2016 Employer Health Benefits Survey
Section Seven: Employee Cost Sharing
In addition to any required premium contributions, most covered workers face cost sharing for the medical services they use. Cost sharing for medical services can take a variety of forms, including deductibles (an amount that must be paid before most services are covered by the plan), copayments (fixed dollar amounts), and/or coinsurance (a percentage of the charge for services). The type and level of cost sharing often vary by the type of plan in which the worker is enrolled. Cost sharing may also vary by the type of service, such as office visits, hospitalizations, or prescription drugs.
The cost-sharing amounts reported here are for covered workers using services provided in-network by participating providers. Plan enrollees receiving services from providers that do not participate in plan networks often face higher cost sharing and may be responsible for charges that exceed plan allowable amounts. The framework of this survey does not allow us to capture all of the complex cost-sharing requirements in modern plans, particularly for ancillary services (such as durable medical equipment or physical therapy) or cost-sharing arrangements that vary across different settings (such as tiered networks). Therefore, we do not collect information on all plan provisions and limits that affect enrollee out-of-pocket liability.
General Annual Deductibles For Workers in Plans with Deductibles
- A general annual deductible is an amount that must be paid by enrollees before most services are covered by their health plan. Non-grandfathered health plans are required to cover some services such as preventive care without cost sharing. Some plans require enrollees to meet a service-specific deductible such as on prescription drugs or hospital admissions in lieu of or in addition to a general deductible.
- Eighty-three percent of covered workers are enrolled in a plan with a general annual deductible for single coverage, similar to 81% in 2015. Since 2011, the percentage of covered workers with a general annual deductible for single coverage has increased from 74% to 83% (Exhibit 7.2).
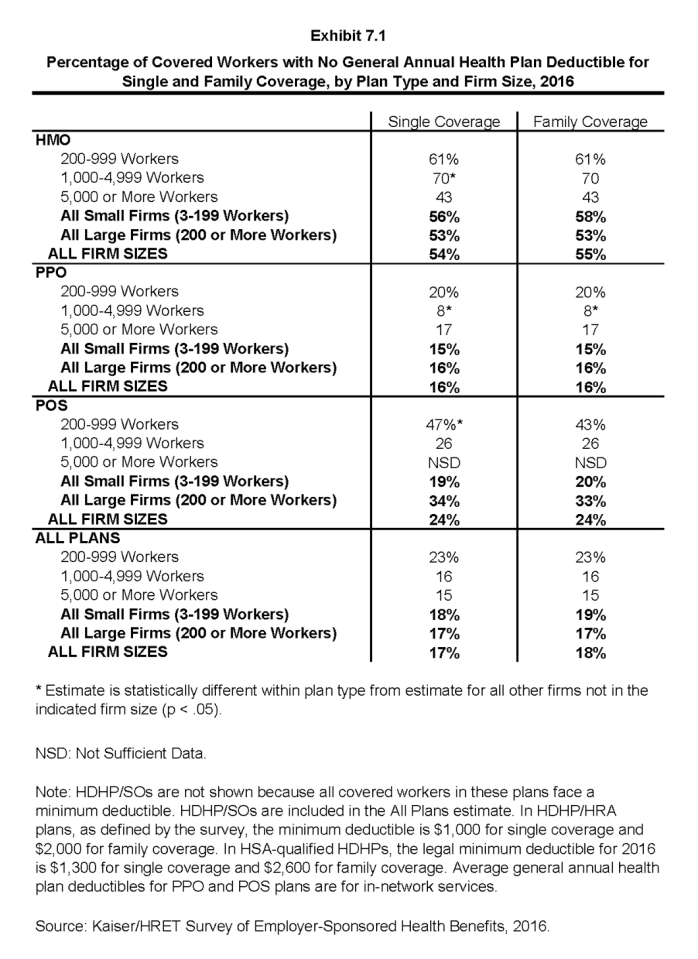
- The percentage of covered workers enrolled in a plan with a general annual deductible for single coverage is similar for small firms (3-199 workers) and large firms (200 0r more workers) (82% and 83%) (Exhibit 7.1).
- The likelihood of having a deductible varies by plan type. Covered workers in HMOs are less likely to have a general annual deductible for single coverage than workers in other plan types. Fifty-four percent of workers in HMOs do not have a general annual deductible for single coverage, compared to 24% of workers in POS plans and 16% of workers in PPOs (Exhibit 7.1). The percentage of covered workers in HMO plans with a general annual deductible for single coverage has increased from 29% in 2011 to 46% in 2016 (Exhibit 7.2).
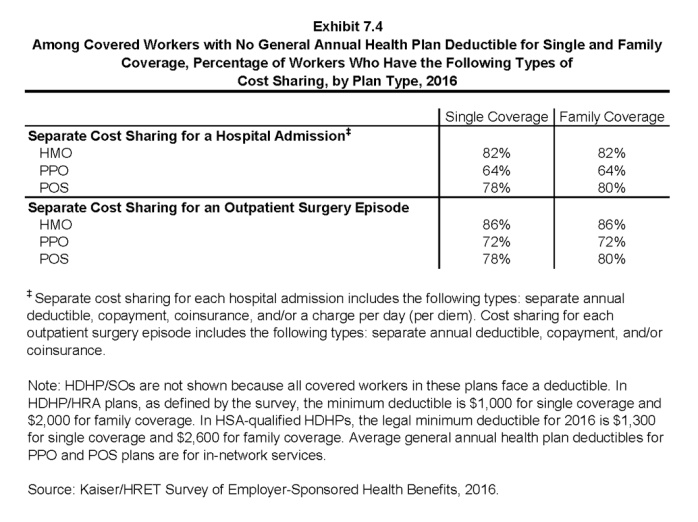
- Covered workers in plans without a general annual deductible often have other forms of cost sharing when they are hospitalized or use other medical services. For covered workers in plans without a general annual deductible with single coverage, 82% in HMOs, 64% in PPOs, and 78% in POS plans are in plans that require some cost sharing for hospital admissions. The percentages are similar for family coverage (Exhibit 7.4).
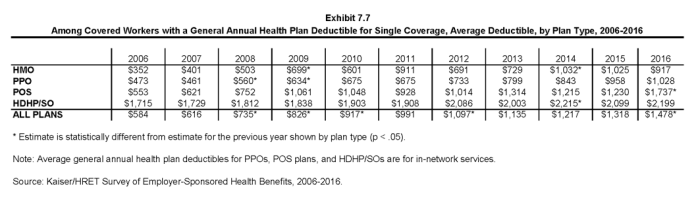
- For covered workers in a plan with a general annual deductible, the average annual deductible for single coverage is $1,478, an increase over the average deductible ($1,318) last year (Exhibit 7.7).
