2013 Employer Health Benefits Survey
Employer-sponsored insurance covers about 149 million nonelderly people.1 To provide current information about employer-sponsored health benefits, the Kaiser Family Foundation (Kaiser) and the Health Research & Educational Trust (HRET) conduct an annual survey of nonfederal private and public employers with three or more workers. This is the fifteenth Kaiser/HRET survey and reflects employer sponsored health benefits in 2013.
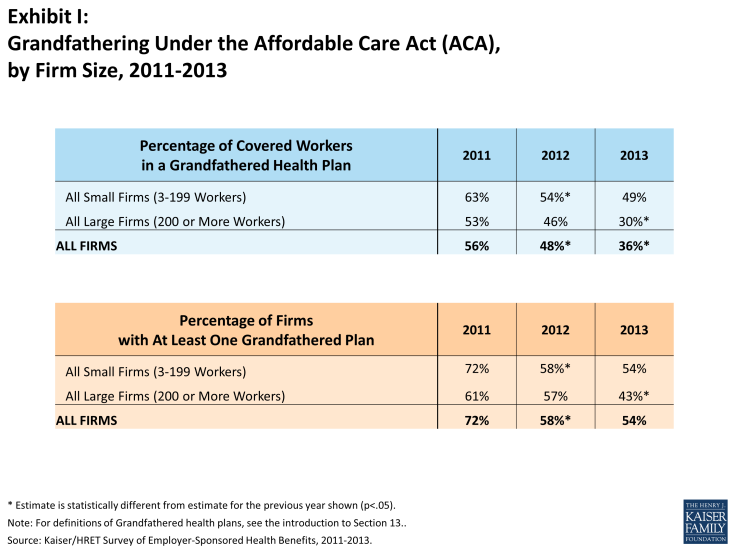
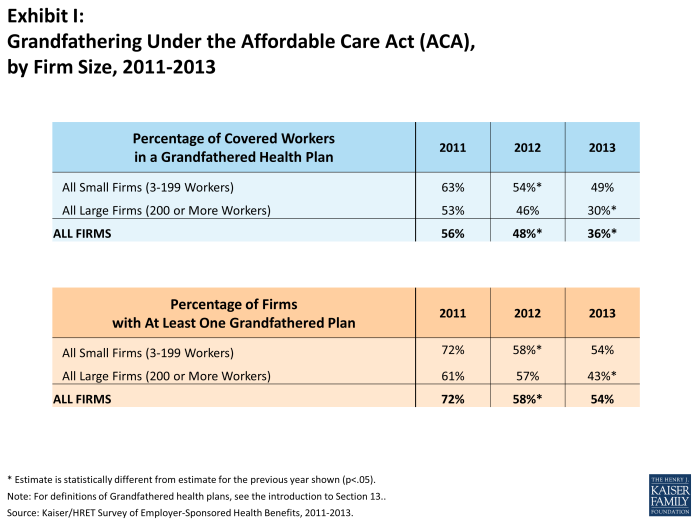
The key findings from the survey, conducted from January through May 2013, include modest increases in premiums for both single coverage (5%) and family coverage (4%). Covered workers generally face similar premium contributions and cost-sharing requirements in 2013 compared to 2012. However, the percentage of covered workers enrolled in plan with a general annual deductible increased in 2013, to over three quarters of covered workers (78%). Additionally, over half (58%) of covered workers at small firms (3-199 workers) now have a deductible of a $1,000 dollars or more. The percentage of firms (57%) which offer health benefits to at least some of their employees and the percentage of workers covered at those firms (62%) are statistically unchanged from 2012. The percentage of covered workers enrolled in grandfathered health plans – those plans exempt from many provisions of the Affordable Care Act (ACA) – declined to 36% of covered workers from 48% in 2012 and 56% in 2011. Firms offering health benefits continue to offer wellness and health promotion programs: 77% of firms offer at least one wellness program, 24% offer employees health risk assessments, and 57% offer at least one disease management program. Small percentages of these firms use financial incentives in order to encourage workers to participate or complete these activities.
