Women’s Sexual and Reproductive Health Services: Key Findings from the 2020 KFF Women’s Health Survey
Issue Brief
Key Takeaways
Use of Contraceptives
- Six in ten (60%) women aged 18 to 49 years say it is very important to avoid becoming pregnant in the next month; one in four women (25%) say avoiding pregnancy is not a priority. One in seven (14%) sexually active women report they are not using any form of contraception and the leading reason is concern and dislike of side effects.
- More than four in ten (44%) women have been worried they were pregnant when they did not want to be and the main reason was because they did not use birth control.
- Oral contraceptives and condoms are the leading forms of reversible contraception women use, and almost a quarter say they use an intrauterine device (IUD).
- Most women (72%) use more than one type of contraception in their lifetime and on average, women use 3.4 different contraceptive methods throughout their lifetime.
- Nearly one in five women (18%) use contraception solely for a reason not related to preventing pregnancy such as managing a medical condition or preventing STIs.
Contraceptive Coverage
- One in five women (18%) are not using their preferred method of contraception and a quarter (25%) say it is because they can’t afford it.
- Almost two-thirds of privately insured women have full contraceptive coverage through their plans where all FDA-approved contraceptive methods and contraceptive counseling and education are covered without cost-sharing, but one in five women (21%) with private insurance are still paying some out-of-pocket costs for their contraceptive care.
- Nearly one-third (31%) of oral contraceptive users say they have missed taking their birth control because they were not able to get their next supply in time.
Access to Quality Sexual and Reproductive Health Care
- Publicly funded clinics provide contraceptive care for one in five low-income and uninsured women (21%). The majority of women rely on office-based providers for their birth control.
- Four in ten women (44%) rate their provider’s contraceptive counseling as excellent, but the share rating counseling as excellent is lower among Black (36%) and Hispanic (38%) women, as well as low-income (35%) and uninsured (28%) women.
- The majority of reproductive-aged women (65%) are comfortable with pharmacists prescribing birth control and support making birth control available over the counter without a prescription (70%).
- Most reproductive-aged women have discussed contraception with their providers (68%), but a much smaller shared were asked about sexually transmitted infections (26%-28%) and domestic violence (38%). Only about 1 in 10 (11%) of women of reproductive age say they have discussed HIV pre-exposure prophylaxis (PrEP) with their provider.
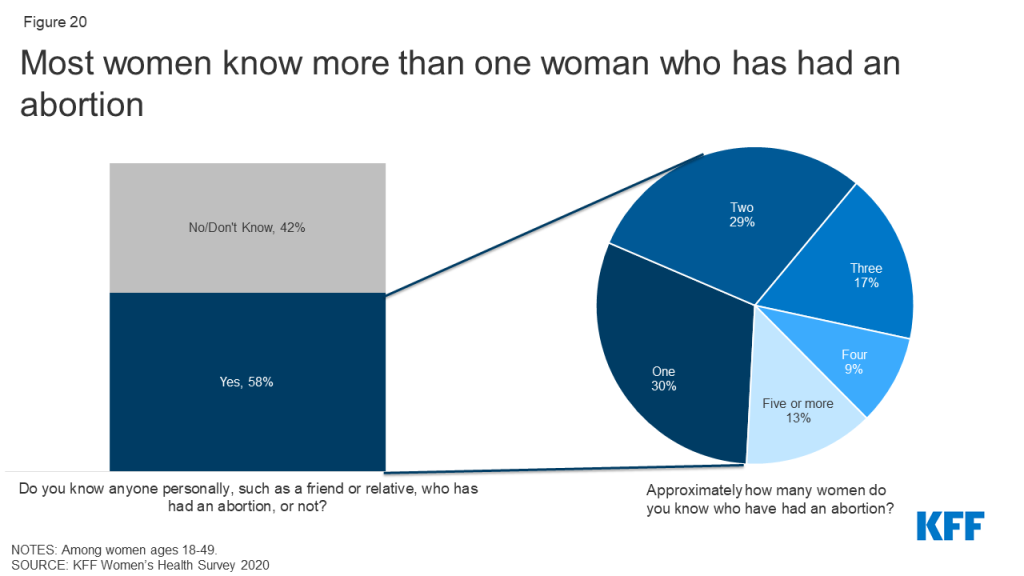
- Most reproductive-aged women (58%) know someone who has had an abortion with 68% of those women knowing more than one person and just over half of women have heard of a medication abortion (57%).
