Sexually Transmitted Infections (STIs): An Overview, Payment, and Coverage
Sexually transmitted infections encompass many different types of viral and bacterial infections. Every year, an estimated 20 million new sexually transmitted infections (STIs) are reported to the Centers for Disease Control and Prevention (CDC) in the United States. The rates of reported STIs reached record-breaking levels in 2018, continuing their recent rise. Despite these high rates, a 2019 KFF poll found that a large share of the public is unaware of how common STIs are, with less than half (36%) aware that STIs rates are increasing.
While all sexually active individuals are potentially at risk, rates are highest among 15-24 year olds, as well as gay and bisexual men. Black and Hispanic populations are also disproportionately affected relative to non-Hispanic White populations. Increasing rates of STIs highlight the importance of prevention, testing, treatment, as well as information and education, in curbing the transmission of these infections. This fact sheet examines trends and disparities in STI prevalence, reviews the STI screening and preventive care coverage policies for private insurance and public programs (including coverage gaps), and describes confidentiality in the provision of these services.
What are Sexually Transmitted Infections?
STIs are generally defined to include chlamydia, genital herpes, gonorrhea, hepatitis B, HIV, Human Papillomavirus (HPV), syphilis, and trichomoniasis . All STIs, including HIV, are preventable, and there are treatments to cure many, though not all, of them. Because some STIs often show no symptoms, at least initially, some people with an STI may not find out until more serious health concerns present. For this reason, preventive measures and routine screenings are important for the early identification of these infections in order to engage in treatment and to prevent further transmission and more serious complications.
Untreated STIs, particularly chlamydia and gonorrhea, can result in pelvic inflammatory disease (PID) in women and infertility. It is estimated that HPV, the most common STI in the United States, will be contracted at some point during the lifespan of nearly every sexually active individual. Most cases of HPV resolve on their own, but certain strains of HPV are linked to cervical, throat, penile, and anal cancers. The HPV vaccine protects against nine strains of this virus, including several that are associated with cancer.
Pregnant women with an untreated STI face increased risk of complications as do their infants. Exposure to an STI during pregnancy can result in preterm labor, low birth weight, premature rupture of membranes, and transmission to the infant during delivery. HIV and syphilis are particularly serious if transmitted to newborn infants. So long as a mother with HIV is engaged in consistent antiretroviral (ARV) treatment, it would be highly unlikely to transmit HIV to a baby. Up to 40% of babies born to women with untreated syphilis may be stillborn or die from the infection. Late or limited prenatal care has been associated with congenital syphilis (when the infection is present in utero or childbirth). Congenital syphilis is preventable in most cases, if women are screened for syphilis and treated early during prenatal care.
Prevalence of Sexually Transmitted Infections
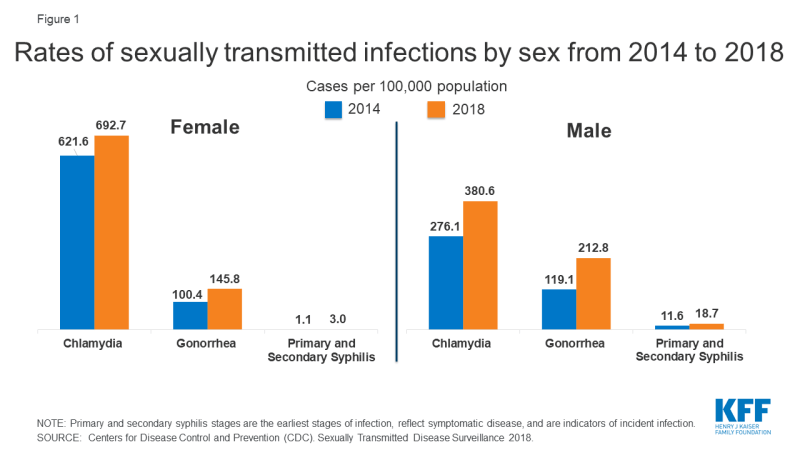
While women still account for the highest reported cases of STIs (driven mainly by high numbers of chlamydia in women), men, in particular gay and bisexual men, saw greater increases in rates of syphilis, chlamydia, and gonorrhea in recent years. Syphilis infection rates nearly doubled among men from 2014 to 2018 (Figure 1).