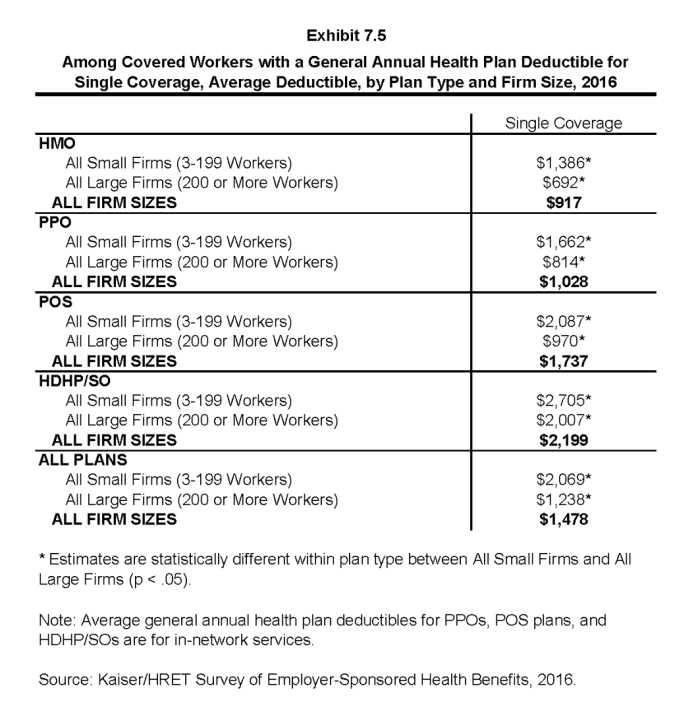
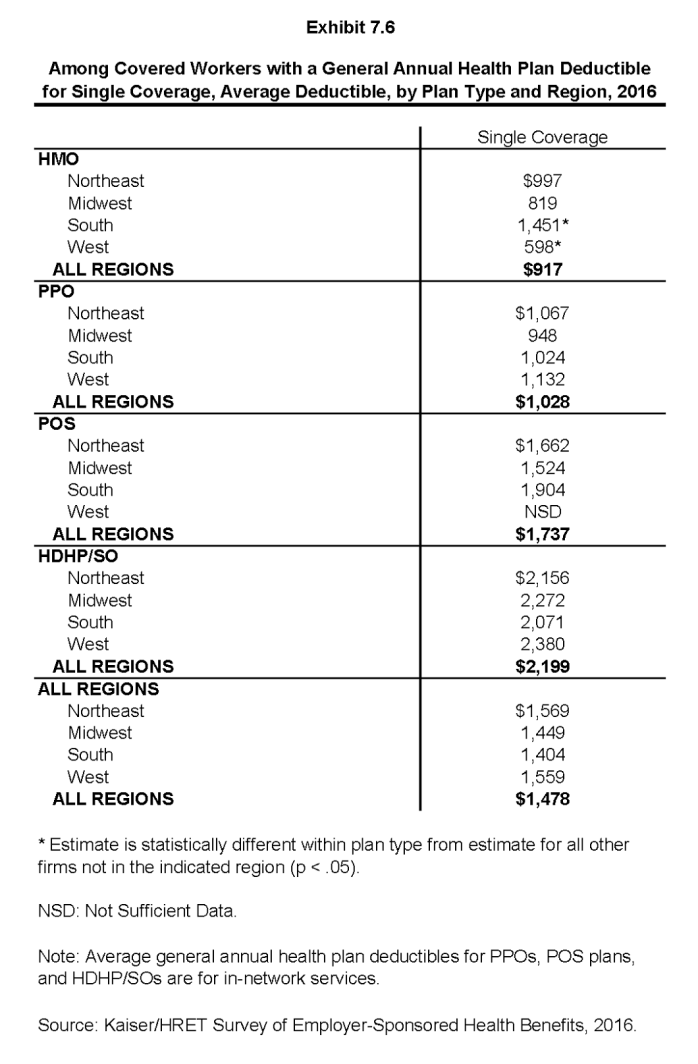
- Average deductibles vary considerably by plan type. For covered workers in plans with a general annual deductible, the average deductibles for single coverage are $917 in HMOs, $1,028 in PPOs, $1,737 in POS plans, and $2,199 for HDHP/SOs (Exhibit 7.5).
- Deductibles for single coverage are generally higher for covered workers in small firms than for covered workers in large firms across plan types. For example, for covered workers in PPOs with a general annual deductible, the average deductible amount for single coverage in small firms is more than twice as large as the average deductible amount in large firms ($1,662 vs. $814). Overall, for covered workers in plans with a general annual deductible, the average deductible amount for single coverage in small firms is higher than the average deductible amount in large firms ($2,069 vs. $1,238) (Exhibit 7.5).
- The average general annual deductible for single coverage for covered workers in plans with a deductible has increased 49% over the last five years, from $991 in 2011 to $1,478 in 2016 (Exhibit 7.7).
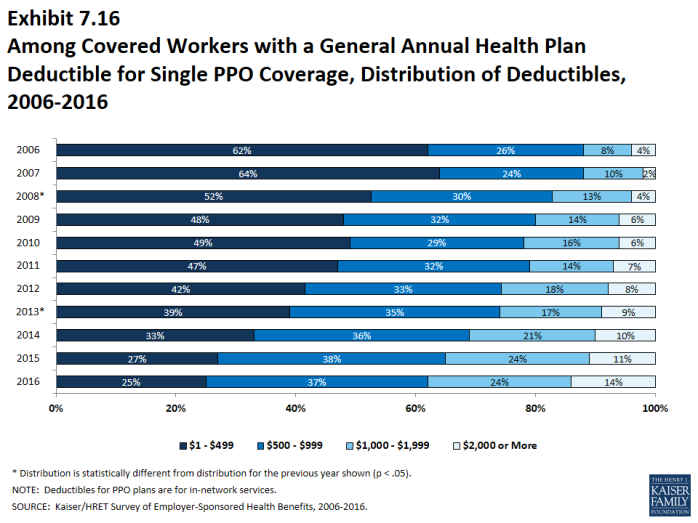
- There is considerable variation in the dollar values of general annual deductibles for covered workers at different firms. For example, 25% of covered workers enrolled in a PPO plan with a general annual deductible for single coverage have a deductible of less than $500 while 14% have a deductible of $2,000 or more (Exhibit 7.16).