Introduction
Sexual and reproductive health is an integral part of women’s overall health. Access to these services is shaped by a broad range of factors including coverage and affordability, national and state policies, availability of care, health provider characteristics, as well as individual preferences and experiences. For many women, the Affordable Care Act (ACA) improved access to sexual and reproductive health care by expanding pathways to Medicaid eligibility and making private insurance more affordable. The ACA also required private health insurance plans to cover many recommended preventive services without any patient cost-sharing, such as sexually transmitted infection counseling and screening and all 18 FDA-approved contraceptive methods. While the ACA has expanded sexual and reproductive health care, state and federal policy actions in recent years have resulted in more limited access to comprehensive sexual and reproductive health care, including abortion referrals and services, particularly for women who depend on publicly supported health care providers and clinics.
Access in the past year has also been undoubtedly affected by the COVID-19 pandemic, which has forced providers to find ways to make contraceptive and STI services available via telehealth or through minimal contact, like no-test medication abortions. There is increasing interest in expanding efforts to allow pharmacists to prescribe birth control, gain FDA approval for over-the-counter oral contraception without a prescription, and expanding access to contraception through smartphone apps or online platforms that no longer require a visit to a brick-and-mortar clinic or doctor’s office.
While the system is undergoing constant change, the perspectives and experiences of women in obtaining sexual and reproductive health care can help to shape the next generation of policies and programs. This brief provides a window into some of those voices and perspectives by presenting selected findings from the 2020 KFF Women’s Health Survey, a nationally representative survey of women conducted in November/December of 2020 (Methodology). The survey covered a wide range of topics related to women’s coverage, use, access, and experiences with the health care system. This brief presents survey findings on coverage and use of reproductive and sexual health services among different subgroups of 2,695 women ages 18 to 49.
Use of Contraceptives
WHILE MOST REPRODUCTIVE AGE WOMEN SAY IT IS IMPORTANT TO THEM TO PREVENT PREGNANCY, ONE IN FOUR WOMEN SAY AVOIDING PREGNANCY IS NOT A PRIORITY.
Among women ages 18-49 who are not currently trying to get pregnant, the majority say it is very important (60%) or somewhat important (10%) for them to avoid becoming pregnant in the next month, but a quarter of women (25%) say it is not very important or not important at all (Figure 1). More than half (57%) of women who are not using contraception say that it is very important or somewhat important for them to avoid pregnancy compared to 81% of women using contraception. These data speak to the fact that even though women are not necessarily trying to get pregnant, they may be open to having a pregnancy and may not want to use contraception.
WOMEN ARE NEARLY TWICE AS LIKELY TO HAVE BEEN CONCERNED ABOUT AN UNWANTED PREGNANCY COMPARED TO MEN.
Over four in ten (44%) women have thought they were pregnant when they did not want to be, compared to one in four (27%) men who said this with regard to a partner (Figure 2). Nearly half (47%) of women and over half of men (57%) said it was because they did not use birth control. About a quarter of women (23%) and men (27%) said they or their partner had missed a pill or they had used their birth control incorrectly, 19% of women and 16% of men said their birth control failed like a condom breaking, and 18% of women and 22% of men weren’t sure the contraceptive method they were using worked.
A MINORITY OF WOMEN AND MEN USED CONDOMS THE LAST TIME THEY HAD SEX.
Six in ten sexually active women report using a method of contraception the last time they had sex compared to four in ten men, regardless of current partner status (Figure 3). Condom use at last sex was lower. Overall, 16% of women say their partner used a condom the last time they had sex, and 26% of men report using a condom. This differed significantly by whether someone was married or living with their partner compared to not. Condoms are not only used as contraceptives but are effective in reducing the risk of transmission of sexually transmitted infections. Men who are married or living with a partner are 2.5 times more likely to use a condom than men who are widowed, divorced, separated, or never married (40% vs. 16%). Thirteen percent of women who are married or living with a partner say their partner used a condom the last time they had sex compared to 23% of women who are widowed, divorced, separated, or never married. When asked if they had discussed birth control or condom use with their most recent sexual partner, the majority of men and women, regardless of partner status, said they had discussed with their partner.
ONE IN SEVEN SEXUALLY ACTIVE WOMEN DO NOT USE CONTRACEPTION. CONTRACEPTIVE NON-USE IS HIGHER AMONG ASIAN WOMEN AND WOMEN WHO ARE UNINSURED OR LOW-INCOME.