HEALTH INSURANCE PREMIUMS AND WORKER CONTRIBUTIONS
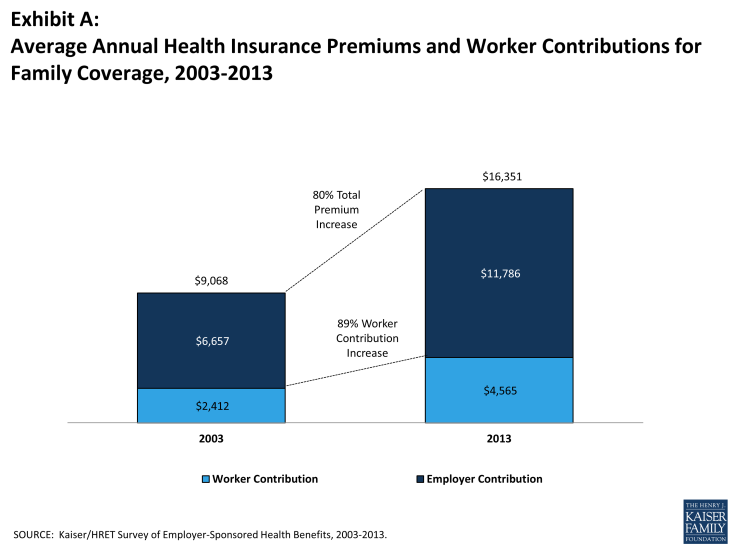
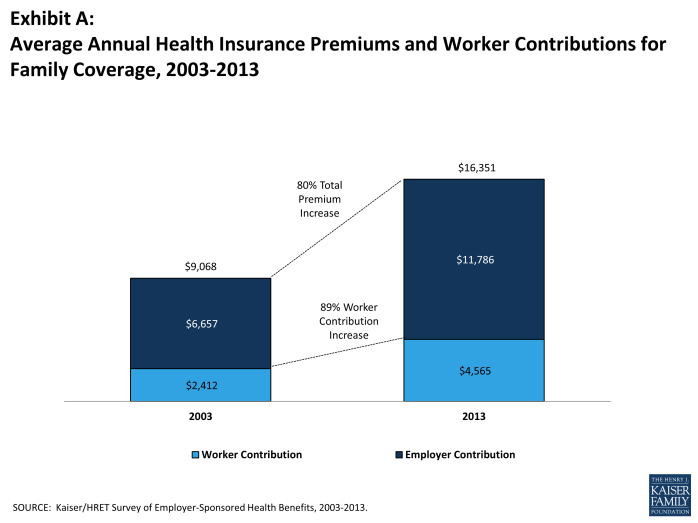
In 2013, the average annual premiums for employer-sponsored health insurance are $5,884 for single coverage and $16,351 for family coverage. The single premium is 5% higher and the family premium is 4% higher than the 2012 average premiums. During the same period workers’ wages increased 1.8% and inflation increased 1.1%.2 Over the last 10 years, the average premium for family coverage has increased 80% (Exhibit A).
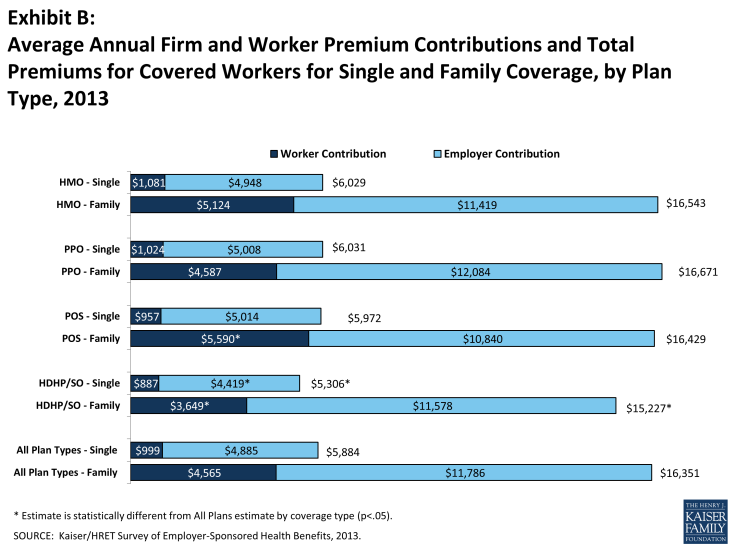
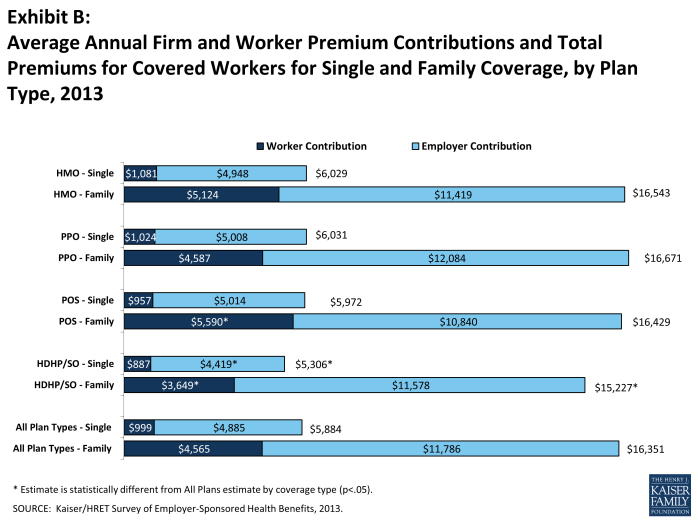
Average premiums for high-deductible health plans with a savings option (HDHP/SOs) are lower than the overall average for all plan types for both single and family coverage (Exhibit B), at $5,306 and $15,227, respectively. Looking at firm size, the average premium for family coverage is lower for covered workers in small firms (3-199 workers) than for workers in larger firms ($15,581 vs. $16,715).
