Expanding Postpartum Medicaid Coverage
Issue Brief
High rates of preventable maternal mortality and morbidity and wide racial and ethnic disparities have caught the attention of clinicians, public health practitioners, advocates, and policymakers.1 In the closing days of the Trump Administration, HHS released an action plan to improve maternal health, and President-elect Biden has cited this topic as a key health care issue. Vice President-elect Harris has been an advocate in the Senate for improving maternal health, particularly stemming the disproportionately high rates of maternal mortality and morbidity among Black women, and may continue to champion this work at the Executive Branch. During the 2019-2020 Congressional session, more than a dozen bills across political lines related to maternal health outcomes, care, and coverage were introduced, and many could be re-introduced when the new Congress is seated. Several federal and state efforts aim to address the postpartum period, the time shortly after the birth of an infant, an important but often neglected element of maternity care. Birthing parents may be dealing with a host of medical conditions, such as complications from childbirth, pain, depression or anxiety, all while caring for a newborn. It can be a medically vulnerable period and many cases of maternal mortality occur in the postpartum period.
While Medicaid pays for more than four in ten births and must cover pregnant women through 60 days postpartum, after that period states can and have made very different choices regarding whether eligibility for Medicaid coverage is continued. In states that have not expanded Medicaid under the Affordable Care Act (ACA), many women are left without a pathway to coverage and become uninsured just two months after giving birth. Recently, there has been growing interest from federal and state policymakers, clinicians, and health advocates in expanding Medicaid’s postpartum coverage from 60 days to one year. This brief discusses Medicaid’s eligibility for pregnancy and postpartum care, describes gaps in coverage particularly for low-income women who live in states that have not expanded Medicaid under the ACA, and highlights several state and federal efforts to extend postpartum coverage for a longer period of time.
What is Medicaid’s role for pregnancy and postpartum care?
Medicaid has long prioritized coverage of pregnant women and now finances more than four in ten births in the United States.2 Federal law requires that all states extend eligibility for pregnant women with incomes up to 138% of the federal poverty level (FPL); however, most states (48 and DC) go beyond this minimum threshold, ranging from 138% to 380% FPL. Pregnancy-related coverage must last through 60 days postpartum and the infant is eligible for Medicaid for the first year after birth. For women who qualify for Medicaid on the basis of pregnancy, all states provide pregnant women with a wide range of Medicaid benefits, including prenatal care, childbirth and delivery services. States have discretion to determine specific maternity care benefits under Medicaid. For example, many states cover substance use treatment and home visiting services but fewer cover other services such as doula care and home births.
For pregnant women who are eligible for Medicaid under the ACA’s Medicaid expansion pathway, states must cover all preventive services recommended by the United States Preventive Services Task Force (USPSTF) including many pregnancy-related services, such as prenatal screening tests and folic acid supplements as well as services in the postpartum period, such as lactation consultation and breastfeeding supplies. Importantly, all states cover family planning services before and after pregnancy. Pregnancy-related services for those enrolled under any Medicaid pathway are exempt from cost-sharing. For low-income people in particular, the lower cost sharing and absence of deductibles under Medicaid can be a major advantage over private insurance.
Where are the gaps in coverage during the postpartum period?