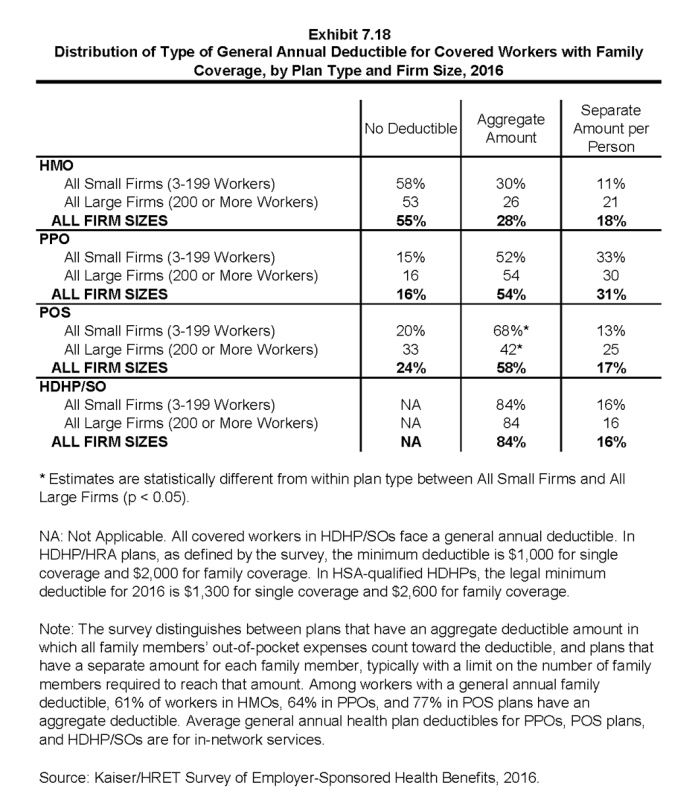
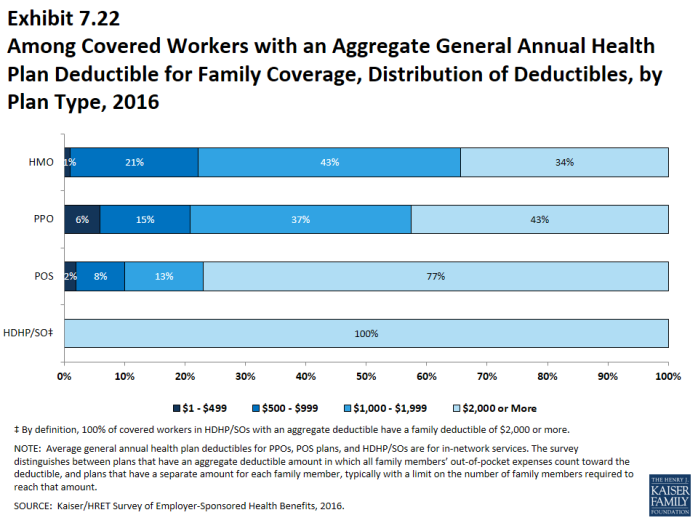
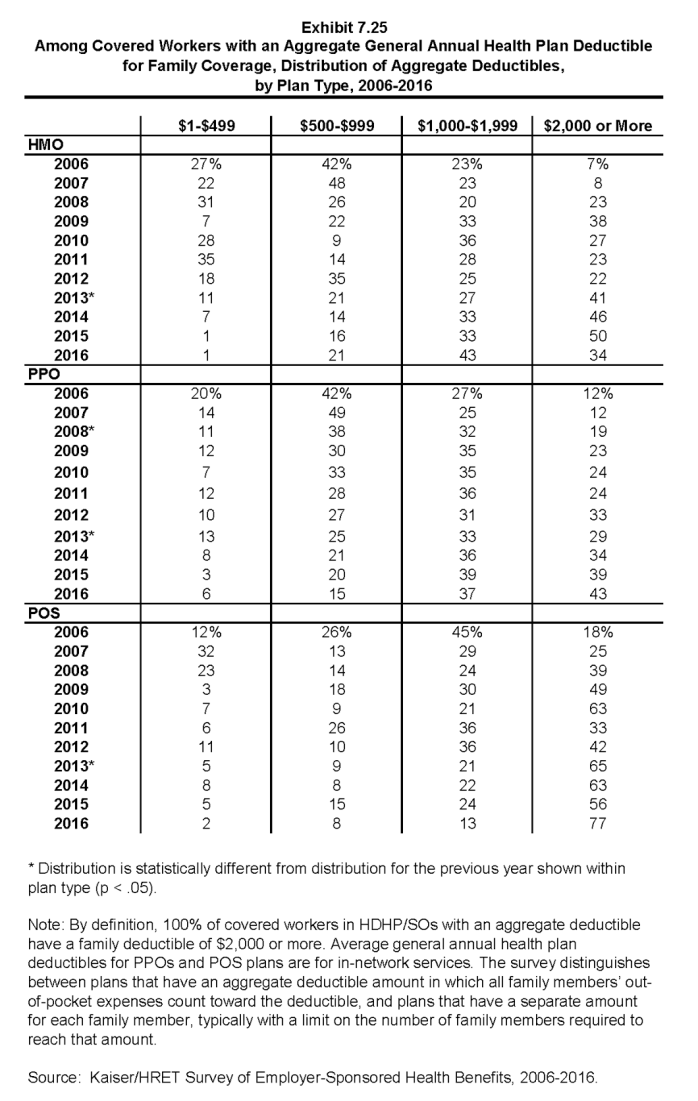
- For family coverage, the majority of covered workers with general annual deductibles have an aggregate deductible, meaning all family members’ out-of-pocket expenses count toward meeting the deductible amount. Among those with a general annual deductible for family coverage, the percentages of covered workers with an average aggregate general annual deductible are 61% for workers in HMOs, 64% for workers in PPOs, and 77% for workers in POS plans (Exhibit 7.18).