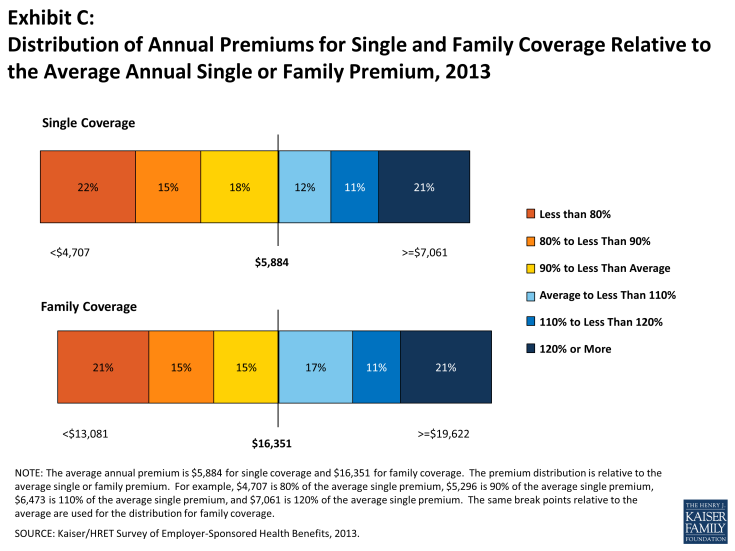
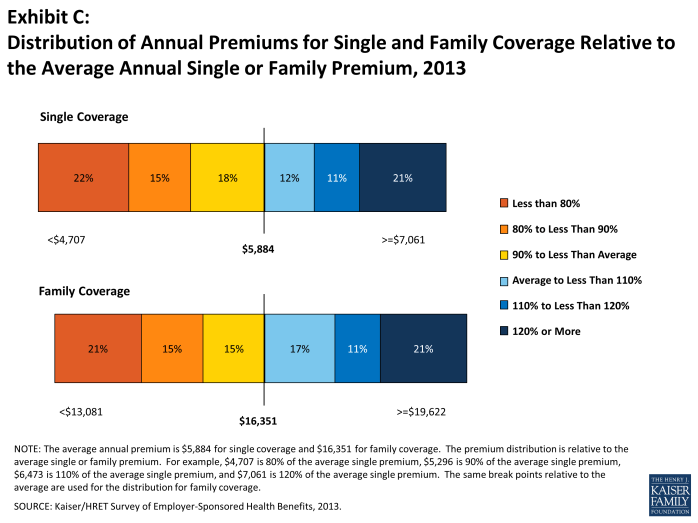
There is significant variation around the average single and family premiums, resulting from differences in benefits, cost sharing, covered populations, and geographical location. Twenty-one percent of covered workers are in plans with an annual total premium for family coverage of at least $19,622 (120% of the average family premium), while 21% of covered workers are in plans where the family premium is less than $13,081 (80% of the average family premium). The distribution is similar around the average single premium (Exhibit C).
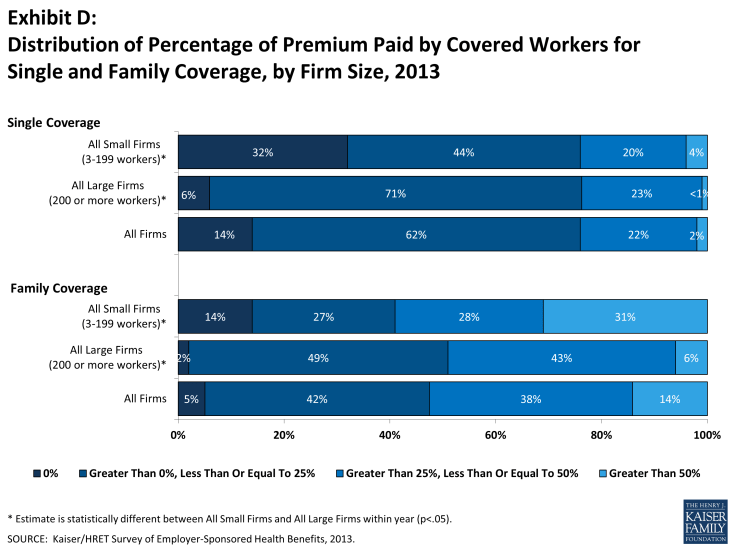
Most often, employers require that workers make a contribution towards the cost of the premium. Covered workers contribute on average 18% of the premium for single coverage and 29% of the premium for family coverage, similar to the percentages contributed in 2012 and relatively unchanged over the past decade. Workers in small firms (3 – 199 workers) contribute a lower average percentage for single coverage compared to workers in larger firms (16% vs. 19%), but they contribute a higher average percentage for family coverage (36% vs. 26%). Workers in firms with a higher percentage of lower-wage workers (at least 35% of workers earn $23,000 or less) contribute higher percentages of the premium for single coverage (23% vs. 17%) and for family coverage (39% vs. 29%) than workers in firms with a smaller share lower-wage workers.
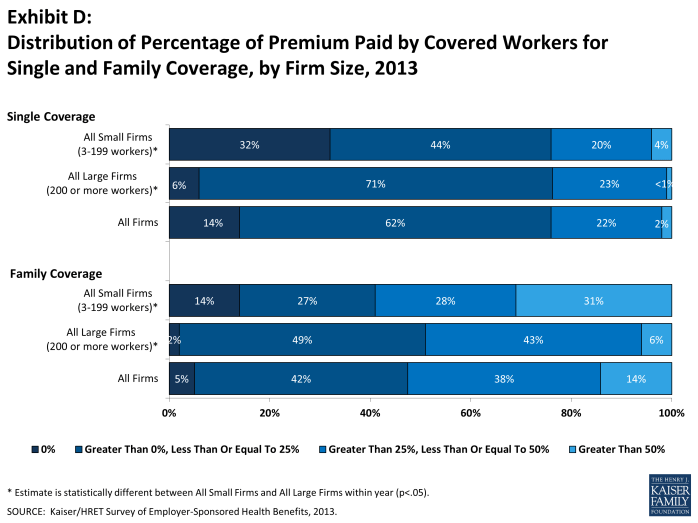
As with total premiums, the share of the premium contributed by workers varies considerably among firms. For single coverage, 62% of covered workers are in plans that require them to make a contribution of less than or equal to a quarter of the total premium, 2% are in plans that require a contribution of more than half of the premium, and 14% are in plans that require no contribution at all. For family coverage, 42% of covered workers are in plans that require them to make a contribution of less than or equal to a quarter of the total premium and 14% are in plans that require more than half of the premium, while only 5% are in plans that require no contribution at all for family coverage (Exhibit D).