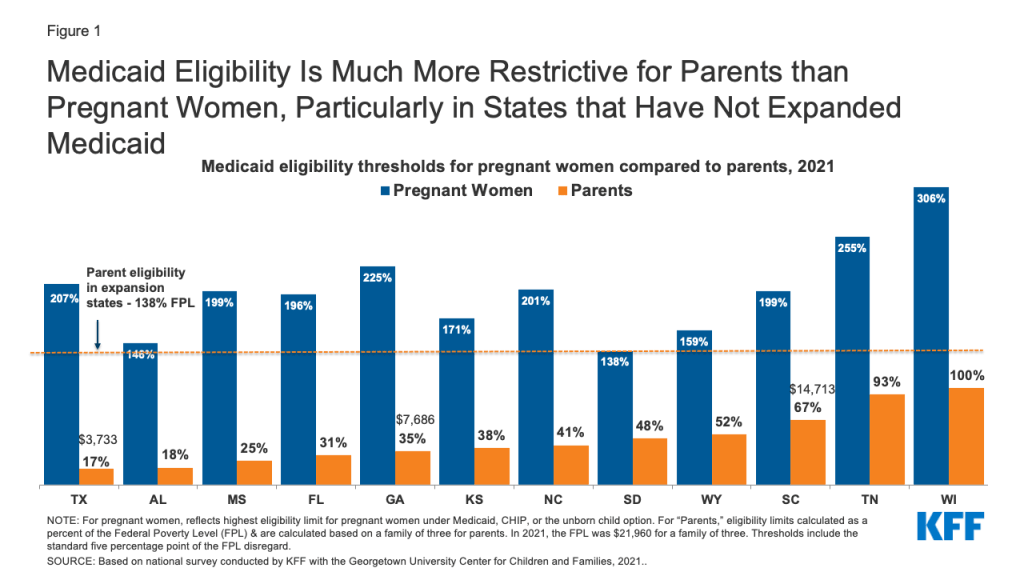
Following the 60 days postpartum period, mothers with incomes up to 138% FPL in the states that have expanded Medicaid under the ACA (38 states and DC) have a continued pathway to coverage. Those with incomes above 138% FPL may qualify for subsidized coverage through the ACA Marketplace. However, in the 12 states that have not adopted the ACA’s Medicaid expansion, postpartum women could qualify for Medicaid as parents to stay on the program, but Medicaid income eligibility levels for parents are much lower than for pregnant people in all of the states (Figure 1). As a result, many women in non-expansion states become uninsured after pregnancy-related coverage ends 60 days postpartum because, even though they are poor, their income is still too high to qualify for Medicaid as parents and too low to qualify for Marketplace subsidies. For example, in Texas, a married mother with a newborn loses Medicaid coverage two months after giving birth if she and her partner have an annual income above $3,733 (17% FPL).
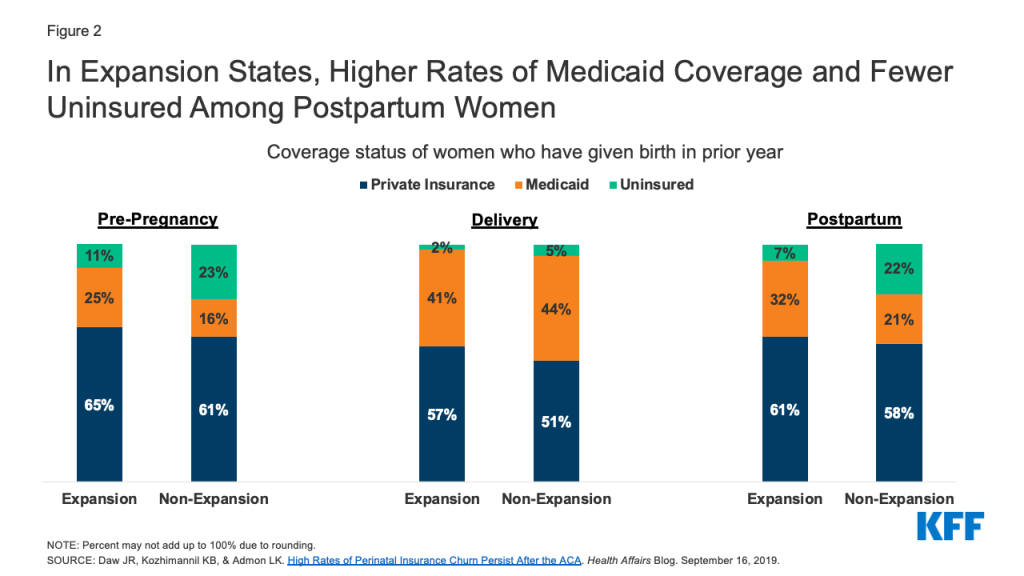
Research shows that Medicaid coverage is higher and uninsured rates are lower among women before and after pregnancy in expansion states compared to non-expansion states (Figure 2). As shown in Figure 2, coverage patterns are similar during pregnancy between expansion and non-expansion states. After pregnancy, however, Medicaid coverage declines and the uninsured rate climbs, with the effect more pronounced in non-expansion states.3
Furthermore, many women in non-expansion states who do not qualify for Medicaid after 60 days postpartum may also not qualify for subsidies to assist with the purchase of private insurance in state Marketplaces because they have incomes between the income limit for parents and 100% FPL, leaving them in the “coverage gap” with few options for affordable coverage.
