How OBGYNs Adapted Provision of Sexual and Reproductive Health Care During the COVID-19 Pandemic
|
Key Takeaways
|
|
Introduction
The COVID-19 pandemic has had a profound impact on health care access and delivery. While patients’ other health care needs have generally not declined, providers have been tasked with figuring out how to address these needs while mitigating risk to both patients and staff related to the COVID-19 pandemic. Many providers have altered their practice models dramatically, including the rapid adoption of telehealth and reconfiguring practice workflows. While obstetrician-gynecologists (OBGYNs) do not represent the entirety of sexual and reproductive health (SRH) care providers, their experiences offer us insight into the field at a time of great change and adaptation.
At the time the novel coronavirus had started to spread widely within the U.S., KFF was underway fielding a national survey of OBGYNs to understand SRH care provision across the U.S. Realizing that practice patterns had likely changed due to the pandemic, we took the opportunity after the initial survey release to add a subset of questions related to provision of care during the COVID-19 pandemic. A nationally representative sample of 855 office-based U.S. OBGYNs answered the COVID-19 supplemental questions from July 8, 2020 to September 1, 2020. In this brief, we report on how the COVID-19 pandemic has impacted the provision of SRH care by U.S. OBGYNs.
The margin of sampling error for these questions is +/-6 percentage points at the 95% confidence level. All comparisons noted in this brief are statistically significant (p <0.05). A summary of physician and practice characteristic definitions can be found in the methodology section.
Declines in Visit Volume
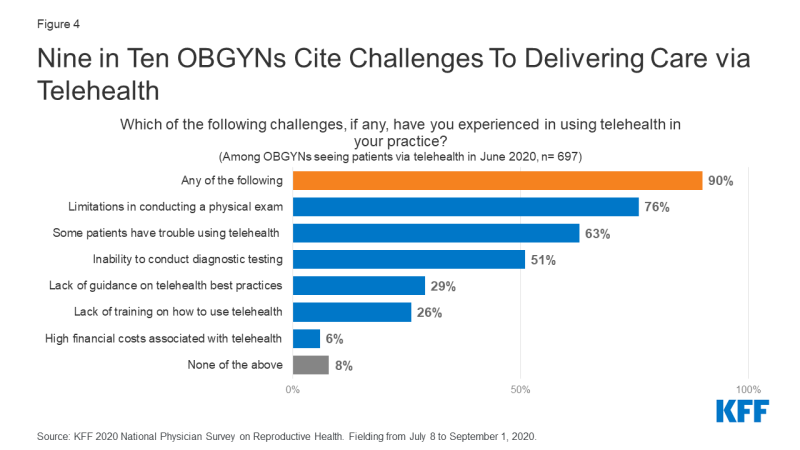
At the time of the survey, more than half (54%) of OBGYNs said they had seen a decrease in the number of patient visits since the COVID-19 pandemic started in March 2020. Approximately a third (35%) saw about the same number of patients, while a minority (10%) saw more patients since the beginning of the pandemic (Figure 1). Those who were in small practices, defined as ≤ 3 full-time equivalent (FTE) doctors or advanced practice clinicians, appear to have been hit the hardest, with 73% of OBGYNs at small practices reporting a decrease in patients compared to 46% and 48% of OBGYNs at medium (4-10 FTE) and large practices (>10 FTE). Also, more OBGYNs age 65+ reported seeing declines in patient visits, compared to all younger age groups (80% for age 65+, 59% for age 55-64, 58% for age 45-54, 38% for age <45); this is also the age group that had the largest share of OBGYNs who did not utilize any telehealth in June 2020 (Table 2).
When those who reported a decrease in patient volume were asked to identify the primary driver of the decline, most attributed the decline to fewer patients seeking care (45%) or practice specific limitations (37%). State restrictions on health care services was less commonly (7%) cited as the primary reason for declines in patient volume (Figure 1).
