced larger coverage gains than non-expansion states, leaving individuals in rural areas in non-expansion states nearly twice as likely to be uninsured as those in expansion states.
Further action among states to implement the ACA Medicaid expansion to low-income adults could lead to additional coverage gains in rural areas. As of April 2017, 19 states have not yet adopted the Medicaid expansion to low-income adults. These non-expansion states are home to 59% of nonelderly uninsured individuals living in rural areas. Additional action to expand Medicaid within these states would likely lead to increased coverage among individuals living in rural areas. In the four states (Kansas, Maine, North Carolina, and Virginia) that have had recent legislative activity related to implementing the expansion,5 nearly a quarter or more nonelderly individuals live in rural areas.
Reductions in Medicaid could disproportionately affect individuals living in rural America. If federal funding for Medicaid is reduced through elimination of enhanced funding for the ACA Medicaid expansion or limits on funding for the broader program, states would likely need to increase state spending to maintain coverage or make program cutbacks that would reduce eligibility, benefits, or provider payments. Given the larger role Medicaid plays for individuals in rural areas compared to other areas, individuals in these areas would likely be disproportionately impacted by coverage losses as well as reduced benefits and increased premiums and cost sharing. Further, analysis shows that high poverty states and states in the South, which include many rural areas, would be disproportionately impacted by reductions in federal Medicaid funds and face the highest increases in state spending to maintain coverage amid federal reductions. Reductions in Medicaid coverage would also increase demands on safety net providers, including community health centers and public hospitals. At the same time, the loss of federal Medicaid revenues would increase fiscal strains on these providers who already face a range of challenges that have contributed to increases in closures among rural hospitals in recent years.6
| Methods |
| This brief is based on analysis of American Community Survey (ACS) data from 2013-2015. In this brief, rural areas are defined using the 2010 Index of Relative Rurality (IRR) measure, which is a continuous measure of a county’s degree of rurality based on population size, population density, extent of urbanized area, and distance to the nearest metro area.7 For this analysis the IRR is divided into five equally weighted population quintiles based off ACS weighted data. County level data for ACS was obtained by using a public use microdata area (PUMA) code to county crosswalk based on the 2010 Census definition.8 Although the IRR determines the degree of a county’s rurality and not if a county is rural or urban, throughout this brief, the population quintile with the highest degree of rurality is referred to as “rural,” and the population quintile with the lowest degree of rurality is referred to as “urban.” The remaining three population quintiles are referred to as “other.” While the elderly population is included in the assignment of rurality, they are excluded from the remainder of the analysis, as our focus is Medicaid’s role as a health insurer for children and non-elderly adults. |