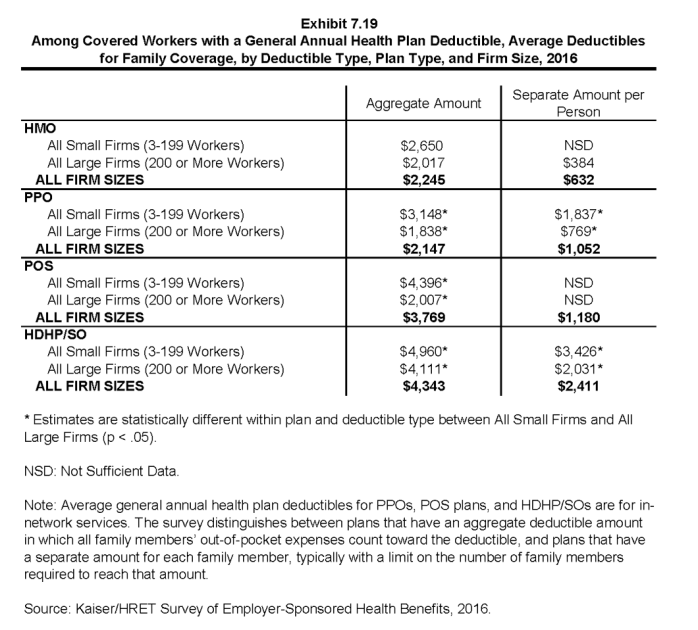
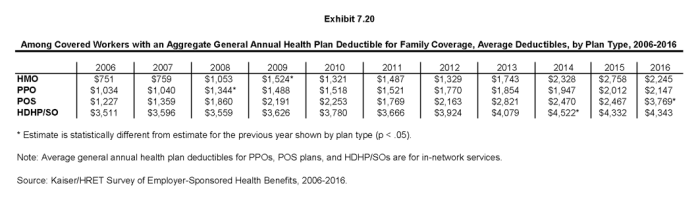
- The average deductible amounts for covered workers with an aggregate deductible for family coverage are $2,245 for HMOs, $2,147 for PPOs, $3,769 for POS plans, and $4,343 for HDHP/SOs (Exhibit 7.19). Deductible amounts for aggregate family deductibles are similar to last year for plan types other than POS plans (Exhibit 7.20).
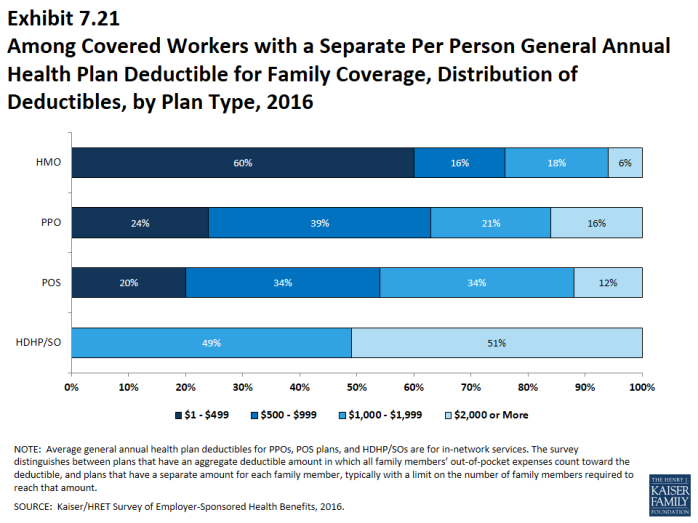
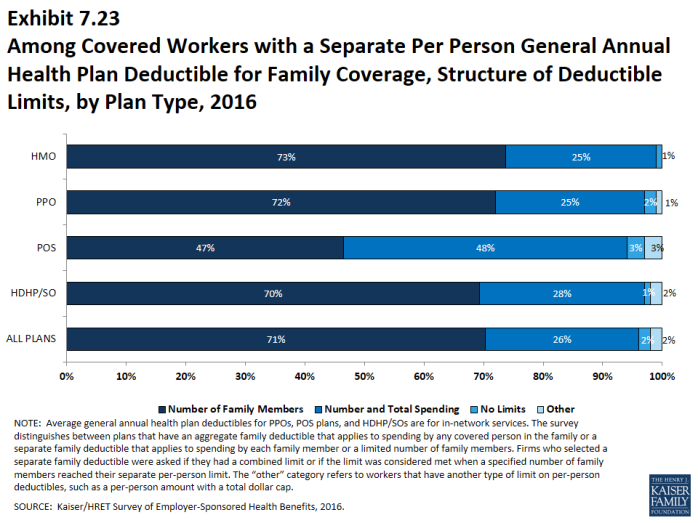
- The other type of family deductible, a separate per-person deductible, requires each family member to meet a separate per-person deductible amount before the plan covers expenses for that member. Many plans with separate per-person family deductibles (71%) consider the deductible met for all family members if a prescribed number of family members each reaches his or her separate deductible amounts (Exhibit 7.23). Plans may also require each family member to meet a separate per-person deductible until the family’s combined spending reaches a specified dollar amount.
- For covered workers in health plans that have separate per-person general annual deductible amounts for family coverage, the average deductibles are $632 for HMOs, $1,052 for PPOs, $1,180 for POS plans, and $2,411 for HDHP/SOs (Exhibit 7.19).
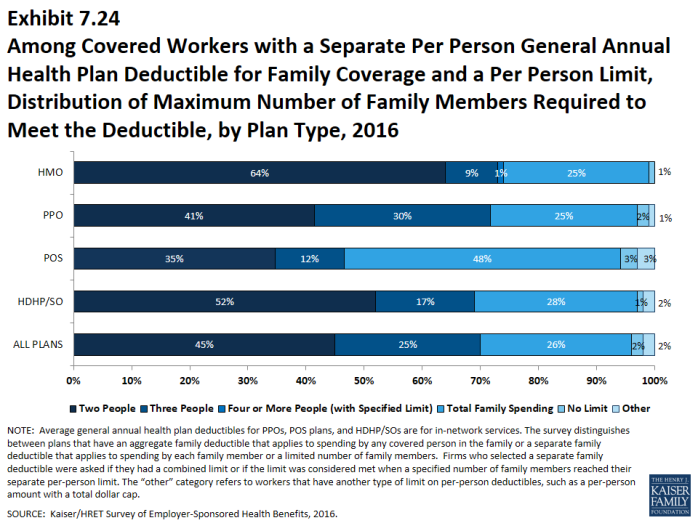
- Most covered workers in plans with a separate per-person general annual deductible for family coverage have a limit to the number of family members required to meet the separate deductible amounts (Exhibit 7.23).1 Among those covered workers in plans with a limit on the number of family members, the most frequent number of family members required to meet the separate deductible amounts is two (45%) (Exhibit 7.24).
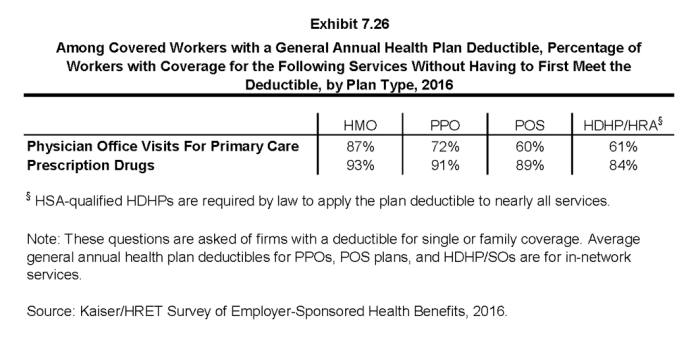
- The majority of covered workers with a general annual deductible are in plans where the deductible does not have to be met before certain services, such as physician office visits or prescription drugs, are covered.