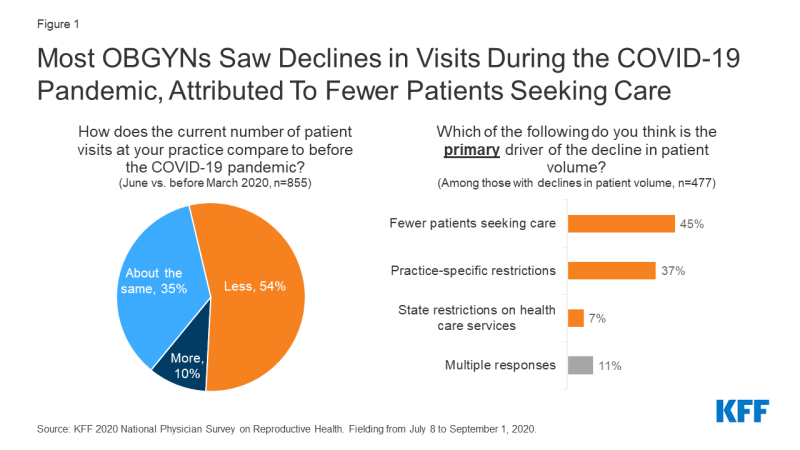
Figure 1: Most OBGYNs Saw Declines in Visits During the COVID-19 Pandemic, Attributed To Fewer Patients Seeking Care
Telehealth Utilization
During the COVID-19 pandemic, the use of telehealth grew rapidly among OBGYNs. Prior to the start of the COVID-19 emergency in the U.S. (March 1, 2020), the vast majority (86%) of OBGYNs said they did not conduct any telehealth visits. By June 2020, however, almost all (84%) reported conducting telehealth visits (Figure 2).
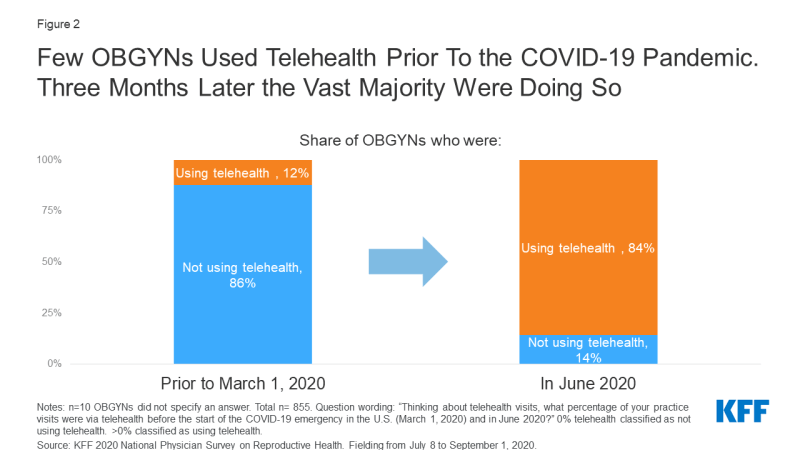
Figure 2: Few OBGYNs Used Telehealth Prior To the COVID-19 Pandemic. Three Months Later the Vast Majority Were Doing So
The average share of overall practice visits that OBGYNs reported conducting via telehealth grew from 1.5% before the COVID-19 emergency to 18% in June 2020. Physicians who had been using telehealth before the pandemic reported using telehealth for a significantly higher share of visits on average in June 2020 compared to those with no prior experience (35% vs. 16%). The average share of total visits conducted via telehealth also differed by physician characteristics, with higher shares of telehealth visits reported among female physicians and those under age 54. There were also differences by practice location, with those practicing in urban locations, the West and Northeast (areas initially hit hardest by the pandemic) and in Medicaid Expansion states reporting a higher share of telehealth visits (Table 1). No differences were identified by practice size.
| Table 1: Average share of total visits conducted via telehealth in June 2020, by demographics | ||
| Thinking about telehealth visits (e.g. virtual visits conducted via video or phone), what percentage of your practice visits were via telehealth in June 2020? | ||
| Average | ||
| Overall | 18% | |
| Used Telehealth Prior to the COVID-19 Pandemic | Yes | 35* |
| No | 16 | |
| Gender | Female | 20* |
| Male | 14 | |
| Age | <45 | 21 |
| 45-54 | 23* | |
| 55-64 | 11 | |
| 65+ | 14 | |
| Region | West | 26* |
| Northeast | 21* | |
| Midwest | 16 | |
| South | 13 | |
| Urbanicity | Urban | 19* |
| Suburban | 18 | |
| Rural | 11 | |
| Practice in Medicaid Expansion State | Yes | 21* |
| No | 12 | |
| * Indicates a statistically significant difference (p<0.05) from reference group in bold | ||
When looking at how often OBGYNs utilized telehealth for patient visits, most did so for a minority of visits in June 2020; few (9%) were using telehealth for >50% of their total visits (Figure 3). Therefore, while the majority of OBGYNs have used some telehealth during the COVID-19 pandemic, most continued to deliver the bulk of their visits via in-person care.