| Table 1: Sexually Transmitted Infection Rates of Reported Cases, by Selected Characteristics, 2018 Rate per 100,00 population |
||||||
| Gonorrhea | Chlamydia | Syphilis (primary and secondary stages) | Congenital Syphilis | HIV | ||
| U.S. Total | 179.1 | 539.9 | 10.8 | 33.1 | 11.4 | |
| Sex | Men | 212.8 | 380.6 | 18.7 | NR | 22.5 |
| Women | 145.8 | 692.7 | 3 | NR | 5.1 | |
| Race | White | 71.1 | 212.1 | 6 | 13.5 | 4.9 |
| Black | 548.9 | 1192.5 | 28.1 | 86.6 | 39.3 | |
| Hispanic | 115.9 | 392.6 | 13 | 44.7 | 16.2 | |
| Asian/Pacific Islanders | 35.1 | 132.1 | 4.6 | 9.2 | NA | |
| American Indian/Alaska Native | 329.5 | 784.8 | 15.5 | 79.2 | 7.8 | |
| Age | 15-19 | 432.4 | 2110.6 | 7.7 | NR | 8 |
| 20-24 | 713 | 2899.2 | 27.8 | NR | 27.6 | |
| 25-29 | 553.6 | 1427.3 | 33 | NR | 32.5 | |
| 30-34 | 366.4 | 701.5 | 26.9 | NR | 25.6 | |
| Region | Northeast | 138.4 | 492.1 | 8.7 | 8.5 | 10 |
| South | 194.4 | 565.2 | 11.1 | 12.4 | 15.7 | |
| Midwest | 184.5 | 524 | 7.1 | 44.7 | 7.2 | |
| West | 179.7 | 548.5 | 15 | 48.5 | 9.3 | |
|
NOTES: NR is Not Reported. Primary and secondary syphilis stages are the earliest stages of infection, reflect symptomatic disease, and are indicators of incident infection.
SOURCE: Centers for Disease Control and Prevention (CDC), Sexually Transmitted Disease Surveillance 2018; CDC, Diagnoses of HIV Infection in the United States and Dependent Areas, 2018.
|
||||||
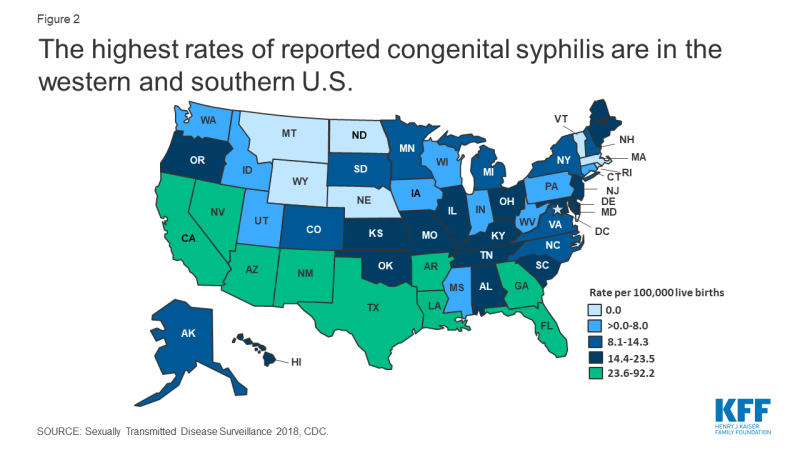
Congenital syphilis rates increased 173% between 2014 and 2018, with the number of cases the highest they have been since 1995. The highest rates of congenital syphilis were in the South, West, and Southwest (Figure 2).
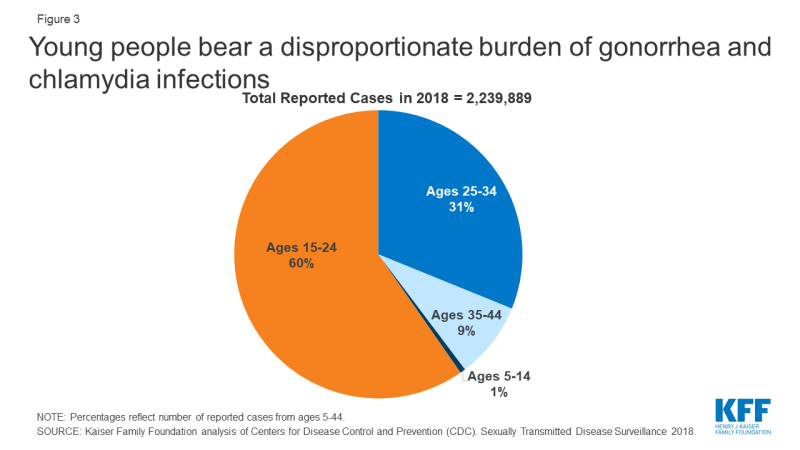
STIs also have a disproportionate impact on young people, ages 15-24, who acquire half of all new STIs, despite only representing 25% of the sexually active population (Figure 3). Young people, ages 15-24, account for 60% of all reported cases of gonorrhea and chlamydia.