How has the coronavirus affected postpartum coverage?
The Families First Coronavirus Recovery Act (FFCRA) includes an enhanced federal match (FMAP) to states, contingent on meeting maintenance of eligibility (MOE) requirements that include ensuring continuous coverage for enrollees until the end of the month in which the public health emergency (PHE) is in place. Under earlier guidance issued by the Centers for Medicare and Medicaid Services (CMS), someone qualifying on the basis of pregnancy would remain enrolled in that group, even after the 60 days postpartum period. Under a new interim final rule effective on November 2, states can move a pregnant woman from the pregnancy group to another eligibility pathway if eligible for another full benefit group, such as ACA expansion, and the benefit package for the new group is the same or more generous than the pregnant woman benefit package, move to new group. However, if the pregnancy benefit package is more generous than another pathway or the person is ineligible for any other full benefit group, they would remain enrolled in pregnancy group.
In addition to changing eligibility for coverage, the coronavirus pandemic has changed the way pregnancy and postpartum care is provided. New mothers may be more isolated from postpartum support, such as family members or doulas and women may be accessing services such as lactation consultations or postpartum checkups via telehealth. Continuity of coverage may be even more valuable given the other disruptions in care that new parents may be facing during the pandemic.4
Why is coverage for postpartum care important?
Postpartum care encompasses a range of important health needs, including recovery from childbirth, follow up on pregnancy complications, management of chronic health conditions, access to family planning, and addressing mental health conditions. While postpartum care has traditionally centered around one clinical visit six to eight weeks after delivery, there has been a paradigm shift to emphasize that postpartum care is an ongoing process that typically requires multiple visits and follow up care that may last a year or even longer. This is particularly important for those who experience pregnancy complications or have chronic conditions, such as hypertension or diabetes.
Mental health is a major concern during and after pregnancy. Suicidality among pregnant and postpartum people has risen over the past decade. At least one in ten women experience perinatal depression, and some studies suggest higher rates but poorer access to treatments among some communities of color and low-income women. ACOG recommends screening during the postpartum visit and initiation of treatment or referral to a mental health provider when a woman is identified with depression. This kind of care may be provided over a long duration, often lasting beyond 60 days.
Addressing pregnancy-related deaths (typically defined as death within one year of pregnancy)5 , particularly the substantially higher rates among Black and American Indian and Alaska Native (AIAN) women, is an urgent health challenge.6 At least one-third of maternal deaths occur in the postpartum period. Identifying the causes of maternal mortality and morbidity is complex, and coverage is only one factor, but research strongly indicates that access to health care throughout a woman’s reproductive years, is essential for prevention, early detection, and treatment of some of the conditions that place women at higher risk for pregnancy-related complications, including cardiovascular disease, diabetes, and chronic hypertension. Coverage disruptions during the perinatal period disproportionately affect Black, AIAN, and Hispanic women. Furthermore, a wide array of conditions that may present or persist through the postpartum period, including mental health challenges, intimate partner violence, and substance use, all play a role in maternal mortality and broader maternal health outcomes.