Looking at the dollar amounts that workers contribute, the average annual premium contributions in 2013 are $999 for single coverage and $4,565 for family coverage. Neither amount is a statistically significant increase over the 2012 values ($951 and $4,316, respectively). Covered workers’ average dollar contribution to family coverage has increased 89% since 2003 and 36% since 2008 (Exhibit A). Workers in small firms (3 – 199 workers) have lower average contributions for single coverage than workers in larger firms ($862 vs. $1,065), but higher average contributions for family coverage ($5,284 vs. $4,226). Workers in firms with a higher percentage of lower-wage workers (at least 35% of workers earn $23,000 or less) have higher average contributions for single coverage ($1,234 vs. $979) and for family coverage ($5,818 vs. $4,455) than workers in firms with lower percentages of lower-wage workers.
PLAN ENROLLMENT
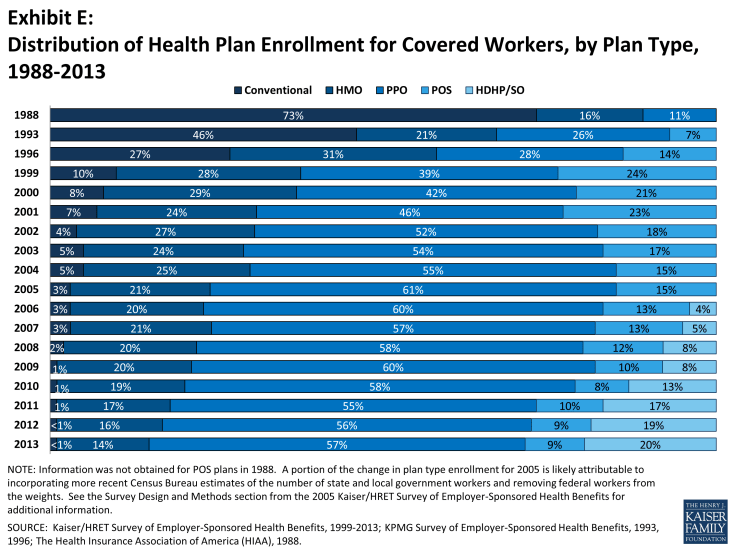
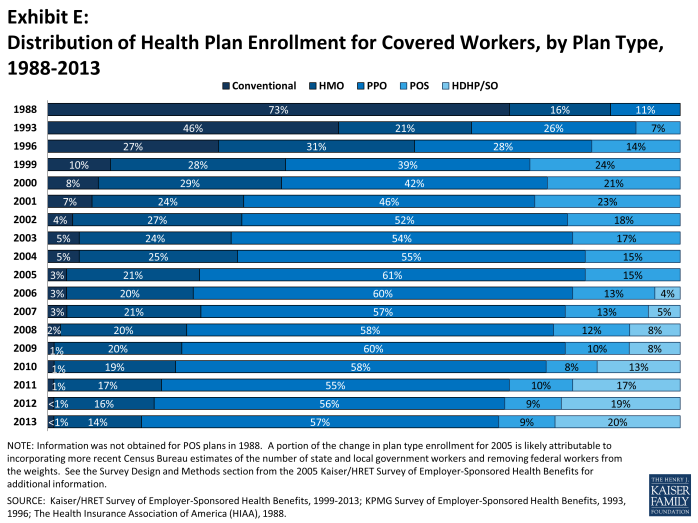
PPO plans remain the most common plan type, enrolling 57% of covered workers in 2013. Twenty percent of covered workers are enrolled in an HDHP/SO, 14% in an HMO, 9% in a POS plan, and less than 1% in a conventional plan (Exhibit E). Enrollment in HDHP/SOs increased significantly between 2009 and 2011, from 8% to 17% of covered workers, but has plateaued since then (Exhibit E). Enrollment distribution varies by firm size, for example, PPOs are relatively more popular for covered workers at large firms (200 or more workers) than smaller firms (62% vs. 47%) and POS plans are relatively more popular among smaller firms than large firms (16% vs. 5%).
EMPLOYEE COST SHARING
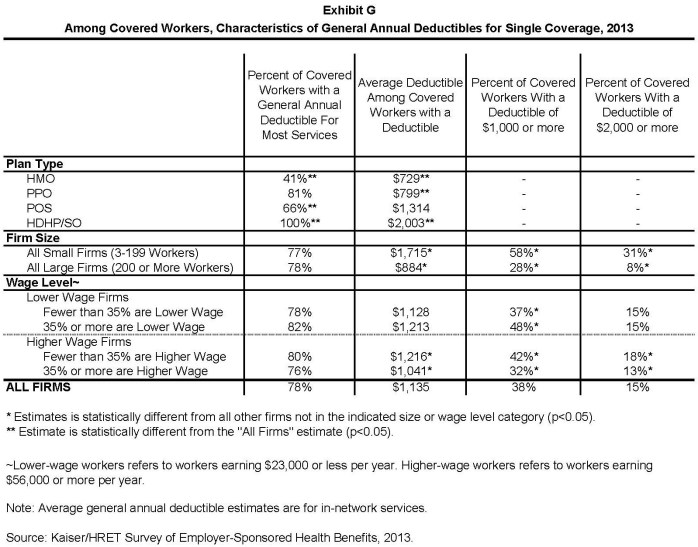
Most covered workers face additional plan costs when they use health care services. Seventy-eight percent of covered workers have a general annual deductible for single coverage that must be met before most services are reimbursed by the plan. Even workers without a general annual deductible often face other types of cost sharing when they use services, such as copayments or coinsurance for office visits and hospitalizations.