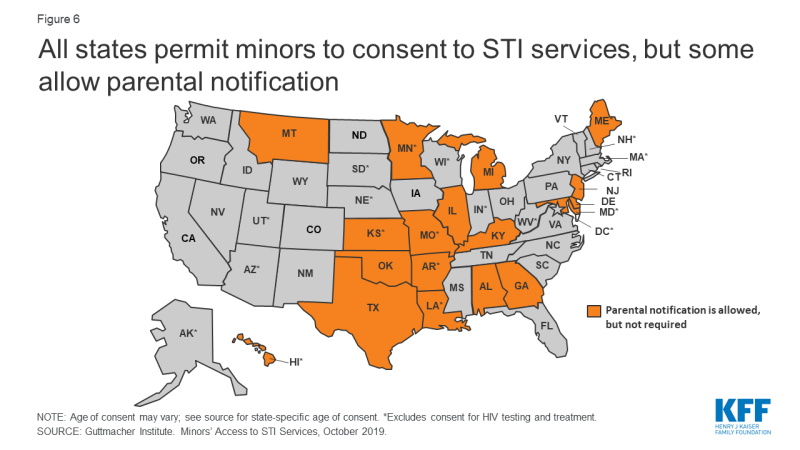
Due to a combination of social, structural, and economic inequities, HIV and other STIs disproportionately affect certain groups (Figure 4). In 2018, Blacks accounted for 38% of reported gonorrhea cases and 33% of primary and secondary syphilis cases, despite comprising just 13% of the population. Blacks also accounted for 42% of new HIV diagnoses in the U.S in 2018. Hispanics are also disproportionately affected, accounting for 27% of persons newly diagnosed with HIV and representing 18% of the population in 2018.
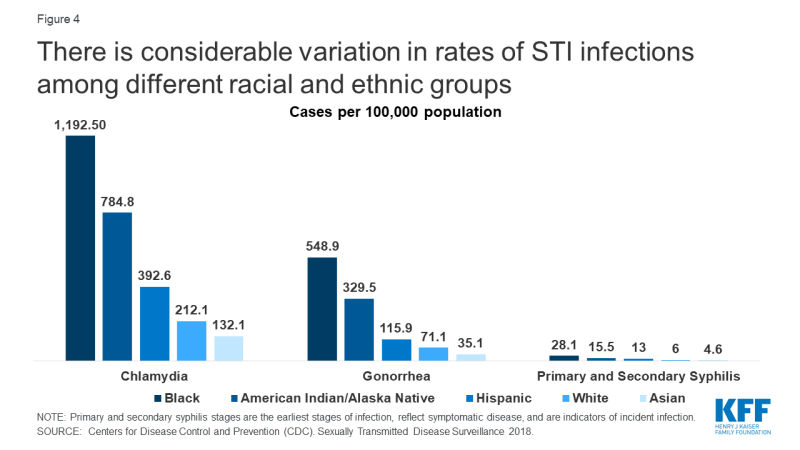
Figure 4: There is considerable variation in rates of STI infections among different racial and ethnic groups
Gay and bisexual men of all races have also been disproportionately affected since the start of the HIV/AIDS epidemic. In 2018, men who have sex with men (MSM) accounted for more than two thirds (69%) of all HIV diagnoses in the U.S., representing 86% of cases among males. MSM also accounted for 78% of male primary and secondary syphilis cases in 2018.