- Large majorities of covered workers (87% in HMOs, 72% in PPOs, and 60% in POS plans) with general annual deductibles are enrolled in plans where the deductible does not have to be met before physician office visits for primary care are covered (Exhibit 7.26).
- Similarly, among workers with a general annual deductible, large shares of covered workers in HMOs (93%), PPOs (91%), and POS plans (89%) are enrolled in plans where the general annual deductible does not have to be met before prescription drugs are covered (Exhibit 7.26).
General Annual Deductibles Among All Covered Workers
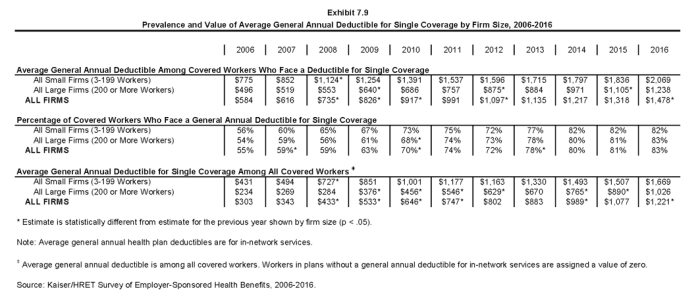
- As discussed above, the share of covered workers in plans with a general annual deductible has increased significantly over time: from 55% in 2006, to 74% in 2011, to 83% in 2016, as have the average deductible amounts for covered workers in plans with deductibles: from $584 in 2006, to $991 in 2011, to $1,478 in 2016. Neither trend by itself captures the full impact of changes in deductibles on covered workers. We can look at the average impact of both trends together on covered workers by assigning a zero deductible value to covered workers in plans with no deductible and looking at how the resulting averages change over time. These average deductible amounts are lower in any given year but the changes over time reflect both the higher deductibles in plans with deductibles and the fact that more workers face them.
- Using this approach, the average general annual deductible for single coverage for all covered workers in 2016 is $1,221 (Exhibit 7.9).
- The 2016 value is 63% higher than the average general annual deductible of $747 in 2011 and 300% higher than the average general annual deductible of $303 in 2006 (Exhibit 7.9).
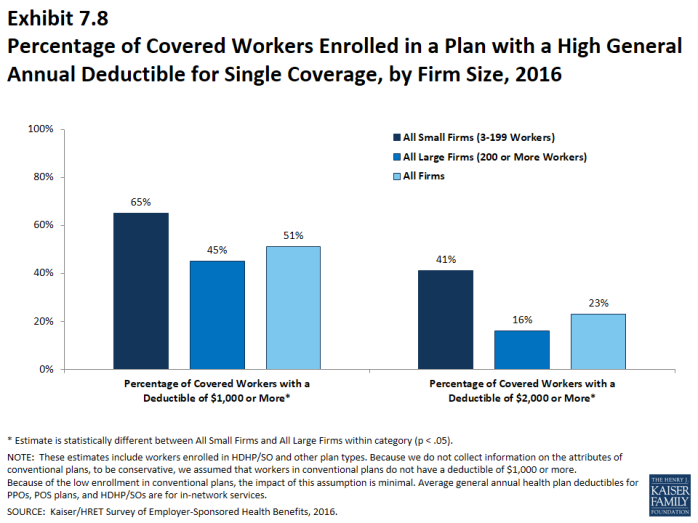
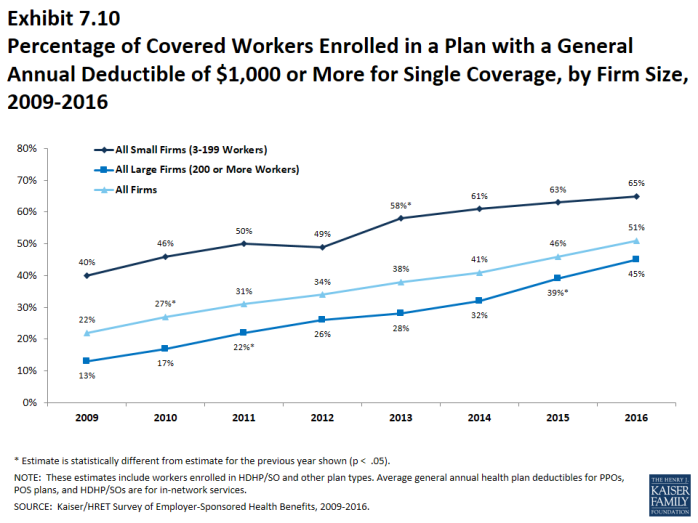
- Another way to look at deductibles is the percentage of all covered workers who are in a plan with a deductible that exceeds certain thresholds. Fifty-one percent of covered workers are in plans with a general annual deductible of $1,000 or more for single coverage, similar to the percentage in 2015 (46%) (Exhibit 7.10).
- Over the last five years, the percentage of covered workers with a general annual deductible of $1,000 or more for single coverage has grown substantially, increasing from 31% to 51% (Exhibit 7.10).
- Workers in small firms are more likely to have a general annual deductible of $1,000 or more for single coverage than workers in large firms (65%vs. 45%) (Exhibit 7.8).
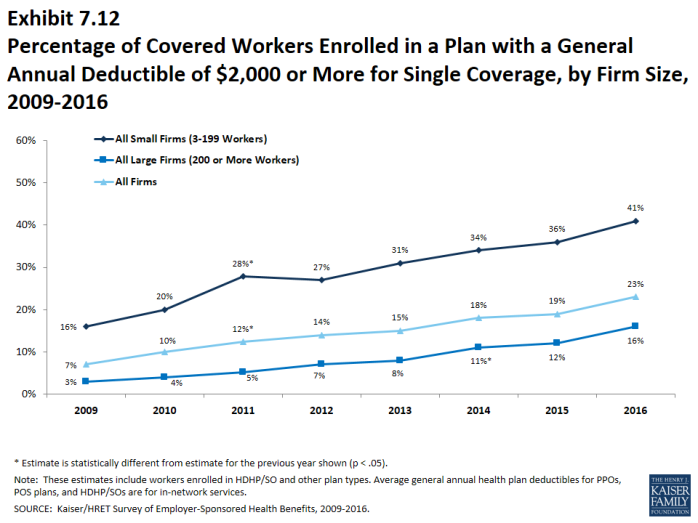
- Twenty-three percent of covered workers are enrolled in a plan with a deductible of $2,000 or more, similar to the percentage last year (19%) (Exhibit 7.12). Forty-one percent of covered workers at small firms have a general annual deductible of $2,000 or more, in contrast to 16% in large firms (Exhibit 7.8).
