The independent source for health policy research, polling, and news.
VOLUME 17
Race-Based Vaccine Myths Spread Amid Measles Outbreaks
This is Irving Washington and Hagere Yilma. We direct KFF’s Health Information and Trust Initiative and on behalf of all our colleagues at KFF, we’re pleased to bring you this edition of our bi-weekly Monitor.
Summary
This volume discusses the spread of race-based vaccine myths amid measles outbreaks, along with shifts in health communication from fact-checking to fostering open dialogue. It also explains common misconceptions about heart attack treatment and prevention, a new scientific journal that questions established science, and gaps in research standards for AI chatbots used in healthcare.
Recent Developments
Race-Based Vaccine Myths Spread Amid Measles Outbreaks
As a measles outbreak in Texas worsens and other cases are reported in the country, misinformation about vaccines continues to spread, influencing public perception and fueling hesitancy. One recurring narrative falsely claims that Black children should follow a different vaccine schedule than children of other races because of alleged differences in immune systems. Some research has shown that people of African descent may demonstrate, on average, a stronger immune response to the rubella vaccine. However, the study’s authors state that the data does not support that there is a need for different vaccine schedules based on race. The claim spread in news and social media after it was brought up during Robert F. Kennedy Jr.’s Senate confirmation hearings, with social media posts both debunking and supporting this narrative.
One of the most popular social media posts on the topic came from Senator Angela Alsobrooks, who shared a video clip on X of her asking Kennedy about these claims during the confirmation hearing and expressing her concern about the dangers of this narrative. The post received approximately 164,000 likes and 30,000 reposts, and 15,000 comments as of February 19. While many commenters shared Alsobrooks’ concern, some perpetuated the misconception that biological differences in vaccine safety are supported by evidence. In some instances, commenters cited cases in which race-based medicine is used in other domains as justification for biological differences in medication effectiveness. But scientists have emphasized that race is a social construct, not a biological category, and using it as a proxy for genetics has led to harmful medical practices.
Despite decades of credible research showing that vaccines are not associated with autism, narratives linking vaccines to autism in Black children have also gained traction, sometimes citing a retracted study of 2004 CDC data. The study, which claimed that Black boys who received the MMR vaccine on schedule were diagnosed with autism at higher rates than other children who did not receive the vaccine on time, was retracted due to flawed methods and the lead author’s undisclosed ties to the anti-vaccine group, Children’s Health Defense. Other claims that vaccines cause autism cite a debunked study, commonly referred to as the “Mawson Study”, which is not about race-related risk but reports an alleged connection between vaccines and autism. However, the study was not published in a peer-reviewed journal, was funded by an anti-vaccine group, and authored by researchers with a history of publishing vaccine-related research that was later retracted. This belief, alongside other unfounded concerns about vaccine safety, may be fueling the decline in childhood vaccination rates, which has led to outbreaks of vaccine-preventable diseases like measles.
Polling Insights:
KFF’s January 2025 Tracking Poll on Health Information and Trust found that majorities of parents say they keep their children up to date on vaccinations (82%), support public schools requiring vaccines for students (76%), and believe the benefits of childhood MMR vaccines outweigh the risks (72%). While majorities of parents across partisanship express each of these views, the shares answering in the pro-vaccine direction are notably larger among parents who identify as Democrats or lean that way, compared to their Republican and Republican-leaning counterparts.
The Field of Health Communication Explores Moving Beyond Fact-Checking to Foster Dialogue
Some health communication professionals are shifting their approach to promoting accurate health beliefs, moving beyond reactive fact-checking to open conversations that help people weigh benefits and risks more accurately. One emerging strategy, known as bypassing, focuses on presenting relevant facts rather than directly debunking misinformation. For example, instead of stating that “aluminum in vaccines causes bone problems” is false, bypassing highlights that “the aluminum in vaccines enhances their effectiveness in preventing disease.” Research suggests this approach may be more effective at changing personal attitudes, though its impact on policy views is less clear. Fostering open conversations may also allow health professionals to share nuances of scientific information in an accessible manner. For topics like vaccines, simply emphasizing their safety and effectiveness may not be enough as it fails to address public concerns and skepticism. Members of the Council for Quality Health Communication argue that the phrase “safe and effective” should be replaced with a more nuanced, empathetic approach that explains vaccine benefits in relatable terms, acknowledges uncertainties, and engages with people in ways that resonate with their real-world experiences and values.