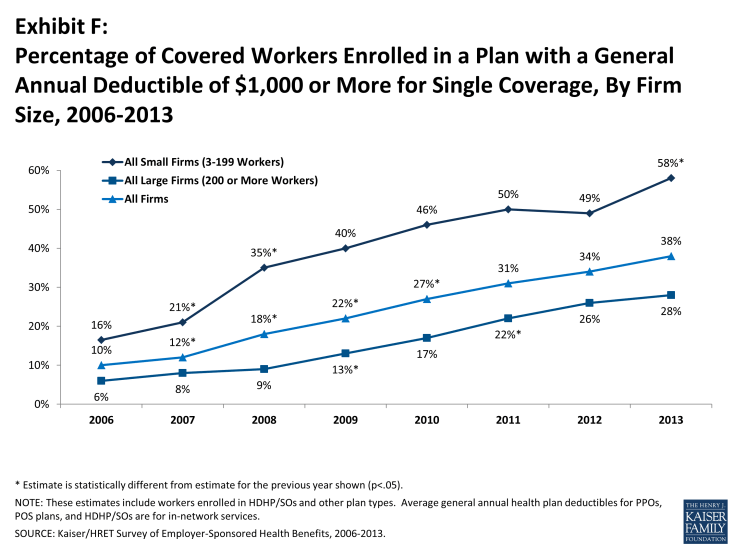
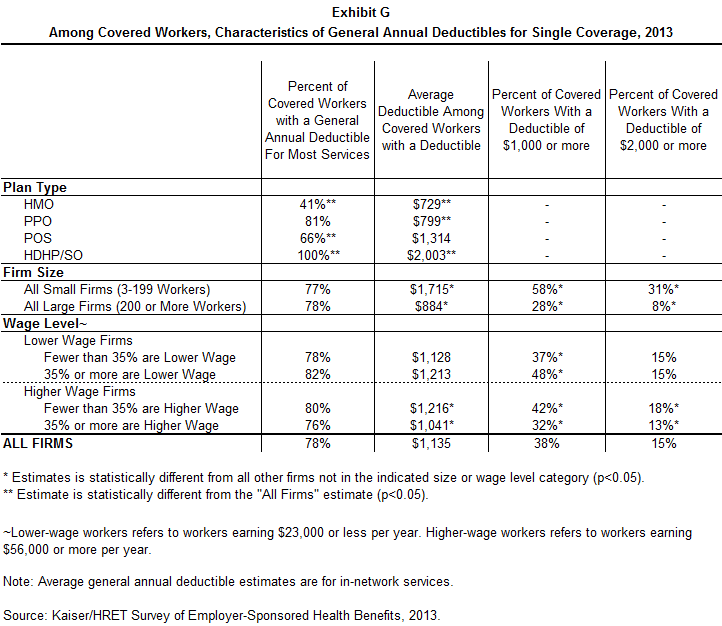
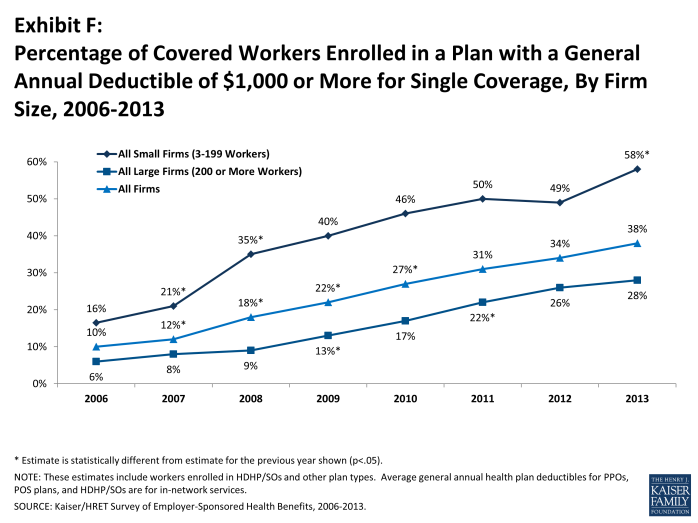
Among covered workers with a general annual deductible, the average deductible amount for single coverage is $1,135. The average annual deductible is unchanged from 2012 ($1,097), but has increased from $735 dollars in 2008. Deductibles differ by firm size: for workers in plans with a deductible, the average deductible for single coverage is $1,715 in small firms (3-199 workers), compared to $884 for workers in larger firms (Exhibit G). Among all covered workers, 58% in small firms (3-199 workers) and 28% in larger firms are in a plan with a deductible of at least $1,000 for single coverage (Exhibit F). The percentage of covered workers at small firms (3-199 workers) with a deductible of a $1,000 or more increased significantly in 2013 from 49% in 2012.