Over six in ten sexually active women of reproductive age report using at least one method of contraception in the past 12 months, while one in seven (14%) report that they did not use contraception and are not trying to conceive (Figure 4). One in four (25%) uninsured women report not using contraception compared to 13% of women with Medicaid and private insurance. Similarly, almost a quarter of sexually active Asian women report not using contraception compared to 13% of Black and White women and 15% of Hispanic women, while a lower share of Asian women report they or their partner are unable to conceive (3% vs. 11% of Hispanic women, 14% of Black women, and 19% of White women). Low-income women are also more likely to report not using contraception compared to higher-income women (18% vs. 13%) (Figure 5).
.
When asked about the reason for not using birth control, the number one reason was being worried about or disliking the side effects of birth control (29%), followed by not minding if they got pregnant (23%) and not wanting to use birth control (23%) (Figure 6). Over 1 in 5 women cited another reason that was not included in the survey.
CONDOMS, ORAL CONTRACEPTION, AND IUDS ARE THE MOST COMMONLY USED FORMS OF CONTRACEPTION.
Reproductive-aged women were most likely to have used male condoms in the past 12 months (39%), followed by oral contraceptives (37%), and IUDs (23%) (Table 1). Compared to all women of reproductive age, younger women ages 18-35 were more likely to have used oral contraceptives (50% vs. 37%), the contraceptive patch (4% vs. 2%), a contraceptive implant (11% vs. 7%), male condoms (47% vs. 39%), and emergency contraception (15% vs. 9%). Women ages 26-35 were more likely to use fertility awareness-based methods (11%) compared to all women of reproductive age (8%). Women ages 36-49 were most likely to have used an IUD in the past 12 months (28%) compared to all women of reproductive age (23%).
MOST WOMEN USE MORE THAN ONE CONTRACEPTIVE METHOD IN THEIR LIFETIME.
Eighty-seven percent of women report using contraception at some point in their lifetime and on average, women report using 3.4 methods of contraception throughout their lifetime. Seven in ten women (70%) ages 18-64 say they have used oral contraceptives, including a larger share of women ages 36-64. Male condoms were the second most frequently used contraceptive among women ages 18-64 (66%). Younger women ages 18-35 have higher shares that have used implants and emergency contraception compared to women overall (Table 2). Nearly three-fourths of women (72%) have used more than one type of contraception in their lifetime, four in ten women have used more than two types of contraception in their lifetime (42%), and one in five women have used more than three types of contraception in their lifetime (22%). Contraceptive switching is common and it is important that women have access to the full range of contraceptive methods without cost-sharing, so they can find the contraceptive method that works best for them if they want to use contraception. Also, women’s contraceptive needs can change over their reproductive lifespan, what works when they are in their twenties may not be what is best for them in their thirties or forties. Shared-decision making with a provider can allow a patient to communicate their values and preferences for contraception and the provider can share their medical knowledge to help the patient find a contraceptive method that is most consistent with their preferences.
NEARLY ONE IN FIVE WOMEN USE CONTRACEPTION FOR A REASON NOT RELATED TO PREVENTING PREGNANCY.
While many women have used more than one contraceptive in their lifetime, they also use contraception for more than just preventing pregnancy. Over six in 10 women (61%) say they use contraception only to prevent pregnancy (Figure 7). Over one in five (22%) women use contraception to prevent pregnancy and some other reason. Nearly one in five women (18%) use contraception solely for a reason not related to preventing pregnancy such as managing a medical condition or preventing STIs.
ONE IN FOUR UNINSURED AND LOW-INCOME WOMEN ARE NOT USING THEIR PREFERRED CONTRACEPTIVE METHOD.
While many women try and use multiple contraceptive methods throughout their lives for various reasons, nearly one in five women (18%) say they are not currently using their preferred method of birth control (Figure 8). This share is higher among uninsured and low-income women who may not have affordable access to the full range of contraceptive methods or be aware of public programs that provide those services. The primary reason women say they are not using their preferred method of contraception is because they cannot afford it (Figure 9). The goal of publicly supported programs like Title X and Medicaid is to provide access to family planning services to individuals who need family planning services but may not be able to afford services because of lack of insurance or low income. Most Title X clinics provide the full range of contraceptive methods to their uninsured and low-income clients. The fact that such a sizable share of women still report affordability barriers to care may speak to the role of public programs and the need for outreach to expand awareness of and access to sexual and reproductive health care services to low-income and uninsured women.
