In recent years, there has been a reduction in rates of teen pregnancy, births, and abortions. Similarly there has been a drop off in the share of adolescents engaging in sexual activity. Despite this shift, recent data indicate that the rates of unintended pregnancy and sexually transmitted infections (STIs) among teens and young adults remain higher in the U.S. than in other developed nations and are considerably higher among certain racial and ethnic minorities and in different geographic regions in the nation. This fact sheet provides key data on sexual activity, contraceptive use, pregnancy, prevalence of STIs, and access to reproductive health services among teenagers and young adults in the U.S.
Sexual Activity
- Nearly half (47%) of all high school students report ever having had sexual intercourse in 2013, a decline from 54% in 1991. A similar share of male and female students report ever having had sex (48% vs. 46%).1
- There are racial and ethnic differences in sexual activity rates. Black high school students are more likely to have had intercourse (60%) compared to White (44%) and Hispanic students (49%). A higher share of Black high school students (14%) and Hispanic students (6%) initiated sex before age 13 compared to White students (3%).2
- More than one in ten (13%) female teens and one in six (17%) male teens had more than four sexual partners in their lives. The percentage of high school students who report having had four or more sexual partners declined from 18% in 1995 to 15% in 2013.3
- One-third (34%) of high school students are currently sexually active, defined as having had sexual intercourse with at least one person in the previous three months. Almost one-quarter (22%) of these students reported using alcohol or drugs during their most recent sexual encounter. More males reported using alcohol or drugs (26%) compared to females (19%), and White males (28%) had higher rates than Black males (19%).4
- One in ten high school students who dated or went out with someone within the previous 12 months reported having experienced dating violence. More than 10% of students reported experiencing physical violence, and 10% of students reported experiencing sexual dating violence. Seven percent of students have been physically forced to have sexual intercourse, with more females (11%) than males (4%) reporting this experience.5 One in four women ages 15 to 24 report that they have talked with a health care provider about dating violence.6
- Young women experience the highest rates of rape and sexual assault among all age groups. More than 1 in 5 (22%) college women have been victims of physical abuse, sexual abuse, or threats of physical violence.7 Among women who have ever been raped, 30% were raped when they were between the ages of 11 and 17 and 37% were raped between the ages of 18 and 24.8
- “Sexting” is the exchange of explicit sexual messages or images by mobile phone. More than one in ten (13%) 14 to 24 year olds report having shared a naked photo or video of themselves via digital communication such as the internet or text messaging.9
- Twice as many young adults identify as lesbian, gay, bisexual, or transgender (LGBT) compared to older adults. A 2013 survey found 6.4% of adults ages 18 to 29 identified as LGBT compared to 3.2% of 30 to 49 year olds.10
Contraception
- Three quarters (74%) of teen girls reported learning about birth control in school.11 Half (50%) of teen girls ages 15 to 18 discussed contraception with a health care provider, compared to 77% of young adult women (ages 19 to 24).12 Among adolescents, 53% of females and 45% of males talked about contraception or STIs with their partner before their first time having sex.13
- 22% of teen females and 14% of teen males reported they did not use contraception at first intercourse.14 Research has shown that those who reported condom use at their sexual debut were more likely to engage in protective behaviors than those who did not report condom use at first intercourse.15
- Two thirds (66%) of sexually active teen males and half (53%) of teen females said they had used a condom at last sexual intercourse (Table 1).16
| Table 1: Types of contraceptives used by teens or by teen’s partner during last sexual intercourse, among teens ages 15-19 | ||||||
| Type of contraceptive | All teens, ages 15-19 | White, Non-Hispanic | Black, Non-Hispanic | Hispanic | Males | Females |
| Condom | 59.1% | 57.1% | 64.7% | 58.3% | 65.8% | 53.1% |
| Birth Control Pills | 19% | 25.9% | 8.2% | 9.0% | 15.1% | 22.4% |
| IUD/Implant | 1.6% | 1.9% | 1.1% | 1.3% | 1.3% | 1.8% |
| Shot/Patch/Ring | 4.7% | 4.8% | 5.7% | 4.3% | 3.7% | 5.6% |
| NOTE: Totals do not round to 100% because some teens may use more than one method and other teens do not use any methods. SOURCE: CDC. Youth Risk Behavior Surveillance System: US, 2013. MMWR, 63(-4). 2014. |
||||||
- 19% of currently sexually active high school students report that they or their partner used birth control pills to prevent pregnancy at last sexual intercourse. 17 White students (26%) were more likely to use birth control pills compared to Black (8%) and Hispanic (9%).18 Approximately 9% of teens used both condoms and one other method of contraceptive during last sexual intercourse.