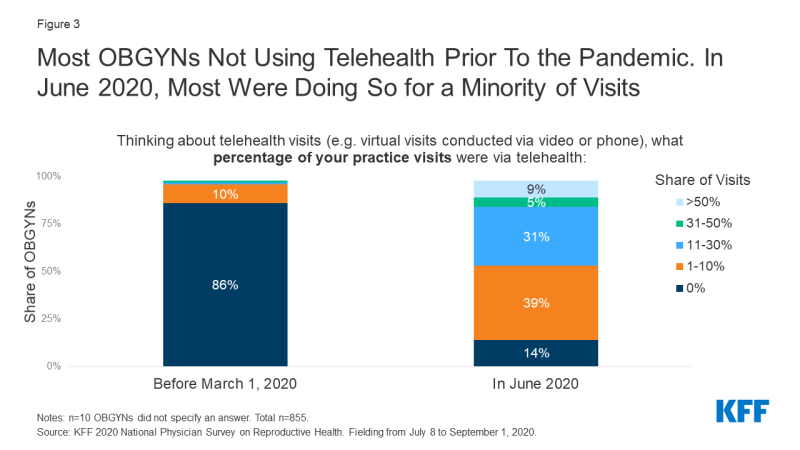
Figure 3: Most OBGYNs Not Using Telehealth Prior To the Pandemic. In June 2020, Most Were Doing So for a Minority of Visits
While there was a major spike in telehealth adoption by June 2020, a small but sizable share of OBGYNs (14%) did not conduct any telehealth visits. A higher share of male OBGYNs compared to female, and older doctors compared to younger doctors reported no telehealth use in June 2020. Additionally, while there has been much discussion about the potential for telehealth to expand access in rural regions where transportation barriers can be a limiting factor in obtaining care, OBGYNs in rural areas were more likely than those in urban and suburban areas to have not adopted telehealth during the pandemic. About 1 in 4 OBGYNs practicing in rural areas, small practices and in states without Medicaid expansion reported no telehealth use (Table 2).
| Table 2: Who has not adopted telehealth into their practice during the COVID-19 pandemic? | ||
| Share of OBGYNs who reported no telehealth use in June 2020 | ||
| Overall | 14% | |
| Used Telehealth Prior to the COVID-19 Pandemic | Yes | 1* |
| No | 16 | |
| Gender | Female | 9* |
| Male | 23 | |
| Age | <45 | 6* |
| 45-54 | 9* | |
| 55-64 | 20 | |
| 65+ | 28 | |
| Practice Size1 | Large | 9* |
| Medium | 10* | |
| Small | 22 | |
| Urbanicity | Urban | 12* |
| Suburban | 8* | |
| Rural | 29 | |
| Practice in Medicaid Expansion State | Yes | 9* |
| No | 24 | |
| Question wording: “Thinking about telehealth visits (e.g. virtual visits conducted via video or phone), what percentage of your practice visits were via telehealth in June 2020?” Those who indicated 0% telehealth visits classified as no telehealth use. *Indicates statistically significant difference (p<0.05) from reference group in bold 1Practice size defined by number of full-time equivalent (FTE) doctors and advance practice clinicians: small ≤3 FTE, medium 4-10 FTE and large >10 FTE. |
||
Telehealth Challenges
Among OBGYNs who provided telehealth care in June 2020, nine in ten (90%) experienced a telehealth-related challenge. The most cited challenge was the limitation in conducting physical exams (76%), followed by their patients having trouble using telehealth (63%), the inability to conduct diagnostic testing via telehealth (51%), lack of guidance on telehealth best practices (29%) and lack of training on how to use telehealth effectively (26%). A small minority cited high financial costs associated with establishing a telehealth program as a challenge (6%) (Figure 4).
For OBGYNs who had not been using telehealth prior to the pandemic, a higher share reported telehealth challenges (93%) compared to those who had used telehealth prior (75%). Those without prior telehealth use more often cited lack of training (29% vs. 5%), lack of guidance on best practices (32% vs. 14%) and limitations in conducting a physical exam (80% vs. 54%) as challenges, compared to those with prior telehealth use (Figure 5).