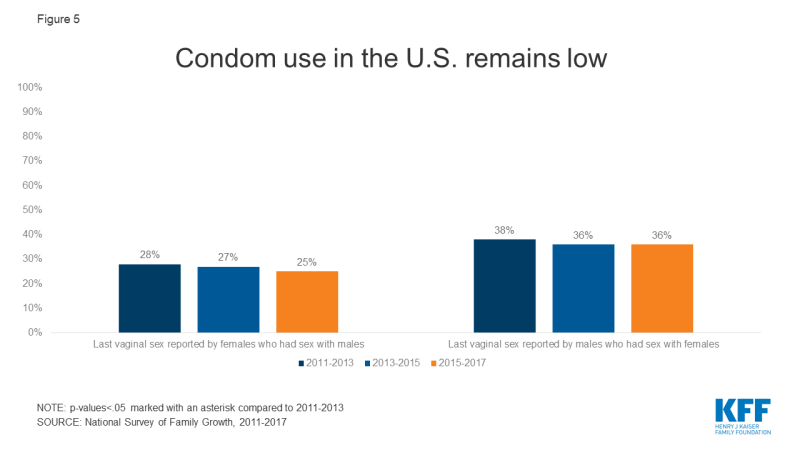
The higher prevalence of HIV and other STIs in certain communities can mean risk of exposure is also greater in these communities, particularly when sexual networks are close-knit. When used correctly, condoms are effective at preventing the transmission of HIV and other STIs. However, condom use in the U.S. remains low (Figure 5. Pre-exposure prophylaxis (PrEP), a daily pill approved by the FDA in 2012, reduces the risk of sexually contracting HIV by up to 99% among people at high risk.
Expedited Partner Therapy
Many states have laws allowing expedited partner therapy (EPT), which permits the treatment of partners of patients diagnosed with an STI without examination. The CDC has recommended this practice since 2006 in certain circumstances due to its success in reducing gonorrhea reinfection rates. Currently 39 states and DC allow physicians to provide at least some treatment to the partner of a patient diagnosed with a STI. Among publicly funded clinics, 79% provided expedited therapy for the patient’s partner at the same visit in 2015. However, even in states where EPT has been legalized, many do not allow the patient’s insurance coverage to be billed for the partner’s treatment, which can create a financial barrier to care.
Paying for STI Prevention and Treatment Services
Access to prevention, screening, testing and treatment services for STIs is facilitated by private insurance, public coverage such as Medicaid and Medicare, as well as publicly-supported health programs. The CDC estimates that in 2008 (the most recent estimate available), the annual direct medical costs in the US associated with STIs (including HIV) were nearly $16 billion.
Private Insurance
The Affordable Care Act (ACA) requires most private health insurance plans to cover recommended preventive services, including HIV and other STI screening, with no cost sharing. For adults, this includes US Preventive Services Taskforce (USPSTF) recommendations receiving an A or B grade, which include vaccines recommended by the CDC’s Advisory Committee for Immunization Practices, and services for women recommended by the Health Resources and Services Administration (HRSA). STI-related services that must be covered without cost-sharing by most plans are presented in Table 2.
In June 2019, the USPSTF Task Force added an A grade recommendation for PrEP for the prevention of HIV in high-risk populations, which means that most insurance plans must begin covering the full cost of the drug in the plan year that starts after June 2020. CDC guidelines on PrEP advise that individuals on PrEP have follow up visits and lab work, including being re-tested for HIV four times a year, but it is unclear whether these follow-up visits and lab work must be covered without cost-sharing by most insurance plans.
Plans are also required to cover prescription contraceptives for women, so coverage for female condoms would be required if an enrollee has a prescription but not when purchased over the counter. Twelve states (CA, CT, DE, IL, MD, MA, NJ (will apply to insurance plans in April 2020), NM, NV, NY, OR, WA) and DC currently require insurance coverage for over-the-counter contraceptive methods – of these however– 8 states (CA, DE, IL, MD, MA, NJ, NV, OR) exclude male condoms.
Medicaid
Medicaid, the national health coverage program for low-income individuals, is financed and operated jointly by the federal and state governments. For the 37 states and DC that have expanded Medicaid, STI counseling, screenings, preventive vaccinations, and PrEP must be covered at no cost for the newly eligible populations under the ACA just as they are for enrollees in private insurance plans (Table 2). However, this requirement does not apply to populations covered by Medicaid through other pathways, where coverage for specific STI screenings and treatments is determined by the state.