New Public Health Journal Co-Founded by Nominee for NIH Director Questions Widely Accepted Science
A new scientific journal, the Journal of the Academy of Public Health, has drawn attention for its potential bias and questioning of scientific consensus. The journal has ties to the news site RealClearPolitics and was co-founded by Dr. Jay Bhattacharya, President Trump’s nominee for NIH director. Another Trump nominee, Dr. Marty Makary, nominee for FDA commissioner serves on the editorial board, although both Makary and Bhattacharya are currently listed as “on leave” from the journal. Its first edition included articles that questioned COVID-19 vaccine trials, suggested a link between DTaP vaccines and childhood asthma, and argued school mask mandates were ineffective. Co-founder Dr. Martin Kulldorff, known for opposing COVID-19 lockdowns and child vaccination, also published a paper claiming that established journals suppress dissenting viewpoints and fail to address public health biases. While the journal’s critiques may appeal to those questioning the prevailing public health consensus, some question its objectivity. The journal is open-access and peer reviewed, but it operates on a membership model where only invited members of the Academy of Public Health can submit articles, which may raise additional questions about how this exclusivity may impact credibility. However, the journal’s divergence from scientific consensus may increase its credibility among Republicans who are less likely than Democrats to list scientific research studies among their top trusted sources for public health information, according to the Rollins-Gallup Public Health Priorities Survey.
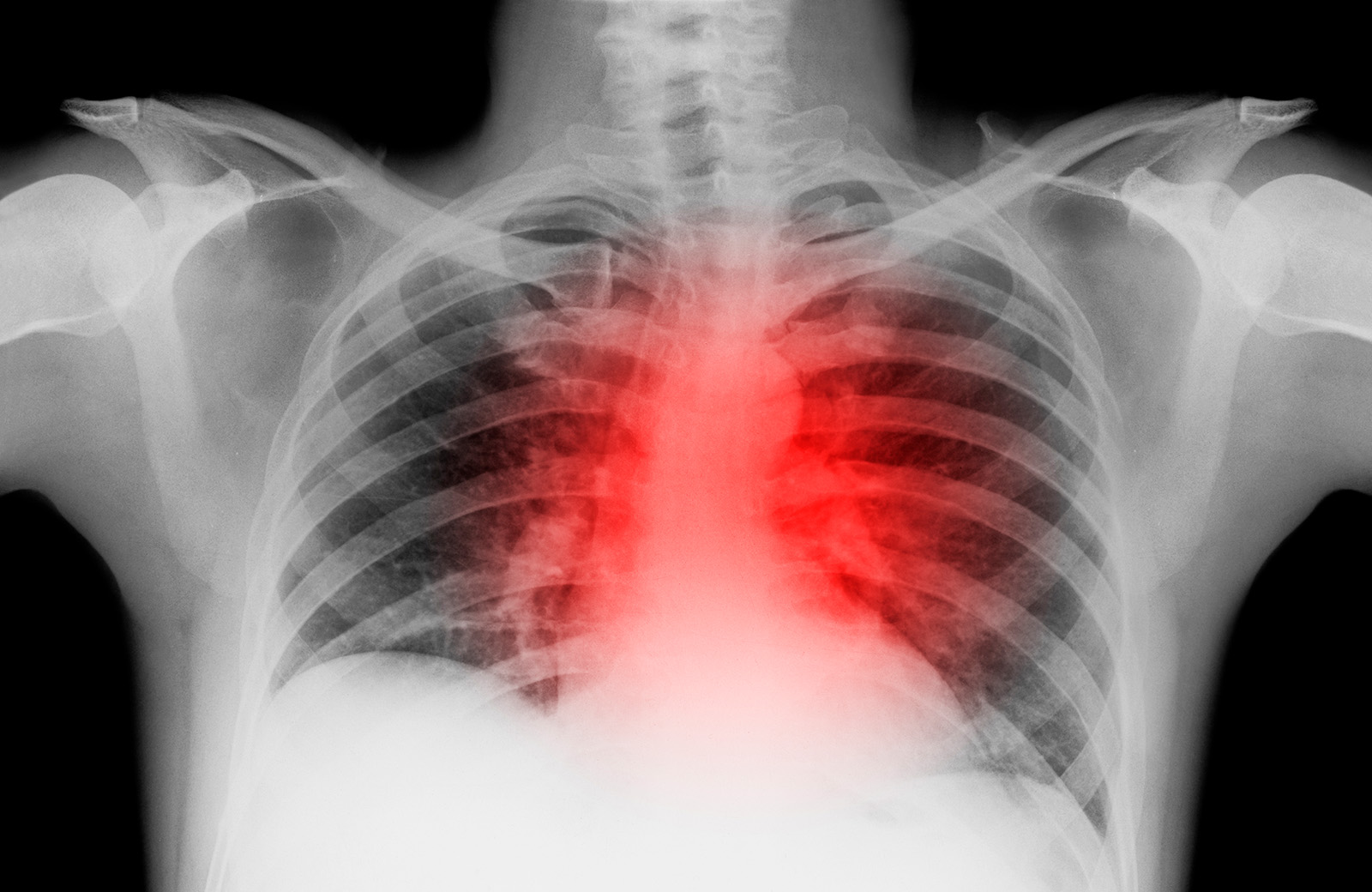
False Beliefs About Heart Attack Treatment and Prevention Persist as Heart Disease Remains Leading Cause of Death
Heart disease is the leading cause of death in the U.S. and ongoing research continues to examine new factors like COVID-19 that influence cardiovascular risk. However, misinformation about heart attack treatment and prevention persists. One misconception that has re-emerged is that coughing during a heart attack, sometimes called ‘cough CPR,’ can help maintain blood flow to the heart. Health experts have debunked this, explaining that CPR is used for cardiac arrest, not heart attacks, and that by the time CPR is necessary, a person is typically unable to cough. Additionally, coughing cannot restart a heart that has stopped beating. The confusion likely stems from the use of coughing as a temporary measure during certain arrhythmias in monitored medical settings, leading to the misconception that it can improve heart function during a heart attack and potentially delaying care.