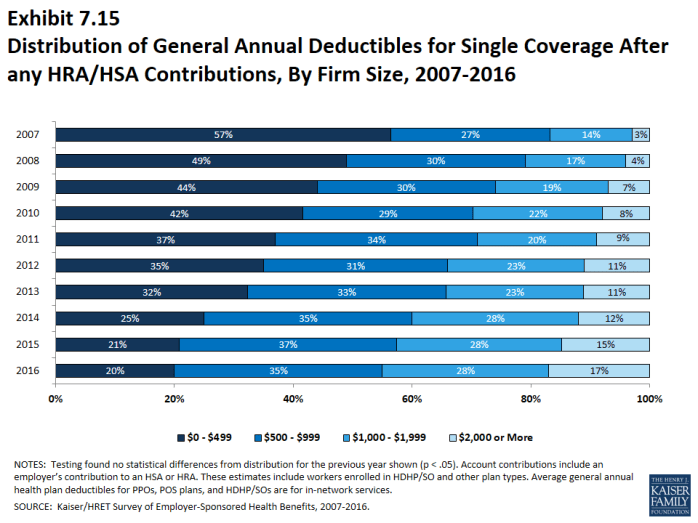
- One of the reasons for the growth in deductible amounts has been the growth in enrollment in HDHP/SOs, which have higher deductibles than other plans. While growing deductibles in PPOs and other plan types generally increases enrollee out-of-pocket liability, the shift in enrollment to HDHP/SOs does not necessarily do so because most HDHP/SO enrollees receive an account contribution from their employers, which in essence reduces the high cost sharing in these plans.
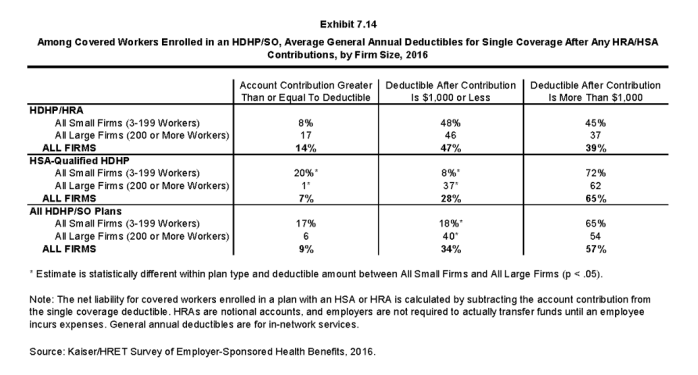
- Fourteen percent of covered workers in an HDHP with an HRA and 7% of covered workers in an HSA-qualified HDHP receive an account contribution for single coverage at least equal to their deductible, while another 47% of covered workers in an HDHP with an HRA and 28% of covered workers in an HSA-qualified HDHP receive account contributions that, if applied to their deductible, would reduce the deductible to $1,000 or less (Exhibit 7.14).
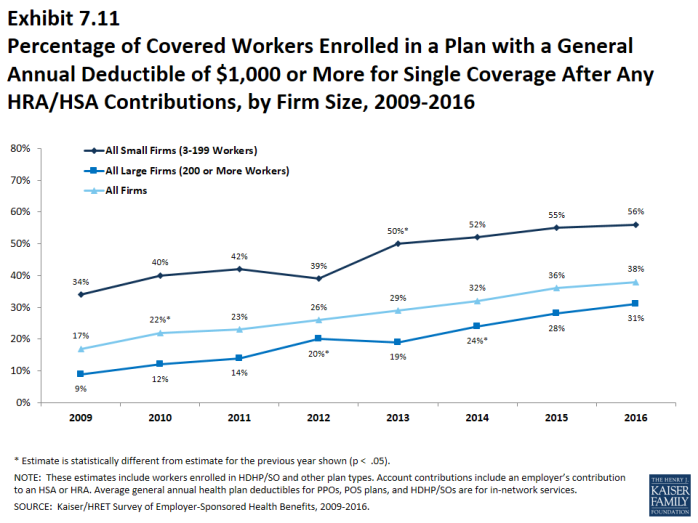
- If we reduce the deductibles that workers face by employer account contributions, the percentage of covered workers with a deductible liability of $1,000 or more would be reduced from 51% to 38% (Exhibit 7.11).
Hospital and Outpatient Surgery Cost Sharing
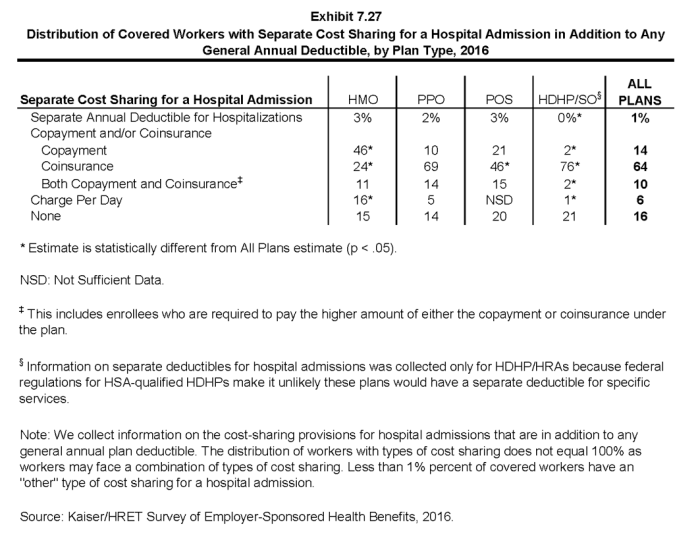
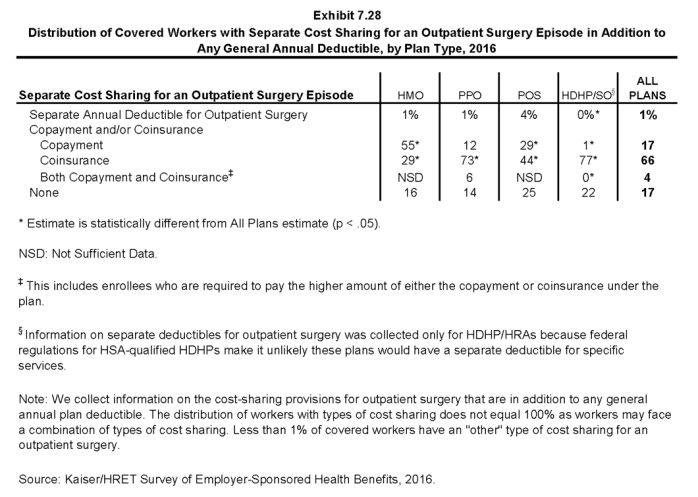
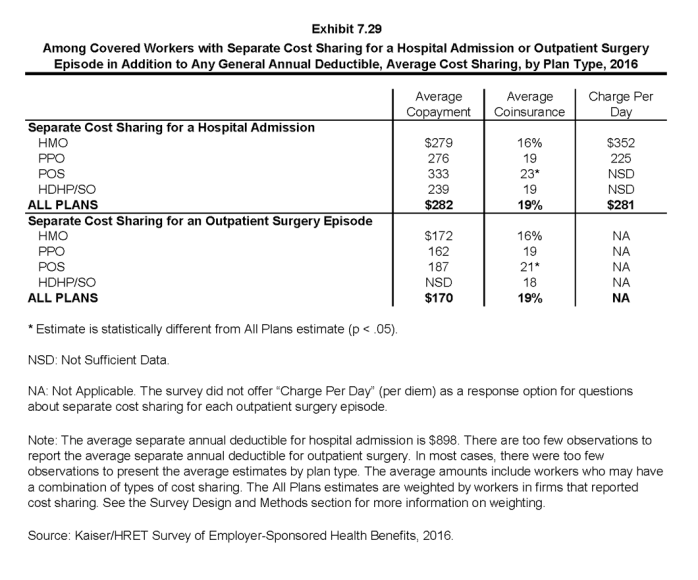
- Whether or not a worker has a general annual deductible, most workers face additional types of cost sharing (such as a copayment, coinsurance, or a per diem charge) when admitted to a hospital or having outpatient surgery. The distribution of workers with cost sharing for hospital and outpatient surgery does not equal 100% as workers may face a combination of types of cost sharing. In addition, the average copayment and coinsurance rates for hospital admissions include workers who may have a combination of these types of cost sharing.