What can states do to extend postpartum coverage under Medicaid?
Assuring that low-income women have continuous coverage after pregnancy would support improvements in infant and maternal outcomes. States have several main pathways for broadening coverage in the postpartum period to Medicaid beneficiaries. These would all involve some increase in state spending, but with substantial federal matching funds available as well. Potential approaches, in decreasing order of scope and reach, include:
- Expand full scope Medicaid–Expanding Medicaid eligibility under ACA would provide the most comprehensive approach to broadening postpartum coverage, and the federal government would pay 90% of the costs for the expansion population. Postpartum women with incomes up to 138% FPL would be able to retain Medicaid past 60 days postpartum, providing greater continuity of coverage and care. Furthermore, other individuals with incomes up to 138% FPL would also qualify for Medicaid coverage, expanding Medicaid benefits to mothers and fathers as well as people without children, including those who intend to become pregnant and need preconception care. Research demonstrates the impact of Medicaid expansion on pregnancy-related coverage and care to date. One study found that Medicaid expansion was associated with lower maternal mortality rates compared to non-expansion states.7 Full Medicaid expansion would also narrow the coverage gap in non-expansion states for poor parents who do not qualify for either Medicaid or subsidies in the Marketplace. Research from the Urban Institute suggests that at least a quarter of uninsured new mothers would likely newly qualify for Medicaid postpartum if their state expanded Medicaid.
- Raise parental income eligibility levels under Medicaid– Short of full expansion, non-expansion states have another tool at their disposal to narrow the postpartum coverage cliff– raising income eligibility thresholds for parents, which is one of the pre-ACA eligibility categories. States set income eligibility levels for Medicaid. Raising the eligibility thresholds for parents could extend Medicaid eligibility to more low-income mothers and fathers and partially close the coverage gap in non-expansion states. Currently, Wisconsin sets eligibility thresholds for parents at 100% FPL and Tennessee is not far behind at 93% FPL (Table 1). The rest of the non-expansion states are much more restrictive however and currently have large gaps in coverage for parents. States would receive their regular federal match rate for any new enrollees who qualify as a result of higher parental eligibility levels.
- Extend pregnancy-related Medicaid coverage beyond 60 days postpartum– A number of states, both expansion and non-expansion, are taking action to try to extend the period of Medicaid postpartum eligibility, but the initiatives vary in scope.8 ,9 Some states are applying for Section 1115 waivers from CMS to extend Medicaid beyond 60 days postpartum. Georgia, a non-expansion state, enacted legislation to extend postpartum coverage from 60 days to six months for those who had a Medicaid funded birth, and the state has submitted a waiver application to CMS. Even in Medicaid expansion states, postpartum women may lose Medicaid coverage postpartum, particularly if their incomes are above 138% FPL, and need to transition to Marketplace insurance. Even with a premium subsidy, some may find the out of pocket costs unaffordable and they may have to change providers with a coverage transition. Some expansion states, such as Illinois and New Jersey, are also seeking waivers from CMS to extend Medicaid’s postpartum period so that low-income postpartum women at income levels above 138% FPL keep their Medicaid coverage beyond two months postpartum.
- Expand coverage for specific postpartum services or specific populations- There has been some interest in broadening Medicaid postpartum coverage for specific health needs. The HHS maternal health action plan recommends supporting policies that allow states to maintain coverage for pregnant and postpartum people with substance use disorders. The postpartum period can be a particularly susceptible time for substance use relapse, with loss of coverage and access to care considered a potential trigger for relapse. Missouri and Indiana have submitted waiver applications to CMS that propose Medicaid postpartum extension to 12 months for postpartum women in need of services for substance use. Missouri’s waiver would allow postpartum women to continue to receive substance use and mental health services for a year, while Indiana’s proposal would extend full Medicaid coverage for those with opioid use disorder. Additionally, both states participate in CMS’ Maternal Opioid Misuse (MOM) model, a funding initiative that the agency offers for states to develop and improve programs to care for pregnant and postpartum people with opioid use disorder..Some states have used state dollars to extend postpartum coverage to certain populations. California enacted legislation and is using state funds to extend Medicaid coverage to a year for postpartum individuals diagnosed with a maternal mental health condition. Since September 2020, the state of Texas has been using state funds to provide a limited package of postpartum services for one year to those enrolled in the state’s Healthy Texas Women program, which is for uninsured reproductive age women. The state has submitted a Section 1115 waiver application to CMS to draw down federal funds for this program.