Outdated guidelines may also contribute to misconceptions about heart attack prevention. Daily aspirin use was once widely recommended for healthy adults to reduce heart attack and stroke risk, however, guidelines from the American College of Cardiology and the American Heart Association (AHA) issued in 2019 only recommend aspirin as an option among adults ages 40-70 who have elevated risk of cardiovascular disease. The guidelines also advise against routine aspirin use for healthy adults over 70 due to the risk of gastrointestinal bleeding. Despite this, a survey by the Annenberg Public Policy Center found that this misconception persists, particularly among older adults. The survey found that 18% of people without a personal or family history of heart attack or stroke reported regularly taking low-dose aspirin, and nearly 43% believed its benefits outweigh the risks. Those ages 60 and over were especially likely to take aspirin daily for prevention and to believe in its benefits, despite updated guidance.
AI & Emerging Technology
Gaps in Research Standards for AI Chatbots in Healthcare
As artificial intelligence (AI) continues to shape healthcare, large language models (LLMs) are increasingly consulted for medical advice. However, concerns persist regarding their accuracy, transparency, and safety. A systematic review of 137 studies evaluated the reporting quality of research assessing LLMs’ ability to offer health guidance. Findings revealed that nearly all studies examined closed-source models without disclosing sufficient details about the LLM version or parameters. Most studies relied on subjective measures to assess chatbot performance, and fewer than a third considered ethical, regulatory, or patient safety implications. The variability in study design and reporting highlights a gap in standardized assessment frameworks which may be useful for conducting reliable evaluations of LLMs used in healthcare.
Support for the Health Information and Trust initiative is provided by the Robert Wood Johnson Foundation (RWJF). The views expressed do not necessarily reflect the views of RWJF and KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities. The Public Good Projects (PGP) provides media monitoring data KFF uses in producing the Monitor.