- Emergency contraceptive (EC) pills can prevent pregnancy when taken within a few days of unprotected intercourse. One type of EC pill, Plan B, is available without a prescription in-front-of-the-counter without age restrictions. Other ECs, such as ella, are available with a prescription. Most teen girls age 15 to 18 (78%) report that they have heard of EC pills.19 From 2006 through 2010, 14% of female teens who had ever had sex had ever used EC pills.20
- The American Congress of Obstetricians and Gynecologists (ACOG) formally recommends long-acting reversible contraceptives (LARCs), such as intra-uterine devices (IUDs), for adolescents.21 LARCs are considered among the most effective forms of reversible contraception. However, utilization rates have been increasing. Approximately 7.4% of women aged 15 to 19 used a LARC in 2013, including an IUD, contraceptive patch, contraceptive implants, vaginal ring or injection.22
- IUDs have historically had high up-front costs with insertion and supplies typically costing between $500 and $1,000. The Affordable Care Act (ACA) requires most new private plans to cover many preventive services important for sexual health without cost sharing, including FDA approved prescribed contraceptive services and supplies for women.23 When financial barriers are removed, studies have shown a majority of women will choose LARCs which have the highest effectiveness rate.24
Pregnancy
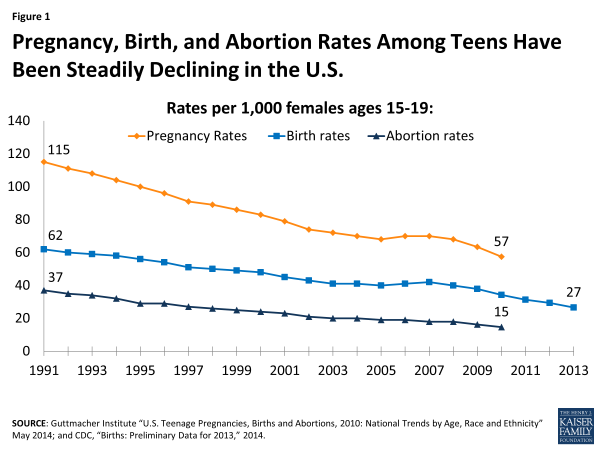
- The pregnancy rate among female teens ages 15 to 19 in 2010 was 57.4 per 1,000, a drop of more than 50% since the peak in 1990.25 Despite the decline in this rate over the past decade, the U.S. continues to have among the highest teen pregnancy, birth, and abortion rates in the developed world.26
- The teen birth rate has decreased significantly over the past decades, falling to 27 births per 1,000 females ages 15 to 19 in 2013 from 62 births per 1,000 females in 1991 (Figure 1).27
- Although birth rates have fallen for teens of all races and ethnicities, the rates for African American, Hispanic and Native American teens are over twice the rates of White and Asian American youth (Figure 2).
- There are also geographic differences in teen birth rates across the nation. In 2012, teen birth rates were highest in South Central states and lowest in the Northeast (Figure 3). The range varied considerably by state with New Mexico having the highest rate (47.5 births per thousand females 15 to 19) compared to a low in New Hampshire (13.8 births per thousand females 15 to 19).28 Teen birth rates have been declining in rural areas, but not as quickly as in suburban and urban areas.29
- The vast majority (82%) of teen pregnancies are unplanned compared to less than half of women above age 25.30 These teen pregnancies comprise more than one sixth of total unintended pregnancies annually in the U.S. and 36% of these unintended pregnancies end in abortion.31 Approximately 18% of women having abortions in the U.S. are teens and 33% are between the ages of 20 and 24.32 Women ages 15 to 19 comprised 17% of women of reproductive age (ages 15 to 44) in 2008.33
Sexually Transmitted Infections (STIs) and HIV/AIDS
- Compared to older adults, sexually active teens and young adults are at higher risk for acquiring STIs, due to a combination of behavioral, biological and cultural factors (Figure 4). Though they make up 25% of the sexually active population, they account for nearly half of new STI cases.34
- HPV is the most common STI among teens, with some estimates reaching an infection rate of 35% of 14 to 19 year olds.35 Currently, there are two vaccines (Gardasil and Cervarix) that protect against strains of HPV associated with cervical cancer and genital warts. The CDC recommends that all girls and women up to age 26 receive the 3 dose course of HPV vaccinations, as well as all boys up to age 21.36 These vaccines are now covered by private insurance without cost sharing, along with counseling on and screening for sexually transmitted infections, by the ACA’s policy for coverage of preventive services.37
- Teens ages 15 to 19 and young adults ages 20 to 24 accounted for the most reported cases of Chlamydia and Gonorrhea in 2012. Females are at greater risk than men of acquiring sexually transmitted infections, and the consequences include pelvic inflammatory disease, pregnancy complications, and infertility.38