Some states extend access to STI services through limited-scope Medicaid family planning programs that provide Medicaid coverage solely for family planning services to women and men who do not qualify for full Medicaid benefits. Most of these programs cover STI screenings, but not all cover treatment if diagnosed. While all state Medicaid programs must cover medically necessary HIV testing, state coverage of routine HIV screening varies because it is an optional benefit under Medicaid. While several states cover condoms, they require prescriptions for this over-the-counter product. Medicaid is the largest public funder of HIV treatment and care, and all state Medicaid programs should cover PrEP.
| Table 2: STI-related Preventive Care Benefits that Plans Must Cover without Cost-Sharing | ||||
| Men who are sexually active or at higher risk | Women who are sexually active or at increased risk | Pregnant women | Young people | |
| Gonorrhea screening | X – sexually active women <24 years, and older women at increased risk | X (for those at increased risk | ||
| Chlamydia screening | X – sexually active women <24 years, and older women at increased risk | X – under 25 | ||
| Syphilis screening | X | X | X | |
| HPV DNA Testing | X – 30 years and older | |||
| HPV vaccine | X – 11 to 26 years | X – 11 to 26 years | X – 11 to 26 years | |
| Hepatitis B screening | X | X | X – at first prenatal visit | X |
| Hepatitis B vaccine | X | X | X – children under 18 years | |
| STI prevention counseling | X | X | X – if sexually active | |
| HIV screening and counseling | X – all aged 15 to 65 years, all others at higher risk | X – all aged 15 to 65 years, all others at higher risk | X | X |
| PrEP | X – all at high risk of HIV acquisition | X – all at high risk of HIV acquisition | X – all at high risk of HIV acquisition | X – all at high risk of HIV acquisition |
| Pap Test (cervical cancer screening) | X – All women ages 21 to 65 | |||
|
NOTES: Population covered and definition of high risk vary by condition. Coverage without cost sharing required in new private plans and Medicaid expansion groups.
SOURCE: Kaiser Family Foundation, Preventive Services Tracker, October 2019.
|
||||
Medicare
Medicare plays a key role in providing health coverage to 60 million people 65 and older as well as younger people with long-term disabilities. The ACA also requires Medicare to cover preventive services that are rated “A” or “B” by the USPSTF without cost-sharing. Medicare Part B (Medical Insurance) covers STI screenings for chlamydia, gonorrhea, syphilis, and/or Hepatitis B once every 12 months for individuals at increased risk for an STI or at certain times during pregnancy for pregnant individuals. Medicare also covers up to two individual 20-30 minute, face-to-face, high-intensity behavioral counseling sessions once each year for sexually active individuals at increased risk for STIs. Additionally, Medicare covers an HIV screening once per year for individuals age 15-65 without regard to perceived risk or for individuals outside of this age range who are at an increased risk for HIV. Medicare Part D is required to cover all approved antiretrovirals (one of “six protected” drug classes), which includes PrEP, but unlike most preventive services covered under Part B, plans are allowed to charge cost sharing for these drugs.
Services and Programs for Uninsured Individuals
Roughly 28 million people, 9% of the population, were uninsured in 2018. A patchwork of public-supported clinics and program make STI services available to uninsured individuals. STI programs funded by federal, state, and local governments, such as those that receive funding from various federal agencies such as HRSA, the CDC, or the Office of Population Affairs (OPA), are important sites of care for STI prevention and treatment, especially, those who are under- or uninsured. As part of the safety-net healthcare network, health centers and health departments provide low-income individuals with free or low-cost care, including counseling, testing, diagnosis and treatment. Research suggests that clinicians at these clinics are also more likely to provide routine STI care and discuss the use of condoms with patients than private providers.
The federal Title X family planning grant program, administered by OPA, also provides support to clinics to serve low-income and uninsured individuals in need of STI screening and treatment. In the past year, however, the network of clinics participating in the program has shrunk significantly. About one in four Title X funded sites have withdrawn from the program in response to the Trump Administration’s new regulations that block Title X support to clinics that provide abortion services and referrals in addition to family planning and STI services. The organizations that no longer participate in the program have not only lost funding available to provide low-income individuals with contraceptive services, but also may have had an impact on the availability of STI testing and treatment services in many communities.
For people living with HIV, the Ryan White HIV/AIDS Program works with health departments and local community-based organizations to provide HIV medical care and other support services for people living with HIV who have no insurance or are underinsured.
The AIDS Drug Assistance Program or ADAP is part of the Ryan White HIV/AIDS Program. It helps covers the cost of HIV-related prescription medications for low- to moderate- income people who have limited or no prescription drug coverage. Each state operates its own ADAP, so eligibility and program elements can vary state to state.