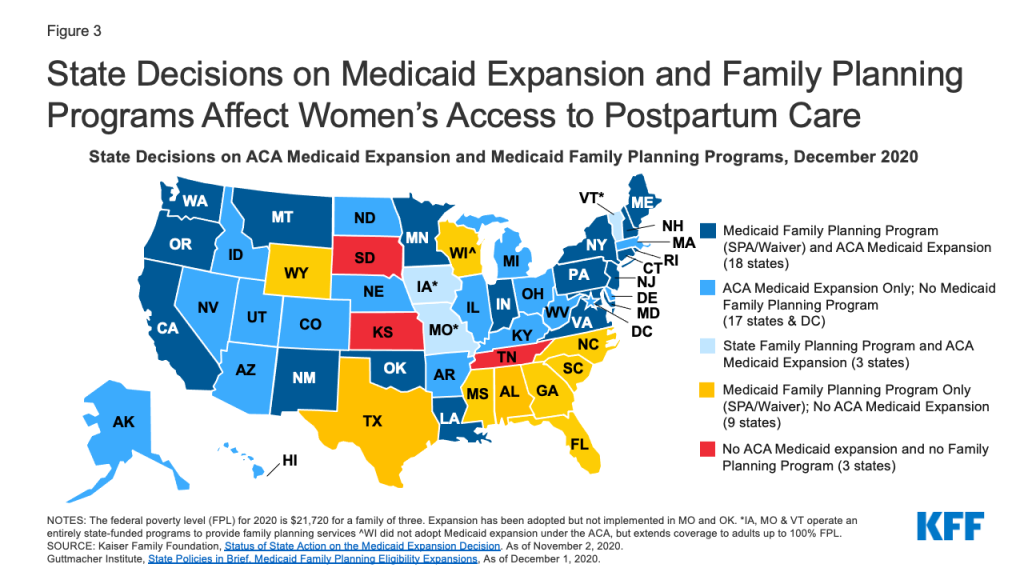
- Provide postpartum coverage for family planning services – Outside of lengthening the postpartum period under Medicaid, half of states provide Medicaid coverage for just family planning services to individuals who do not qualify for full Medicaid coverage. While these programs do not provide coverage that is as comprehensive as full scope Medicaid, they provide access to postpartum and intrapartum contraceptive services, which is important for pregnancy planning and healthy birth spacing. Most of the non-expansion states have a Medicaid or state-funded family planning program (Figure 3). However, in three states – Tennessee, Kansas, and South Dakota – postpartum individuals who were covered by Medicaid for pregnancy likely become uninsured after 60 days because the state has not expanded Medicaid under the ACA, and may not even have access to contraceptive services after pregnancy because the state does not have a Medicaid-funded family planning program.
What legislative proposals are currently being considered at the federal level to broaden postpartum coverage and strengthen maternity care?
In the 2019-2020 Congressional session, a number of federal bills related to maternal health care coverage, access, and quality are pending. Major themes across these bills include extension of Medicaid postpartum coverage to 12 months, coverage of doulas, greater support for state maternal mortality review committees, broadening provider networks in rural areas, and training on health equity and implicit bias for providers. Some notable federal bills that have garnered attention include:
- H.R. 4996 Helping Medicaid Offer Maternity Services (MOMS) Act of 2019 (sponsored by Rep. Robin Kelly), would amend the Medicaid program to allow states the option to extend continuous coverage with full benefits for postpartum individuals through one year postpartum. The bill was approved unanimously by voice vote in the House, and while many advocates and policymakers called for the Senate to pass the bill before the end of the 2019-2020 session, it was not passed.