.
Among women who are not using their preferred method, one in five women (20%) say it is because their provider recommended a different method. There is increasing consensus about the importance of high-quality, client-centered contraceptive counseling to ensure that provider care is respectful of, and responsive to, individual patient preferences, needs, and values and importantly, that the patient guides all clinical decisions. Ensuring that patients have autonomy in their contraceptive decision-making is of high value and leads to greater satisfaction with their care and continued use of their method of choice.
Contraceptive Coverage
ONE IN FIVE WOMEN STILL REPORTS PAYING OUT-OF-POCKET FOR CONTRACEPTIVE CARE NEARLY 10 YEARS AFTER THE ACA WENT INTO EFFECT.
The ACA requires that most private plans cover contraceptive services which include patient education and counseling for contraceptive services and all of the 18 FDA- approved methods of contraception without cost-sharing. This provision has drastically reduced cost-sharing for contraception among women with employer or individual insurance plans. The majority of privately insured women report that their insurance covers the full cost of their contraceptive care (64%), but one in five (21%) women say their insurance only covered part of the cost and they paid the rest (Figure 10). There are a number of reasons that women could be responsible for some or all of those payments. For example, a woman could be using a brand-name contraceptive that is not in her plan’s formulary or she is unaware of or not offered a generic alternative. Some women paying out-of-pocket could also be receiving care out-of-network or still be enrolled in a grandfathered health insurance plan (which is exempt from the requirement). Some 13% of covered workers are enrolled in a grandfathered plan in 2019. An unknown number of women are also either employed by or dependents of a worker employed by an organization that has a religious objection to contraception. Those employers are not obligated to provide no-cost contraceptive coverage to their employees. Only 5% of women said they have had problems getting their insurance to pay for a prescribed birth control, such as an IUD, implant, injection, patch, pill, or ring.
In recent years, there has been a move to expand the supply of contraceptives dispensed to women since some women miss their pill (and are at risk of an unplanned or unwanted pregnancy) because they have run out of their supply. The majority of women ages 18-49 (59%) who used oral contraceptives in the past 12 months, received 3-5 months’ supply (Figure 11). However, twice as many low-income women compared to women with incomes ≥ 200% FPL only received 1–2-month supply (43% vs. 20%). Women with Medicaid also received a 1–2 months' supply at twice the rate of women with private insurance (42% vs. 22%). A much larger share of uninsured women (15%) reported receiving 6-11 months of supply compared to women with Medicaid and private insurance (1%). Laws have been passed in at least 17 states and DC that require coverage for 12 months of oral contraceptives to allow women continuous contraceptive coverage for at least a year. However, these laws typically only apply to fully insured plans. Many Medicaid programs can and do limit supply of hormonal contraception to 1-3 month periods; self-funded employer plans are also permitted to do this. Shorter supplies can result in women missing their pills due to delays in receiving their next supply.
Nearly one-third (31%) of hormonal contraceptive users say they have missed taking their birth control because they were not able to get their next supply of pills. This share is higher among younger women ages 18-25 and 26-35 compared to women ages 36-49 (38% and 34% vs. 16%) and among low-income women <200% FPL compared to women with incomes ≥200% FPL (36% vs. 26%) (Figure 12).
Access to Quality Sexual and Reproductive Health Care
THE MAJORITY OF WOMEN GET THEIR CONTRACEPTIVE CARE FROM OFFICE-BASED PHYSICIANS FOLLOWED BY CLINICS.
Three in four reproductive-age women who use contraception report receiving it from a doctor’s office (Figure 13). Many women, particularly about one-fifth of those who are Hispanic (20%), low-income (21%), covered by Medicaid (18%), or uninsured (21%), also use clinics such as federally qualified health centers (FQHC) or freestanding family planning clinics such as Planned Parenthood. Notably, about one in five women who are uninsured said they obtained their most recent contraception at another site, such as a pharmacy or drugstore. And, while there has been growing interest in telehealth, just 5% of women reported that they obtained contraception via a phone or video visit, website, or app.
LESS THAN HALF OF WOMEN REPORT RECEIVING THE HIGHEST QUALITY PERSON-CENTERED COUNSELING.