- Despite the high rates of infection, many young women do not receive provider counseling on STIs. One-third of teen girls and almost half (45%) of young adult women ages 19 to 25 report that they have discussed STIs with their providers in the past three years.39
- Research has found that STI screening rates vary among youth. One study estimates that 37% of young men and 70% of young women ages 15 to 24 had an STI test in the past year.40 However, in another recent survey, more than half (56%) of young women who reported having an STI test incorrectly assumed it was a routine part of the exam, which is often not the case.41
- Over 34,000 young people, ages 13 to 24, were estimated to be living with HIV in the U.S in 2009.42 This age group accounts for 26% of new HIV infections. Most young people with HIV/AIDS were infected through sexual contact.43
- In 2013, 85% of high school students reported that they had been taught about AIDS or HIV infection in school.44 However, there are still gaps in knowledge about HIV/AIDS. One-third of teens ages 12-17 do not know that HIV is an STI.45
Access to Services
- Health insurance coverage and the ability to pay for services affect teens’ access to reproductive health care. Prior to many of the ACA insurance coverage benefits taking effect, approximately 25% of young adults 19 to 25 years old were uninsured and 15% were covered by Medicaid in 2012. Six in ten (61%) young adults lived in a low-income household (below 200% of the federal poverty level).46 After the initial insurance enrollment period in 2014, the uninsured rate among young adults ages 18 to 25 has declined to 18.7%.47
- Confidentiality is a priority for teens and young adults. In a national survey, 70% of women 19 to 24 rated confidentiality about use of health care such as family planning or mental health services as “important”; however, the majority of girls and women were not aware that insurers may send an explanation of benefits (EOB) that documents use of medical services that have been used to the principal policy holder, who may be a parent (Figure 5).48
- The Federal Title X program provides confidential contraceptive services and STI screening and treatment for low-income teens and young adults by funding approximately 4,400 clinics, public health departments and hospitals, available in 72% of US counties.49
- Currently, Medicaid funds 75% of publicly funded family planning services in the U.S.50 Family planning is a mandatory service under Medicaid and states are not permitted to charge cost-sharing for family planning services.
- Today, 21 states and DC have policies that explicitly allow minors to consent to contraceptive services, 25 allow consent in certain circumstances, and 4 have no explicit policy.51
- 38 states require some level of parental involvement in a minor’s decision to have an abortion, up from 18 states in 1991. 21 states require that teens obtain parental consent for the procedure, 12 require parental notification, and 5 require both.52
- Teen girls ages 15 to 19 seek information about sexual and reproductive health issues from a variety of sources, primarily family and friends (36%), websites (28%), or health care providers (21%) (Figure 6).53
Figure 5: Many Young Women Place a High Value on Confidentiality but are Unaware Private Plans can Send Explanation of Benefits (EOBs) to Parents
Figure 6: Teens Primarily Get Information on Sexual and Reproductive Health from Family and Friends, Websites, or Health Care Providers
Endnotes
- CDC. Youth Risk Behavior Surveillance System: US, 2013. MMWR, 63(-4). 2014.
- Ibid.
Ibid.
Ibid.
Ibid.
Kaiser Family Foundation, Women and Health Care in the Early Years of the ACA: Key Findings from the 2013 Kaiser Women’s Health Survey, May 2014.
The White House, “1 is 2 Many: Take Action Against Abuse.”
CDC. National Intimate Partner and Sexual Violence Survey, 2011.
AP/MTV Digital Abuse Study, 2011 (http://www.athinline.org)
Kaiser Family Foundation, Health and Access to Care and Coverage for Lesbian, Gay, Bisexual, and Transgender Individuals in the U.S., January 2014.
- Kaiser Family Foundation analysis of the 2013 Kaiser Women’s Health Survey.
Ibid.