- H.R. 1425, Patient Protection and Affordable Care Act Enhancement Act – This bill focuses on strengthening the ACA, but also includes a change to the postpartum period under Medicaid from 60 days to a full year. This differs from the Helping MOMS Act, which proposes a state option, while this bill requires mandatory 12 months postpartum coverage in all states. There would likely be significant differences in financing and access to care between proposals that create a mandatory expansion versus a state option, which some states would not adopt.10 A CBO analysis of the coverage extension in HR 1425 estimates a resulting $6 billion increase in the deficit over ten years. The bill passed the full House of Representatives in June 2020.
- H.R. 6142 – The MOMNIBUS is a package of nine bills sponsored by the Black Maternal Health Caucus in the House of Representatives and Vice-President elect Kamala Harris in the Senate. It is intended to improve different aspects of maternal health care for pregnant people, with a focus on health equity. Key components in the package include an extension of WIC benefits for one year postpartum, measures to diversify the perinatal workforce, funding to enhance maternal mortality committees and data collection, and mitigating the impact of social determinants of health. The MOMNIBUS has not yet been heard in a House committee.
Conclusion
As President-elect Biden, Vice President-elect Harris, and a new Congress come into office, maternal health, particularly large and persistent racial and ethnic inequities, continues to be a major health challenge. Coverage changes alone cannot address these issues, but given Medicaid’s large role in maternity financing and health coverage for communities of color, an extension of postpartum coverage for the full year after a Medicaid birth could provide stable coverage and care to more low-income birthing parents in both non-expansion and expansion states. For birthing parents, the need for health care services does not end two months after childbirth.
The ACA offers states the option to extend Medicaid eligibility to low-income parents with incomes up to 138% of the federal poverty level. However, in the 12 states that have not adopted full scope Medicaid expansion, most postpartum women lack a pathway to coverage and are at greater risk of becoming uninsured and losing access to critical health services in the postpartum and intrapartum periods. Some federal and state-level initiatives are in place to provide coverage for family planning or other more limited services to some reproductive age and postpartum people, but they do not provide the same level of coverage afforded by full scope Medicaid. Absent federal action, these decisions will continue to be in the hands of the states to decide whether to choose from among a number of pathways to expand coverage for new parents.
Table
Endnotes
- Black Mamas Matter Alliance, Policy Working Group. Advancing Holistic Maternal Care for Black Women Through Policy, December 2018. ↩︎
- Martin, et al. National Center for Health Statistics. “Births in the United States, 2019,” October 2020. ↩︎
- Daw, et al. High Rates of Perinatal Insurance Churn Persist After the ACA, Health Affairs, September 16, 2019. ↩︎
- Eckert, E. “Preserving the Momentum to Extend Postpartum Medicaid Coverage,” Women’s Health Issues, September 2020. ↩︎
- March of Dimes. Maternal Death and Pregnancy-Related Death, September 2019. ↩︎
- Howell, E. Reducing Disparities in Severe Maternal Morbidity and Mortality, Clinical Obstetrics and Gynecology, June 2018. ↩︎
- Eliason, E. “Adoption of Medicaid Expansion is Associated with Lower Maternal Mortality,” Women’s Health Issues, February 2020. ↩︎
- National Academy for State Health Policy (NASHP). States’ Efforts to Extend Medicaid Coverage to Postpartum Women. ↩︎
- American College of Obstetricians and Gynecologists (ACOG). Extend Postpartum Medicaid Coverage. ↩︎
- Heberlein, M. MACPAC. “Extending Postpartum Coverage.” December 10, 2020. ↩︎