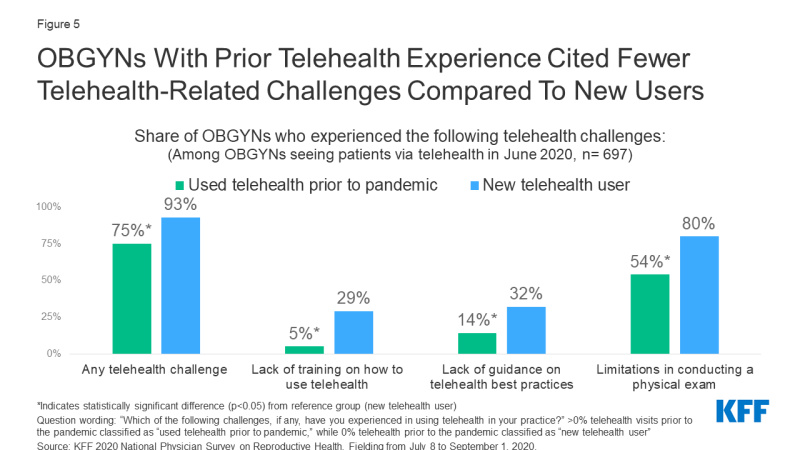
Figure 5: OBGYNs With Prior Telehealth Experience Cited Fewer Telehealth-Related Challenges Compared To New Users
When thinking about the sustainability of telehealth beyond the COVID-19 emergency in the U.S., reimbursement was an issue cited by many. About half of OBGYNs (52%) reported they would need to be reimbursed at the same rate for telehealth compared to in-person care to continue conducting telehealth visits (Figure 6). About one in four (28%) said they would need to be reimbursed at 75-99% compared to in-person care to continue to offer telehealth. Few (11%) would accept <75% reimbursement for telehealth compared to in-person care, and 7% said they would not offer telehealth at all after the resolution of the COVID-19 emergency. Notably, a larger share of OBGYNs practicing in public clinics said they would not offer telehealth in the future, compared to those in private practice (16% vs. 5%).

Figure 6: Most OBGYNs Expect To Be Reimbursed for Telehealth at a Comparable Rate To In-Person Care
Financial and Staffing Challenges
Four in five (81%) OBGYNs said their practice experienced at least one financial or staffing challenge as a result of the COVID-19 pandemic. The most commonly cited experiences were reducing operating hours (56%), reducing pay for clinicians (39%) and furloughing or laying off non-clinical staff (37%). Fewer reduced pay for non-clinical staff (17%), furloughed or laid off clinicians (16%) or closed the practice temporarily (13%) (Table 3). Half of OBGYNs reported that their practice experienced more than one of these challenges.
| Table 3: Challenges Experienced by OBGYN Practices During the COVID-19 Pandemic | |
| Which of the following, if any, has your practice experienced because of the impact of COVID-19? | |
| Reduced operating hours | 56% |
| Reduced pay for clinicians | 39% |
| Reduced pay for non-clinical staff | 17% |
| Furloughed or laid off clinicians | 16% |
| Furloughed or laid off non-clinical staff | 37% |
| Closed the practice temporarily | 13% |
| Closed the practice permanently | 1% |
| Merged with another practice | 3% |
| At least one of the above | 81% |
| More than one of the above | 50% |
| None of the above | 19% |
Financial and staffing challenges affected different shares of OBGYNs depending on practice type and setting (Figure 7). Temporarily closing their practices was reported by a higher share of OBGYNs in the Northeast (26%) compared to the West (10%), Midwest (9%) and South (10%); this was also the case for OBGYNs in small practices (22%) compared to those in medium (11%) and large practices (6%). Reducing operating hours was more common among OBGYNs in urban (59%) and suburban (71%) practices compared to those in rural practices (41%), as well as OBGYNs working in private practice (60%) compared to public clinics (37%). Additionally, a higher share of OBGYNs in private practice than public reported reduced pay for clinicians (42% vs. 22%).