Gilead, the manufacturer of Truvada and Descivy, the PrEP medications, offers a Medication Assistance Program for PrEP that may provide the medication at no cost based on income, but does not cover the cost of the medical visits or the recommended lab testing. The program may also be available to those on Medicare who do not have Part D prescription drug coverage. In addition, some city and state health departments, and foundations offer navigation and other support services, as well as financial assistance to make PrEP free or low cost. In December 2019, the U.S. Department of Health and Human Services launched the Ready, Set, PrEP program, which makes PrEP prescriptions available at no cost to 200,000 at-risk, uninsured individuals each year for up to 11 years. The program does not support required labs and medical services, which can be expensive. This new program is still in early implementation stages.
Confidentiality
Confidentiality is a crucial factor in the provision of STI screening and treatment services. For minors in particular, it can be a challenge. Although all 50 states and DC allow minors to consent to STI services, 18 states allow physicians to inform a parent or guardian that the minor is seeking these services (Figure 6).
Confidentiality has long been a fundamental principle of the Federal Title X family planning program; however, the Trump Administration’s new final regulations for the Title X program also have broadened its requirements to encourage family participation, require documentation of the specific actions taken to encourage family participation (or the specific reason why family participation was not encouraged) in minor’s records, and to document the age of the minor’s sexual partner. While the impact of this regulation on minors’ willingness to seek care at a Title X clinic has not yet been evaluated, there is concern that this new requirement will deter minors from seeking services because of their concerns about confidentiality.
Another confidentiality concern resulted from the ACA provision that allows dependents to remain covered under their parent’s plan up to the age of 26. In 2018, approximately 11.1 million young adults aged 19-25 were covered as dependents in an employer-sponsored insurance policy.1 Although this policy has expanded coverage for young adults, it has raised concerns about privacy and confidentiality in the use of sensitive health services such as STI screening and treatment for young adults covered as dependents. According to a 2013 Kaiser Family Foundation survey, 71% of women ages 18 to 25 rated confidentiality as important to them, but only 37% understood that an Explanation of Benefits (EOB) summary is sent to the primary policyholder (typically the parent) when health services are used.
However, seven states (CA, CO, HI, MD, ME, OR, and WA) have implemented broad laws to ensure confidentiality for minors seeking sensitive services such as STI screenings. Some states (CA, MD, and OR) require insurers to provide confidential communications upon the written request of the covered dependent, including minors. Other states (HI and ME) offer broader protections from disclosure of health information without the consent of the minor. Some states (CT, DE, and FL) have laws focusing specifically on the disclosure of STI treatment without a minor’s consent, including in the billing process.
Conclusion
High rates of STIs continue to be a public health concern. Women, people of color, and youth experience the highest rates of reported infections. Gay and bisexual men account for the majority of the increase between 2000 and 2018. The general public, however, appears to be unaware of the how commonly STIs occur and that their incidence is on the rise.
Publicly funded clinics, many funded by the CDC, OPA’s Title X program, and HRSA’s Ryan White program, including health centers, state and local health departments, STI clinics, and Planned Parenthood clinics, provide confidential STI and HIV care to at-risk and uninsured populations. With the passage of the ACA, most private health insurance plans and Medicaid expansion programs are now required to cover HIV and STI counseling and screening without cost sharing. In addition to coverage, access to and the availability of STI/HIV care will likely depend on a number of factors, including public funding for safety-net providers, adoption of practices aimed at the reduction of transmission such as patient education, expedited partner therapy, consistent routine screenings and treatment, as well as proximity to providers.
