How Are Hospitals Faring Under the Affordable Care Act? Early Experiences from Ascension Health
Expanded health insurance coverage through the Affordable Care Act (ACA) is having a major impact on many of the nation’s hospitals through increases in the demand for care, increased patient revenues, and lower uncompensated care costs for the uninsured. In anticipation of higher revenues from patient care, the ACA calls for reductions in Medicaid Disproportionate Share Hospital (DSH) payments that support hospitals that serve a large number of Medicaid and uninsured patients to help cover the costs of uncompensated care. DSH cuts were scheduled to begin in 2014 but were delayed to FY2018. While many people are focusing on how these changes affect public hospitals and large urban safety net systems, many not-for-profit hospitals that have a strong tradition and mission of caring for underserved populations also may be affected. The size of the impact on specific hospitals will depend, among other factors, on whether hospitals are located in states that expanded Medicaid coverage through the ACA.
This report examines the early experiences with the ACA by Ascension Health, the delivery subsidiary of the nation’s largest not-for-profit health system, Ascension, which includes 131 acute-care hospitals and more than 30 senior care facilities in 23 states and the District of Columbia. Ascension is a Catholic healthcare system with service to the poor as an explicit part of their mission, providing almost $1.8 billion in care to persons living in poverty and other community benefit programs that include $600 million in direct charity care assistance to poor and uninsured patients in their 2014 fiscal year. The analysis examines changes in discharge volumes, hospital finances, and other outcomes between the last three quarters of 2013 – just before implementation of the ACA coverage expansions – and the first three quarters of 2014 (through September 30, 2014). In addition, the analysis compares changes among hospitals in states that expanded Medicaid with hospitals in states that did not expand Medicaid. Key findings include:
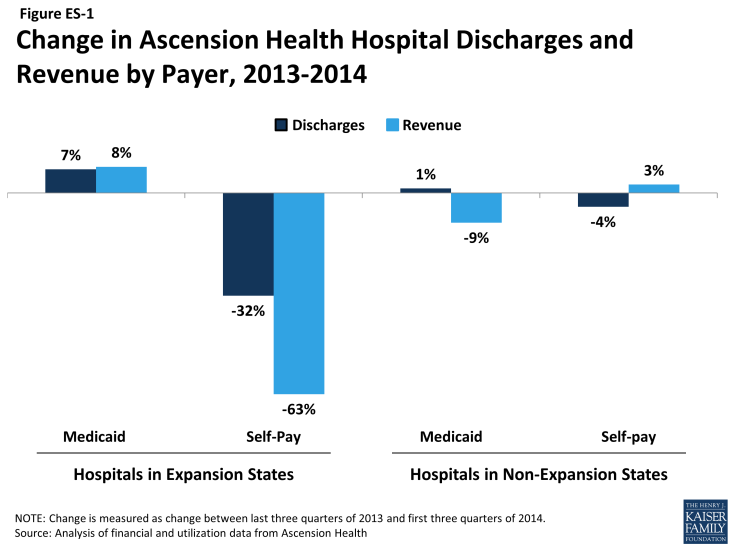
- Compared to hospitals in states that did not expand Medicaid, Ascension Health hospitals in states that expanded Medicaid experienced larger increases in Medicaid discharge volumes and decreases in uninsured/self-pay volume from 2013 to 2014 (see Figure ES-1). Specifically, hospitals in Medicaid expansion states saw a 7.4 percent increase in Medicaid discharge volumes from 2013 to 2014 (compared to 1.4 percent for hospitals in non-expansion states) and a 32.3 percent decrease in uninsured/self-pay discharge volumes (compared to a 4.4 percent decrease in non-expansion states). Correspondingly, Ascension hospitals in expansion states saw an increase in the share of total discharges billed to Medicaid and a decrease in the share of discharges that were uninsured/self-pay.
- Looking at total revenue, Ascension hospitals in expansion states saw an increase (8.2 percent) in Medicaid revenue from 2013 to 2014 and a 63.2 percent decrease in revenue from self-pay (Figure ES-1). Hospitals in non-expansion states actually saw a 9.4 percent decline in Medicaid revenue over the same period and a slight increase (2.6 percent) in revenue from self-pay. Growth in Medicaid revenue from outpatient care outpaced increases in inpatient revenue in expansion states, suggesting that these hospitals experienced greater increases in demand for outpatient care from new Medicaid patients compared to inpatient care.
- Despite somewhat smaller increases in patient revenue, hospitals in expansion states had larger relative increases in operating margins from 2013 to 2014 compared to hospitals in non-expansion states. Operating margins among hospitals in Medicaid expansion states increased from 2.1 percent in 2013 to 3.4 percent in 2014. Operating margins also increased among hospitals in non-expansion states, but the relative increase was smaller compared to hospitals in expansion states. The increase in operating margins in expansion states was due largely to almost zero growth in the costs of providing health care.
- Looking at particular cost items, charity care costs decreased 40.1 percent among hospitals in Medicaid expansion states compared to 6.2 percent in non-expansion states. However, another component of cost of care to the poor, Medicaid shortfalls – the difference between what Medicaid pays and the costs of treating Medicaid patients – increased 31.9 percent between 2013 and 2014. Shortfalls increased for hospitals in expansion states but were more than offset by increases in Medicaid revenue. Shortfalls increased more among hospitals in non-expansion states than expansion states and were not offset by increases in Medicaid revenue, possibly due to state cuts in provider reimbursement. Combining the decrease in charity care costs with the increase in Medicaid shortfalls, the net cost of caring for low income patients decreased among hospitals in expansion states, while these costs increased among hospitals in non-expansion states.
Overall, hospitals in Medicaid expansion states saw increased Medicaid discharges, increased Medicaid revenue, and decreased cost of care for the poor, while hospitals in non-expansion states saw a very small increase in Medicaid discharges, a decline in Medicaid revenue, and growth in cost of care to the poor.