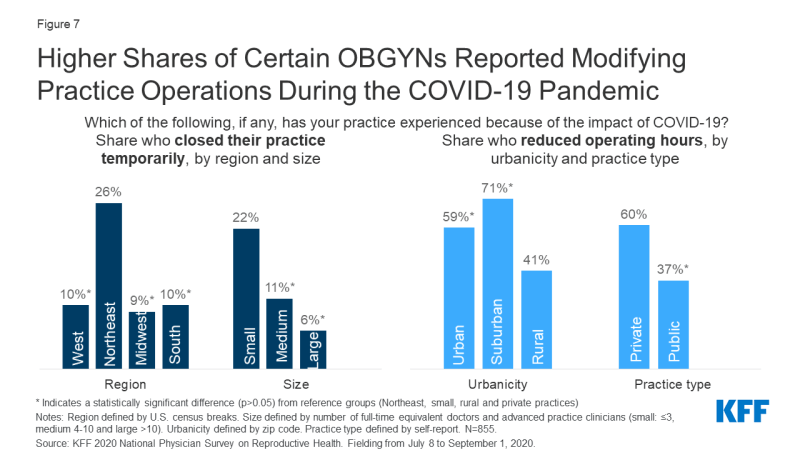
Figure 7: Higher Shares of Certain OBGYNs Reported Modifying Practice Operations During the COVID-19 Pandemic
Delivery of Reproductive Health Care
mode of Delivery
Despite the rapid growth in telemedicine visits, the vast majority of OBGYNs continued to provide basic contraceptive services and STI testing during the COVID-19 pandemic via in-person care. This includes LARC placement (92%), IUD removal (95%), contraceptive injections (93%), prescription of hormonal contraceptive pills (75%) and STI testing for symptomatic patients (94%) (Table 4).
| Table 4: Most OBGYNs Continued to Provide SRH Services In Person During July-August 2020 | |||
| Indicate if, and how, you are currently providing the following services during the COVID-19 emergency? | |||
| Providing in-person | Providing via telehealth | Not currently providing this service | |
| LARC placement | 92% | n/a | 5% |
| IUD removal | 95% | 2%a | 2% |
| Contraceptive injections | 93% | 3%b | 3% |
| Prescription of hormonal contraceptive pills | 75% | 51% | <1% |
| STI testing for symptomatic patients | 94% | 9% | 1% |
| Notes: Respondents could select multiple response options. a Instructing patients on IUD self-removal; b Instructing patients on SQ self-injection |
|||
Some OBGYNs reported utilizing telehealth to deliver these services. Nearly half (51%) of OBGYNs report prescribing OCPs via telehealth since the COVID-19 pandemic began. Younger OBGYNs age <45 (64%) and 45-54 (63%) were about twice as likely to provide OCPs via telehealth than older OBGYNs age 55-64 (34%) and 65+ (28%). Prescribing OCPs via telehealth was also more common among female OBGYNs compared to male (61% vs. 33%), OBGYNs in urban locations compared to rural (55% vs. 35%), and those in large practices compared to small (64% vs. 44%). Providers in the West (67%) reported higher rates of providing OCPs via telehealth compared to those in the Midwest (45%) and South (44%), as well as those in states with Medicaid expansion compared to states without Medicaid expansion (57% vs. 39%) (Table 5).
| Table 5: Provision of OCPs via Telehealth Varies by Physician and Practice Characteristics | ||
| Share who had prescribed OCPs via telehealth during the COVID-19 pandemic | ||
| Overall | 51% | |
| Gender | Female | 61* |
| Male | 33 | |
| Age | <45 | 64* |
| 45-54 | 63* | |
| 55-64 | 34 | |
| 65+ | 28 | |
| Practice Size1 | Large | 64* |
| Medium | 51 | |
| Small | 44 | |
| Urbanicity | Urban | 55* |
| Suburban | 49 | |
| Rural | 35 | |
| Region | West | 67* |
| Northeast | 52 | |
| Midwest | 45 | |
| South | 44 | |
| Practice in Medicaid Expansion State | Yes | 57* |
| No | 39 | |
| Question wording: “Please indicate if, and how, you are currently providing prescription of hormonal contraceptive pills during the COVID-19 emergency.” Table represents those who are providing this service via telehealth. *Indicates statistically significant difference (p<0.05) from reference group in bold 1Practice size defined by number of full-time equivalent (FTE) doctors and advance practice clinicians: small ≤3 FTE, medium 4-10 FTE and large >10 FTE. |
||
Despite innovations in telehealth for use in STI care and contraception, very few OBGYNs reported utilizing telehealth for STI testing (9%), or for providing instruction on self-administered contraceptive injections (3%) or IUD removal (2%) (Table 4). Providers who were using telehealth for >25% of their patient visits in June 2020 reported higher use of telehealth for STI testing (20% vs. 6%), contraceptive injections (8% vs. 1%) and OCP prescription (63% vs. 48%) than providers using telehealth for ≤25% of their visits.