The large majority of workers also have to pay a portion of the cost of physician office visits. Almost three-in-four covered workers pay a copayment (a fixed dollar amount) for office visits with a primary care physician (74%) or a specialist physician (72%), in addition to any general annual deductible their plan may have. Smaller shares of workers pay coinsurance (a percentage of the covered amount) for primary care office visits (20%) or specialty care visits (20%). For in-network office visits, covered workers with a copayment pay an average of $23 for primary care and $35 for specialty care. For covered workers with coinsurance, the average coinsurance for office visits is 18% for primary and for specialty care. While the survey collects information only on in-network cost sharing, it is generally understood that out-of-network cost sharing is higher.
The cost sharing that a person pays when they fill a prescription usually varies with the type of drug – for example whether it is a generic, brand-name or specialty drug – and whether the drug is considered preferred or not on the plan’s formulary. These factors result in each drug being assigned to a tier that represents a different level, or type, of cost sharing. Eighty-one percent of covered workers are in plans with three-or-more tiers of cost sharing. Copayments are the most common form of cost sharing for tiers one through three and coinsurance is the most common form of cost sharing for drugs on the fourth or higher tier of formularies. Among workers with three-or-more tier plans, the average copayments in these plans are $10 for first-tier drugs, $29 for second-tier drugs, $52 for third-tier drugs, and $80 for fourth-tier drugs – similar to the amounts reported last year. HDHP/SOs have a somewhat different cost-sharing pattern for prescription drugs than other plan types: just 61% of covered workers are enrolled in a plan with three-or-more tiers of cost sharing, while 12% are in plans that pay the full cost of prescriptions once the plan deductible is met, and 18% are in a plan with the same cost sharing for all prescription drugs.
Most workers also face additional cost sharing for a hospital admission or an outpatient surgery episode. After any general annual deductible is met, 61% of covered workers have a coinsurance and 16% have a copayment for hospital admissions. Lower percentages have per day (per diem) payments (7%), a separate hospital deductible (3%), or both copayments and coinsurance (8%). The average coinsurance rate for hospital admissions is 18%, the average copayment is $278 per hospital admission, the average per diem charge is $264, and the average separate annual hospital deductible is $436. The cost-sharing provisions for outpatient surgery are similar to those for hospital admissions, as most covered workers have either coinsurance (62%) or copayments (18%). For covered workers with cost sharing for each outpatient surgery episode, the average coinsurance is 18% and the average copayment is $140.
Most plans limit the amount of cost sharing workers must pay each year, generally referred to as an out-of-pocket maximum. Eighty-eight percent of covered workers have an out-of-pocket maximum for single coverage, but the actual dollar limits differ considerably. For example, among covered workers in plans that have an out-of-pocket maximum for single coverage, 43% are in plans with an annual out-of-pocket maximum of $3,000 or more, and 15% are in plans with an out-of-pocket maximum of less than $1,500. Even in plans with a specified out-of-pocket limit, not all spending is counted towards meeting the limit. For example, among workers in PPOs with an out-of-pocket maximum, 76% are in plans that do not count towards physician office visit copayments, 34% are in plans that do not count towards spending on the general annual deductible, and 84% are in plans that do not count towards prescription drug spending when determining if an enrollee has reached the out-of-pocket limit. The ACA will require that all non-grandfathered plans have an out-of-pocket maximum that counts all cost sharing towards the limit.
AVAILABILITY OF EMPLOYER-SPONSORED COVERAGE
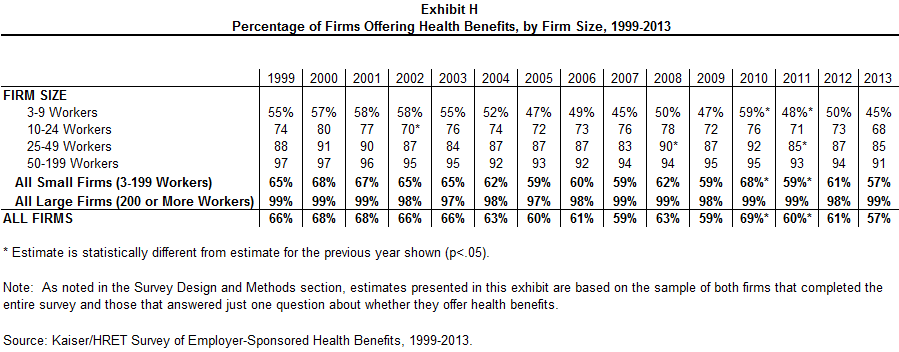
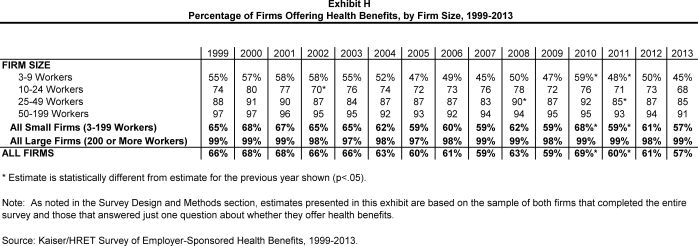
Fifty-seven percent of firms offer health benefits to their workers, statistically unchanged from the percentage that offered last year (61%) (Exhibit H). The offer rate is similar between 2012 and 2013 for both small firms (3 – 199 workers) and larger firms. The likelihood of offering health benefits differs significantly by size of firm, with only 45% of employers with 3 to 9 workers offering coverage, but virtually all employers with 1,000 or more workers offering coverage to at least some of their employees. Ninety percent of workers are in a firm that offers health benefits to at least some of its employees, similar to 2012 (92%). Offer rates also differ by other firm characteristics; 59% of firms with fewer younger workers (less than 35% of the workers are age 26 or younger) offer health benefits compared to 23% of firms with more younger workers.