| Appendix Table 1: Number of Reported Sexually Transmitted Infections, 2018 | ||||||
| State | Chlamydia Cases | Gonorrhea Cases | Syphilis (Primary and Secondary) Cases |
Congenital Syphilis Cases | HIV Prevalence (2017) | HIV Diagnoses |
| Alabama | 28,437 | 12,742 | 477 | 7 | 13,124 | 572 |
| Alaska | 6,159 | 2,247 | 55 | 1 | 720 | 20 |
| Arizona | 40,807 | 12,870 | 1,047 | 61 | 16,062 | 806 |
| Arkansas | 17,663 | 7,300 | 288 | 25 | 5,634 | 281 |
| California | 231,415 | 79,192 | 7,607 | 332 | 128,153 | 4,398 |
| Colorado | 29,124 | 8,894 | 337 | 7 | 12,352 | 409 |
| Connecticut | 16,732 | 4,959 | 91 | 2 | 10,328 | 250 |
| Delaware | 6,038 | 1,691 | 30 | 0 | 3,285 | 91 |
| DC | 9,014 | 4,240 | 279 | 0 | 14,316 | 208 |
| Florida | 104,758 | 32,644 | 2,880 | 108 | 110,034 | 4,683 |
| Georgia | 65,936 | 20,867 | 1,607 | 31 | 52,528 | 2,552 |
| Hawaii | 7,735 | 1,495 | 92 | 4 | 2,524 | 66 |
| Idaho | 6,572 | 1,134 | 46 | 1 | 1,145 | 37 |
| Illinois | 77,325 | 25,422 | 1,408 | 29 | 35,076 | 1,352 |
| Indiana | 34,926 | 12,193 | 367 | 1 | 11,218 | 510 |
| Iowa | 14,682 | 4,839 | 86 | 3 | 2,671 | 116 |
| Kansas | 14,231 | 5,256 | 152 | 8 | 2,997 | 154 |
| Kentucky | 19,440 | 7,470 | 366 | 9 | 7,108 | 360 |
| Louisiana | 36,293 | 12,043 | 669 | 46 | 20,424 | 986 |
| Maine | 4,345 | 710 | 74 | 0 | 1,576 | 28 |
| Maryland | 35,482 | 10,305 | 737 | 29 | 32,436 | 979 |
| Massachusetts | 30,460 | 8,076 | 552 | 0 | 20,374 | 654 |
| Michigan | 50,592 | 16,688 | 649 | 13 | 15,667 | 718 |
| Minnesota | 23,569 | 7,542 | 292 | 10 | 8,304 | 283 |
| Mississippi | 22,086 | 9,749 | 464 | 3 | 9,399 | 479 |
| Missouri | 34,728 | 15,090 | 806 | 17 | 12,308 | 446 |
| Montana | 4,917 | 1,181 | 45 | 0 | 625 | 23 |
| Nebraska | 8,026 | 2,696 | 119 | 0 | 2,136 | 79 |
| Nevada | 17,508 | 6,475 | 682 | 31 | 9,609 | 508 |
| New Hampshire | 3,734 | 594 | 64 | 1 | 1,189 | 36 |
| New Jersey | 36,514 | 9,067 | 570 | 13 | 34,891 | 1,044 |
| New Mexico | 14,000 | 5,268 | 304 | 10 | 3,428 | 121 |
| New York | 119,571 | 37,262 | 2,654 | 28 | 126,495 | 2,470 |
| North Carolina | 66,553 | 23,725 | 1,098 | 17 | 30,953 | 1,200 |
| North Dakota | 3,525 | 1,369 | 41 | 0 | 407 | 36 |
| Ohio | 63,220 | 25,146 | 740 | 20 | 21,899 | 984 |
| Oklahoma | 21,974 | 8,998 | 531 | 12 | 6,084 | 234 |
| Oregon | 19,224 | 5,913 | 424 | 10 | 6,879 | 230 |
| Pennsylvania | 59,340 | 15,887 | 797 | 9 | 35,520 | 1,002 |
| Rhode Island | 5,487 | 1,336 | 96 | 0 | 2,547 | 76 |
| South Carolina | 33,910 | 13,801 | 384 | 9 | 16,858 | 719 |
| South Dakota | 4,432 | 1,689 | 41 | 1 | 568 | 28 |
| Tennessee | 38,212 | 14,627 | 553 | 12 | 16,612 | 759 |
| Texas | 146,510 | 47,231 | 2,538 | 367 | 88,099 | 4,483 |
| Utah | 10,541 | 2,895 | 169 | 1 | 2,757 | 121 |
| Vermont | 1,712 | 268 | 11 | 0 | 693 | 18 |
| Virginia | 42,965 | 11,776 | 702 | 9 | 22,149 | 867 |
| Washington | 34,449 | 11,207 | 802 | 7 | 13,205 | 503 |
| West Virginia | 3,599 | 1,143 | 65 | 1 | 1,810 | 85 |
| Wisconsin | 28,027 | 7,882 | 152 | 1 | 6,216 | 210 |
| Wyoming | 2,169 | 311 | 23 | 0 | 326 | 12 |
| Sources: Centers for Disease Control and Prevention (CDC). 2018 Sexually Transmitted Diseases Surveillance. Atlanta: U.S. Department of Health and Human Services, October, 2019. CDC, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (HCHHSTP) AtlasPlus, accessed February 2019. | ||||||
Endnotes
Kaiser Family Foundation estimates based on the Census Bureau's American Community Survey, 2018.