- For hospital admissions, 64% of covered workers have coinsurance and 14% have copayments. Lower percentages of workers have per day (per diem) payments (6%), a separate hospital deductible (1%), or both copayments and coinsurance (10%), while 16% have no additional cost sharing for hospital admissions after any general annual deductible has been met. For covered workers in HMO plans, copayments are more common (46%) and coinsurance (24%) is less common than in other plan types. Only 2% of covered workers in HDHP/SOs have a copayment for hospital admissions, lower than other plan types (Exhibit 7.27).
- The percentage of covered workers in a plan that requires coinsurance for hospital admissions has increased from 55% in 2011 to 64% in 2015.
- The average coinsurance rate for hospital admission is 19%; the average copayment is $282 per hospital admission; the average per diem charge is $281; and the average separate annual hospital deductible is $898 (Exhibit 7.29).
- The cost-sharing provisions for outpatient surgery are similar to those for hospital admissions, as most workers have coinsurance or copayments. Sixty-six percent of covered workers have coinsurance and 17% have copayments for an outpatient surgery episode. In addition, 1% has a separate annual deductible for outpatient surgery, and 4% have both copayments and coinsurance, while 17% have no additional cost sharing after any general annual deductible has been met (Exhibit 7.28).
- For covered workers with cost sharing for outpatient surgery, the average coinsurance rate is 19% and the average copayment is $170 (Exhibit 7.29).
Cost Sharing for Physician Office Visits
- The majority of covered workers are enrolled in health plans that require cost sharing for an in-network physician office visit, in addition to any general annual deductible2.
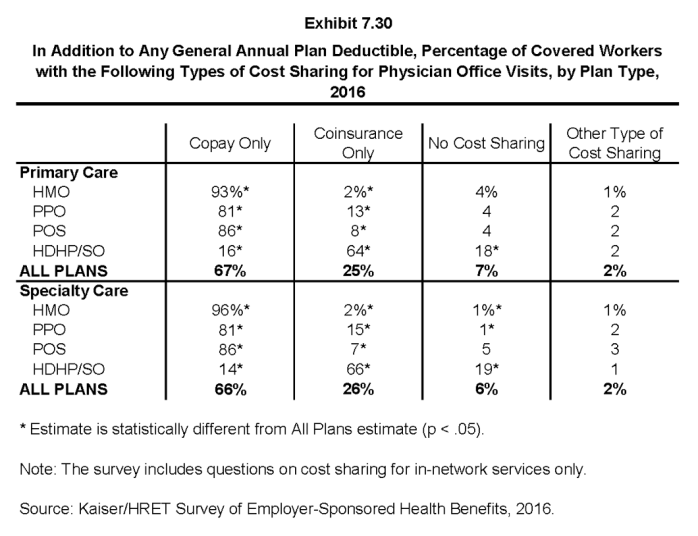
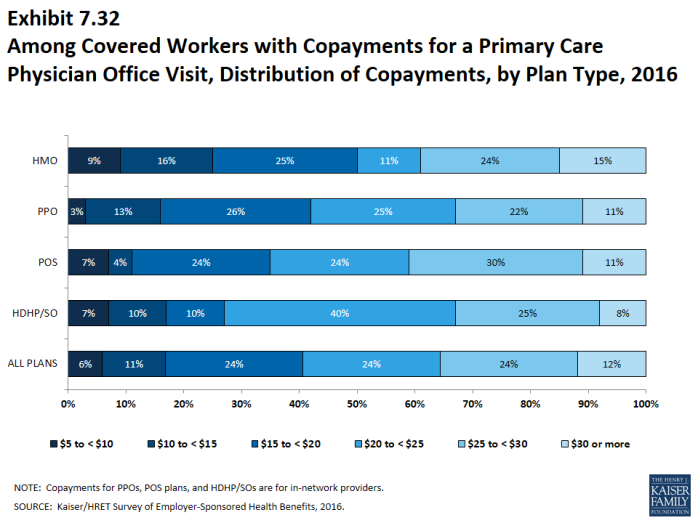
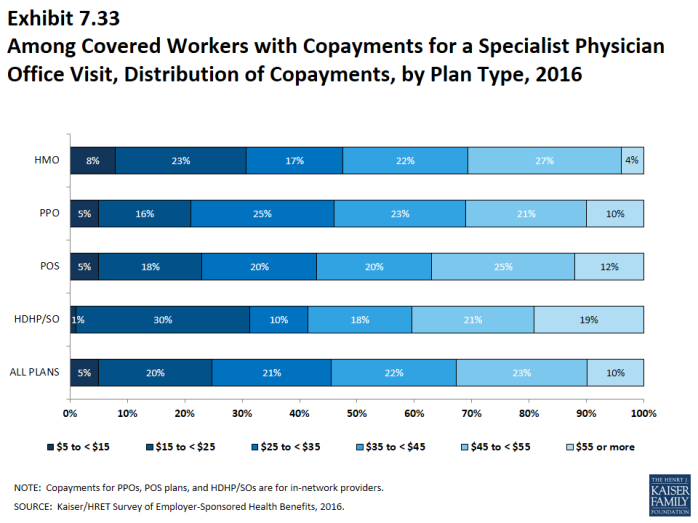
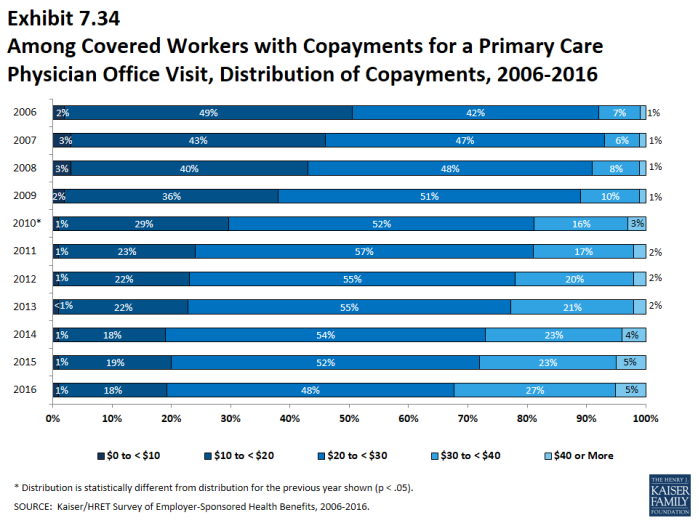
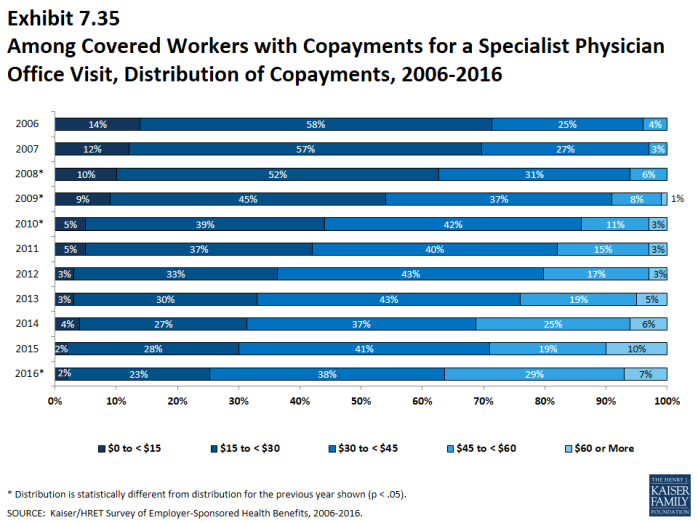