Even in firms that offer health benefits, not all workers are covered. Some workers are not eligible to enroll as a result of waiting periods or minimum work-hour rules. Other workers do not enroll in coverage offered to them because of the cost of coverage or because they are covered through a spouse. Among firms that offer coverage, an average of 77% of workers are eligible for the health benefits offered by their employer. Of those eligible, 80% take up their employer’s coverage, resulting in 62% of workers in offering firms having coverage through their employer. Among both firms that offer and do not offer health benefits, 56% of workers are covered by health plans offered by their employer, the same percentage as 2012.
RETIREE COVERAGE
Twenty-eight percent of large firms (200 or more workers) that offer health benefits in 2013 also offer retiree health benefits, similar to the percentage (25%) in 2012. Among large firms (200 or more workers) that offer retiree health benefits, 90% offer health benefits to early retirees (workers retiring before age 65), 67% offer health benefits to Medicare-age retirees, and 4% offer a plan that covers exclusively prescription drugs.
WELLNESS
Employers continue to offer programs in large numbers that help employees identify issues with their health and engage in healthier behavior. These include offering their employees the opportunity to complete a health risk assessment, and offering a variety of wellness programs that promote healthier lifestyles, including better diet and more exercise. Some employers have begun to collect biometric information from employees (e.g., cholesterol levels and body mass index) and are using it as part of their wellness and health promotion programs.
Almost one-in-four employers (24%) offering health benefits provide employees with an opportunity to complete a health risk assessment. A health risk assessment includes questions about medical history, health status, and lifestyle, and is designed to identify the health risks of the person being assessed. Large firms (200 or more workers) are more likely than smaller firms to ask employees to complete a health risk assessment (55% vs. 23%). Among these firms, 54% of large firms (200 or more workers) report that they provide a financial incentive to employees that complete the assessment.
Fifty-five percent of large firms (200 or more workers) and 26% of smaller firms offering health benefits report offering biometric screening to employees. A biometric screening is a health examination that measures an employee’s risk factors, such as body weight, cholesterol, blood pressure, stress, and nutrition. Of these firms, 11% percent of large firms require employees to complete a biometric screening to enroll in the health plan; and 11% of large firms report that employees may be financially rewarded or penalized based in meeting biometric outcomes.
Virtually all large employers (200 or more workers) and most smaller employers offer at least one wellness program. Seventy-seven percent of employers offering health benefits offer at least one of the following wellness programs in 2013: weight loss programs, gym membership discounts or on-site exercise facilities, biometric screening, smoking cessation programs, personal health coaching, classes in nutrition or healthy living, web-based resources for healthy living, flu shots or vaccinations, Employee Assistance Programs (EAP), or a wellness newsletter. Large firms (200 or more workers) are more likely to offer one of these programs than smaller firms (99% vs. 76%). Of firms offering health benefits and a wellness program, 36% of large firms (200 or more workers) and 8% of smaller firms offer employees a financial incentive to participate in a wellness program, such as smaller premium contributions, smaller deductibles, higher HSA/HRA contributions or gift cards, travel, merchandise or cash.
OTHER EMPLOYER PROGRAMS
Disease Management Programs. Most employers offer at least one disease management program as part of their largest health plan. Disease management programs identify people with chronic illnesses, such as diabetes, depression and hypertension, and offer treatment options to manage or improve the identified condition. Large firms (200 or more workers) are more likely to have a disease management program as part of their largest health plan than small firms (77% vs. 57%). Only 8% of large firms (200 or more workers) whose largest plan includes a disease management program, have a financial incentive to encourage employees to participate.
High Performance or Tiered Networks. Almost a quarter (23%) of employers offering health benefits have high performance or tiered networks in their largest health plan. These programs identify providers that are more efficient or have higher quality care, and may provide financial or other incentives for enrollees to use the selected providers.
Retail Health Clinics. Fifty-six percent of employers offering health benefits cover services provided by retail health clinics. These may be health clinics located in grocery stores or pharmacies to treat minor illnesses or provide preventive services, such as vaccines or flu shots. Among firms covering services in these settings, 17% provide a financial incentive to receive services in a retail clinic instead of a physician’s office.
OTHER TOPICS
Grandfathered Health Plans. The ACA exempts “grandfathered” health plans from a number of its provisions, such as the requirements to cover preventive benefits without cost sharing or the new rules for small employers’ premiums ratings and benefits. An employer-sponsored health plan can be grandfathered if it covered a worker when the ACA became law (March 23, 2010) and if the plan has not made significant changes that reduce benefits or increase employee costs.3 Fifty-four percent of firms offering health benefits offer at least one grandfathered health plan in 2013, similar to the percentage reported in 2012. Small firms (3-199 workers) are more likely than larger firms to offer a grandfathered health plan (54% vs. 43%). Looking at enrollment, 36% of covered workers are enrolled in a grandfathered health plan in 2013, down from 48% in 2012 (Exhibit I). Covered workers in small firms (3-199 workers) are more likely than covered workers in larger firms to be enrolled in a grandfathered health plan (49% vs. 30%).