Women’s interactions with providers play an important role in the quality of their contraceptive care. While there has been a lot of emphasis on access to the most effective methods, there is also growing interest in ensuring that patient-provider relationships are patient-centered and support patient decision making. Approximately four in ten women (44%) rate their most recent contraceptive care provider as “excellent” on all four items of person-centered contraceptive counseling (Figure 14): respecting them as a person, letting them say what mattered to them about their birth control method, taking their preferences about their birth control seriously, and giving them enough information to make the best decision about their birth control. It is particularly concerning that Black, Hispanic, low-income, and uninsured women are less likely to receive this level of high-quality client-centered care. There is a long history of poor reproductive health care for these same groups. It is important to note that there were no significant differences by the type of setting in which the counseling was received, signaling that these groups may be receiving less client-centered care because of their race/ethnicity, income, or insurance regardless of the setting.
Currently, prescription contraceptives require a visit with a clinician in most states. In recent years though, there have been efforts to expand the availability of contraceptives through different avenues, including allowing pharmacists to prescribe and provide some hormonal methods and, applications to the FDA to make oral contraceptive pills (OCPs) available over-the-counter (OTC) without a prescription. Our survey finds that most women are in favor of these changes (Table 3). These approaches appear to be attractive to the majority of reproductive-age women: two-thirds (65%) say they are comfortable with pharmacists prescribing contraceptives and 70% support making pills available OTC if the FDA says it is safe and effective. There are differences in acceptability between different subgroups of women with higher levels of acceptability found among White women, women with a college degree, women living in urban/suburban areas, and Democratic women.
ONE-THIRD OF 18-25 YEAR OLD WOMEN HAVE NEVER SEEN A DOCTOR OR NURSE FOR A GYNECOLOGICAL EXAM. PRIVATELY INSURED WOMEN WERE THE MOST LIKELY TO HAVE A HAD A GYN VISIT IN THE PAST 12 MONTHS AND UNINSURED THE LEAST LIKELY.
Nearly three in four reproductive age women report that they have had a gynecological exam in the past three years (Figure 15). However, that is the case for only half of uninsured women (49%). More than one in ten uninsured women (14%) say that they have never had a gynecological exam, higher than the share of privately insured women (8%). Receipt of gynecological exam increases with age. While 30% of women ages 18-25 say they have never had an exam, that share drops to 4% among women ages 26-35. A gynecological exam usually includes cervical and breast cancer screening, education, and counseling that can prevent future negative health outcomes.
Screening Tests
ASIAN, UNINSURED AND RURAL WOMEN WERE THE LEAST LIKELY TO REPORT HAVING A PAP TEST WITHIN THE PAST TWO YEARS.
A number of federal bodies and professional organizations recommend that women receive sexual health screening tests. These tests are covered without any out-of-pocket charges for women with private insurance and under Medicaid expansion per the ACA’s preventive services requirement. The USPSTF recommends that women receive a Pap smear at least every three years beginning at age 21 depending on their personal risk factors for developing cervical cancer. More than two-thirds (68%) of women ages 21-49 say they have received one in the past two years. However, that is the case for only half of uninsured women (50%) (Figure 16). Pap testing rates are higher among Black women (79%) and lower among Asian women (58%), compared to women who are White (68%). Women who live in rural areas are also less likely than those living in urban areas to have had a Pap test in the prior two years. Many rural communities suffer from a dearth of reproductive health care providers, which may contribute to the lower rates of screening.
DESPITE RECOMMENDATIONS FOR ROUTINE STI AND HIV TESTING, FEW WOMEN HAD HAD A RECENT TEST.
One in four women (26%) report they had an HIV test in the past 2 years and one in three women (33%) who had a recent provider visit say they have had a test for an STI other than HIV in the past two years (Table 4). Knowing one’s status is important for receiving early treatment and preventing transmission to sexual partners. STI and HIV tests are covered without cost-sharing in private plans under the ACA’s preventive services coverage requirements and are typically covered by Medicaid programs. Screening rates are higher among women who are younger and low-income, as well as Black and Hispanic women compared to White women.
However, the actual screening rate is likely lower than the share of women who report being tested, as some assume (erroneously) that STI and HIV tests are routine components of a clinical visit. About one-quarter of women who said they were tested for HIV (26%) recently were under the impression that it is routine, which is not the case (Figure 17). This is also true for about a quarter of women who said they had been tested for other STIs (23%). This may cause women to believe they do not have HIV or another STI when in fact they have not actually been tested.