Ryan, S. “Discussions About Contraceptions or STDs with Partners Before First Sex” PSRH, 39(3):149–157, 2007.
CDC. Teenagers in the United States: Sexual Activity, Contraceptive Use, and Childbearing, 2006-2010 National Survey of Family Growth. 2011.
Shafii T. Association between condom use at sexual debut and subsequent sexual trajectories: A longitudinal study using biomarkers. AJPH, 97(6). 2007.
CDC. Youth Risk Behavior Surveillance System: US, 2013. MMWR, 63(-4). 2014.
Ibid.
Ibid.
- Kaiser Family Foundation analysis of the 2013 Kaiser Women’s Health Survey.
CDC. Teenagers in the United States: Sexual Activity, Contraceptive Use, and Childbearing, 2006-2010 National Survey of Family Growth. 2011.
ACOG, Committee on Adolescent Health Care: Long-Acting Reversible Contraception Working Group, 2012.
- CDC. Youth Risk Behavior Surveillance System: US, 2013. MMWR, 63(-4). 2014.
In a June 2014 ruling, the Supreme Court limited the scope of the preventive services requirement and some employers may not need to abide by this requirement. For more information on preventive services now covered by the ACA, refer to the Kaiser Family Foundation fact sheet “Preventive Services Covered by Private Health Plans under the Affordable Care Act,” and for more information on the Supreme Court ruling, refer to “Potential Supreme Court Decision: Who Will Bear the Coverage ‘Burdens?’”.
Secura, G.M., et al. (2010). The Contraceptive CHOICE Project: Reducing Barriers to Long-Acting Reversible Contraception. American Journal of Obstetrics and Gynecology 203(2): 115.e1-115.e7.
Guttmacher Institute “U.S. Teenage Pregnancies, Births and Abortions, 2010: National Trends by Age, Race and Ethnicity” May 2014.
Guttmacher Institute. Teen Pregnancy and Lessons Learned, 2002.
CDC National Vital Statistics Reports, “Births: Preliminary Data for 2013”, 63(2)2014.
CDC National Vital Statistics Reports, “Births: Final Data for 2012”, 62(9)2013.
The National Campaign. Teen Childbearing in Rural America. January 2013.
Finer, LB & Zolna, MR. Shifts in intended and unintended pregnancies in the United States, 2001-2008. American Journal of Public Health 104: S43-S48, 2014.
Ibid.
Guttmacher Inst. Characteristics of U.S. Abortion patients, 2008. May 2010.
Ibid.
CDC. Sexually Transmitted Disease Surveillance. 2012.
CDC. Sexually Transmitted Disease Surveillance. 2012.
CDC.HPV Vaccine Information for Clinicians- Fact Sheet. 2012.
For more information on preventive services now covered by the ACA, refer to the Kaiser Family Foundation fact sheet Preventive Services Covered by Private Health Plans under the Affordable Care Act.
CDC. Reported STDs in the United States: 2012 National Data for Chlamydia, Gonorrhea, and Syphilis. 2014.
- Kaiser Family Foundation analysis of the 2013 Kaiser Women’s Health Survey.
- Cunningham, S. “Relationships Between Perceived STD-Related Stigma STD-Related Shame and STD Screening Among a Household Sample of Adolescents” PSRH, 2009.
- Kaiser Family Foundation analysis of the 2013 Kaiser Women’s Health Survey.
CDC. HIV/AIDS Surveillance in Adolescents and Young Adults,2012
Ibid.
- CDC. Youth Risk Behavior Surveillance System: US, 2013. MMWR, 63(-4). 2014.
MAC AIDS Fund, U.S. Teen Survey Headline Highlights, 2014.
- Kaiser Family Foundation analysis of Urban Institute tabs of ASEC supplement to CPS, 2013.
Gallup. In U.S., Uninsured Rate Sinks to 13.4% in Second Quarter, 2014.
- Kaiser Family Foundation analysis of the 2013 Kaiser Women’s Health Survey.
HHS Office of Population Affairs: Family Planning, Title X Family Planning.
- Guttmacher Institute. “The Central Role of Medicaid in the Nation’s Family Planning Effort”,2012.
- Guttmacher Institute. Minors’ access to contraceptive services. State Policies in Brief. 2013.
- Guttmacher Institute. Parental Involvement in Minors’ Abortions. State Policies 2013.
- Kaiser Family Foundation analysis of the 2013 Kaiser Women’s Health Survey.