Self-Funding. Sixteen percent of covered workers at small firms (3-199 workers) and 83% of covered workers at larger firms are enrolled in plans which are either partially or completely self-funded, similar to 2012 (15% and 81%). Six percent of firms offering fully-insured plans report that they intend to self-insure because of the ACA.
Shopping for Coverage. Fifty-four percent of firms shopped for a new health plan or insurance carrier in the previous year. There was not a significant difference between small (3 – 199 workers) and larger firms in the likelihood of shopping for new coverage. Among firms that shopped, 18% changed carriers in the past year and 15% changed the type of health plan (e.g., HMO, PPO, POS or HDHP/SO) that they offer.
Exchanges for Large Employers. In the last two years, several consulting firms have announced that they were creating private exchanges for employers.4,5 These exchanges would provide employers an opportunity to give their employees a contribution that may be used to choose from a potentially broad choice of health plans that would be managed by the exchange. While few employers have adopted this approach to date, 9% of large firms (200 or more employees), including 29% of firms with 5,000 or more employees, reported that they are considering offering health benefits through a private exchange in the future. This interest may signal a significant change in the way that employers approach health benefits and the way employees get coverage, with employers playing a less active role in plan design and management.
CONCLUSION
The 2013 annual survey did not find major changes in employer-based health benefits. Premiums increased at modest levels, consistent with the last several years, and coverage and offer rates did not change significantly. Employers remain committed to wellness programs: most covered workers are in plans with some type of wellness program and a majority (67%) of employers believes that wellness programs are very or somewhat effective in controlling health care costs.
More changes are expected over the next several years as many of more far-reaching provisions of the health reform law will take effect in 2014, including new benefits, cost-sharing tiers and premium rating rules that will apply to plans for employers with 50 or fewer workers. While several provisions affecting some larger employers have been delayed, most notably the requirement to offer coverage to all full-time employees by 2014, employers may begin adapting benefits and contributions to prepare to meet this requirement for 2015. The adoption of new federal rules for employee wellness programs, which permit employers to have larger financial rewards for employees who participate in wellness programs or who meet defined health outcomes, may encourage employers to modify or extend their wellness approaches.
The emergence of new exchanges, or marketplaces, also may portend important changes for employer-sponsored health insurance. Through an exchange, an employer can provide employees with a larger number and type of health plan options. Exchanges also facilitate the use of defined contributions or other strategies that encourage employees to choose lower cost plans or pay the difference in costs themselves. New SHOP exchanges will offer coverage options to small employers beginning in 2014, although employee choice will be limited in the federal SHOP exchanges until 2015. Large employers have the option of offering coverage through one of several exchanges being sponsored by benefit consulting organizations. While these approaches are new and differ across different exchanges, the common theme is to devolve some benefit choices, and some of the financial responsibility for those choices, to employees. Whether this new way of purchasing coverage works for employers and their employees, and how it affects benefits and plan costs, will be among the more important stories for the employer health insurance market over the next few years.
METHODOLOGY
The Kaiser Family Foundation/Health Research & Educational Trust 2013 Annual Employer Health Benefits Survey (Kaiser/HRET) reports findings from a telephone survey of 2,067 randomly selected public and private employers with three or more workers. Researchers at the Health Research & Educational Trust, NORC at the University of Chicago, and the Kaiser Family Foundation designed and analyzed the survey. National Research, LLC conducted the fieldwork between January and May 2013. In 2013 the overall response rate is 49%, which includes firms that offer and do not offer health benefits. Among firms that offer health benefits, the survey’s response rate is 50%.
We ask all firms with which we made phone contact, even if the firm declined to participate in the survey: “Does your company offer a health insurance program as a benefit to any of your employees?” A total of 2,948 firms responded to this question (including the 2,067 who responded to the full survey and 881 who responded to this one question). Their responses are included in our estimates of the percentage of firms offering health coverage. The response rate for this question is 70%.
Since firms are selected randomly, it is possible to extrapolate from the sample to national, regional, industry, and firm size estimates using statistical weights. In calculating weights, we first determine the basic weight, then apply a nonresponse adjustment, and finally apply a post-stratification adjustment. We use the U.S. Census Bureau’s Statistics of U.S. Businesses as the basis for the stratification and the post-stratification adjustment for firms in the private sector, and we use the Census of Governments as the basis for post-stratification for firms in the public sector. Some numbers in the exhibits in the report do not sum up to totals due to rounding effects, and, in a few cases, numbers from distribution exhibits referenced in the text may not add due to rounding effects. Unless otherwise noted, differences referred to in the text and exhibits use the 0.05 confidence level as the threshold for significance.
For more information on the survey methodology, please visit the Survey Design and Methods Section at http://ehbs.kff.org/.
The Kaiser Family Foundation, a leader in health policy analysis, health journalism and communication, is dedicated to filling the need for trusted, independent information on the major health issues facing our nation and its people. The Foundation is a non-profit private operating foundation, based in Menlo Park, California.
The Health Research & Educational Trust is a private, not-for-profit organization involved in research, education, and demonstration programs addressing health management and policy issues. Founded in 1944, HRET, an affiliate of the American Hospital Association, collaborates with health care, government, academic, business, and community organizations across the United States to conduct research and disseminate findings that help shape the future of health care.