Very few OBGYNs reported that they were not providing the aforementioned services at all at the time this survey was fielded (July 8 to September 1, 2020). In the Northeast (14%), the region hit particularly hard early on in the COVID-19 pandemic, a higher share of doctors reported they were not providing LARC placement at the time of the survey compared to those in the West (4%), Midwest (2%) and South (3%). Similarly, a somewhat higher share of OBGYNs in the Northeast were not providing contraceptive injections (8%) compared to the Midwest (1%) and South (1%) [no statistically significant difference was found from the West (3%)]. It is possible that practices have resumed provision of these services since the fielding of this survey.
Access and Delays in Care
The majority of OBGYNs said it was more difficult to address their patients’ needs during the COVID-19 pandemic; this was true for both reproductive preventive care needs (71%), like STI and cervical cancer screening, as well as chronic gynecological conditions (77%), like addressing fibroids, endometriosis and menopausal symptoms (Figure 8).
Most OBGYNs expressed concern that patients who experience delays in SRH care as a result of the COVID-19 emergency will face negative health consequences. At least six in ten OBGYNs reported being very or somewhat worried about delays in contraceptive care, prenatal care, follow-up care for abnormal pap smears, STI treatment, and obtaining an abortion (Figure 9).

Figure 9: Most OBGYNs Very or Somewhat Worried About Delays in Reproductive Health Care Due To COVID-19
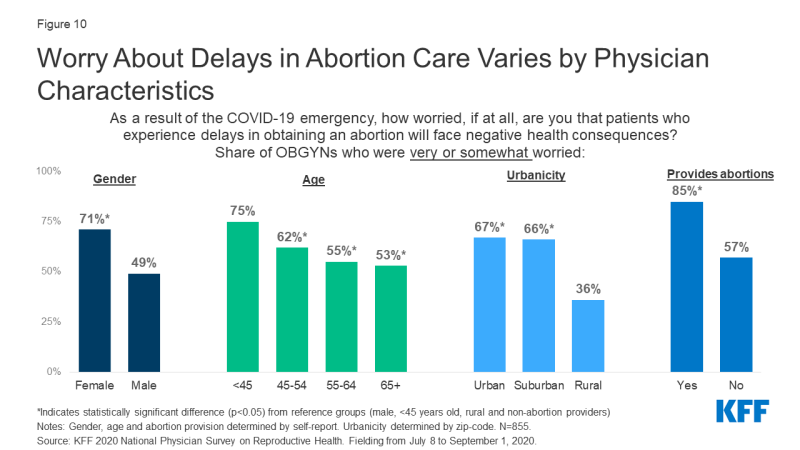
Negative health consequences due to delays in obtaining an abortion were of particular concern to certain groups of OBGYNs. A higher share of female compared to male, urban and suburban compared to rural, and younger compared to older OBGYNs said they were very or somewhat worried about delays in abortion care. Additionally, a higher share of OBGYNs who provide abortions said they were very or somewhat worried about delays in abortion care, compared to OBGYNs who do not provide abortions (Figure 10).
Conclusions and Implications
Since the onset of the COVID-19 pandemic, OBGYNs across the country have been faced with the challenge of how to provide quality sexual and reproductive health (SRH) care to patients during a public health emergency. Our survey finds that most OBGYNs are continuing to provide SRH services, however not without great adaptation. Almost all have changed the way they deliver care, including quickly adopting telehealth, and most have changed, at least temporarily, the way their practice operates, including reducing operating hours and staffing. This rapid response has likely put stressors on both patients and providers. While we were not able to elicit the patient perspective in this survey, we saw that OBGYNs reported declines in patient volumes, largely attributed to fewer patients seeking care, and that OBGYNs worry about the negative health consequences that may result from delays in care. This suggests that patients are facing heightened barriers to accessing care, and that OBGYNs are facing new challenges to providing that care.
While our study provides a snapshot into how OBGYNs adapted their care provision during the Summer of 2020, we recognize that in a rapidly changing environment much has likely evolved since this survey was fielded, and will continue to evolve in the months to come. As the pandemic surges in much of the country, practices may need to reevaluate how they are providing care. OBGYNs, as well as other health care providers, will need to continue to make decisions about how best to meet the sexual and reproductive health care needs of their patients, at a time when patient need for these services has not diminished.