- The most common form of physician office visit cost sharing for in-network services is copayments. Sixty-seven percent of covered workers have a copayment for a primary care physician office visit and 25% have coinsurance. For office visits with a specialty physician, 66% of covered workers have copayments and 26% have coinsurance. Workers in HMOs, PPOs, and POS plans are much more likely to have copayments than workers in HDHP/SOs for both primary care and specialty care physician office visits. For primary care physician office visits, 64% of covered workers in HDHP/SOs have coinsurance, 18% have no cost sharing after the general annual plan deductible is met, and 16% have copayments (Exhibit 7.30).
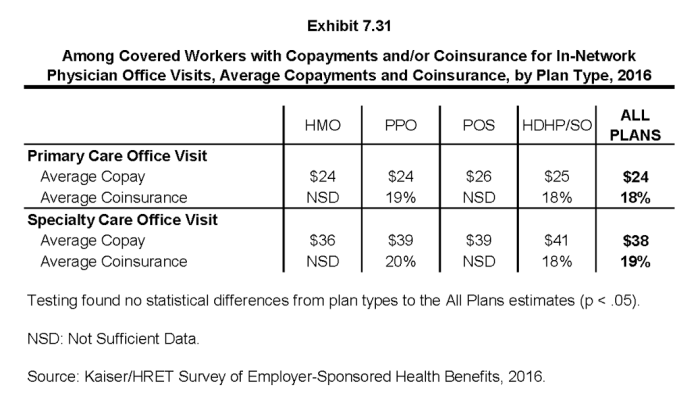
- Among covered workers with a copayment for in-network physician office visits, the average copayment is $24 for primary care and $38 for specialty physician office visits (Exhibit 7.31), similar to the amounts last year (Exhibit 7.31).
- Among workers with coinsurance for in-network physician office visits, the average coinsurance rates are 18% for a visit with a primary care physician and 19% for a visit with a specialist (Exhibit 7.31), the same rates as last year.
Out-Of-Pocket Maximum Amounts
- Most covered workers are in a plan that partially or totally limits the cost sharing that a plan enrollee must pay in a year. These limits are generally referred to as out-of-pocket maximum amounts. The Affordable Care Act (ACA) requires that non-grandfathered health plans have an out-of-pocket maximum of $6,850 or less for single coverage and $13,700 for family coverage.3 Many plans have complex out-of-pocket structures, which makes it difficult to accurately collect information on this element of plan design.
- In 2016, 98% percent of covered workers are in a plan with an out-of-pocket maximum for single coverage. This is a significant increase from 83% in 2011.
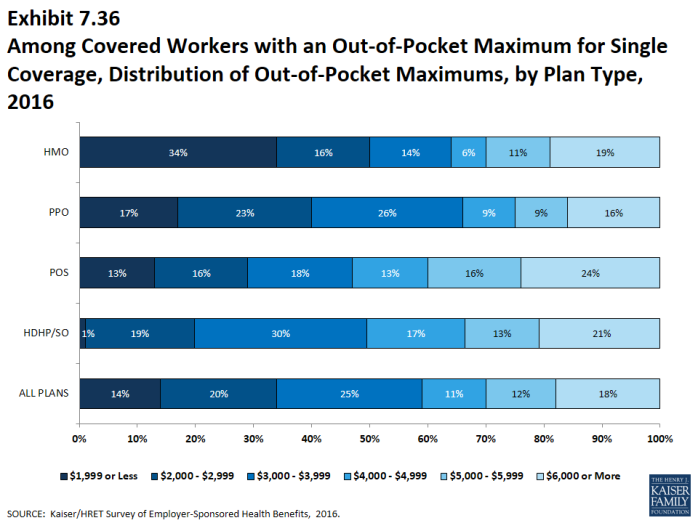
- For covered workers in plans with out-of-pocket maximums for single coverage, there is wide variation in spending limits.
- Fourteen percent of covered workers in plans with an out-of-pocket maximum for single coverage have an out-of-pocket maximum of less than $2,000, while 18% have an out-of-pocket maximum of $6,000 or more (Exhibit 7.36).