Sexual and Reproductive Health Counseling and Education
An important part of the gynecological exam and well-woman visit is counseling and education around sexual and reproductive health care, including discussions around contraception, sexual history or relationships, and sexually transmitted infections (STIs). The ACA also covers contraceptive counseling, as well as HIV and STI counseling without cost-sharing.
WOMEN ARE MUCH MORE LIKELY TO HAVE DISCUSSIONS WITH PROVIDERS ABOUT CONTRACEPTION THAN ABOUT STIs, HIV OR PrEP.
Among these sexual and reproductive health topics, the largest share of women ages 18-49 say they have been asked about or discussed contraception with their provider in the past two years (68%) (Table 5). Black women were significantly less likely to have discussed contraception with their provider compared to White women (60% vs. 70%). The majority of women (63%) also say they have discussed their sexual history with a provider.
Less than one-third of women of reproductive age say they were asked by a provider about HIV or another STI (26% and 28%, respectively). Women with Medicaid were more likely to have a discussion with their provider about HIV (31%) compared to women with private insurance (26%). A larger share of Black (32%) and Hispanic (31%) women were also asked about HIV compared to White women (22%). STI rates continue to rise, with younger women and Black and Hispanic women being disproportionately affected. STI counseling for all people of reproductive age is recommended to help individuals reduce their risk for STI transmission.
Only about 1 in 10 (11%) women of reproductive age say they have discussed HIV pre-exposure prophylaxis (PrEP) with their provider and this was higher among Asian (18%) and Hispanic (15%) women compared to White women (8%). Women with Medicaid (14%) were more likely to discuss PrEP compared to women with private insurance (10%) and low-income women (15%) compared to women with incomes ≥ 200% FPL (10%).
Across all the sexual and reproductive health topics, younger women ages 18-35 compared to women ages 36-49 and women living in urban areas compared to rural areas were more likely to be asked about these topics or discuss them with their doctor or health care provider. Roughly one-third of women ages 40-64 (32%) say a provider has discussed menopause with them recently.
FEW WOMEN ARE SCREENED FOR INTIMATE PARTNER VIOLENCE, DESPITE THE PRESENCE OF RECOMMENDATIONS FROM THE US PREVENTIVE SERVICES TASKFORCE AND THE WOMEN’S PREVENTIVE SERVICES INITIATIVE FOR SCREENING.
Another important topic that the US Preventive Services Task Force recommends providers to screen women of reproductive age for is intimate partner violence (IPV). However, only 38% of women ages 18-49 say a provider has asked them about domestic violence or dating violence in the past two years (Figure 18). This is higher among women ages 26-35 (44%) compared to women ages 36-49 (36%) and women with Medicaid (46%) compared to women with private insurance (38%). However, only 1 in 4 (26%) uninsured women were asked about it. Smaller shares of Asian women (25%) and Black women (33%) report discussing IPV compared to 40% of White women. There were no statistical differences by income and location.
Abortion
A HIGHER SHARE OF WOMEN THAN MEN SAY THEY PERSONALLY KNOW SOMEONE WHO HAS HAD AN ABORTION.
Abortion services are a significant component of sexual and reproductive health care, given that one in four women have had an abortion, making it a relatively common health care service. Nearly six in ten women (58%) and four in ten men (39%) say that they know somebody who has had an abortion (Figure 19). Of that group, most (68%) know more than one woman who has had an abortion (Figure 20). Rates are higher among those who are older, higher income, higher educational attainment (Table 6). Most know one or two women who have had an abortion and on average, women know 2.8 women and men know 2.5 women who have had an abortion.
KNOWLEDGE OF MEDICATION ABORTION IS STILL RELATIVELY LOW. ROUGHLY HALF OF WOMEN AND MEN HAVE HEARD OF MEDICATION ABORTION EVEN THOUGH IT WAS APPROVED BY THE FDA 20 YEARS AGO.
Medication abortion is a pregnancy termination protocol that can be used up to the first 10 weeks of pregnancy that involves taking two different drugs, Mifepristone and Misoprostol. It has been available in the United States for more than 20 years and now accounts for approximately half of all early abortions. However, there are many restrictions on its availability, including an FDA REMS requirement, bans on telemedicine, and requirements for in-person counseling visits and other tests that are not medically recommended for safety. The COVID-19 pandemic has brought many of these restrictions to the forefront as providers have tried to implement no-test and telehealth medication abortion protocols that allow women to pick up medication abortion pills or have them mailed directly to their home with phone or video follow-up without requiring any testing or pre-abortion ultrasounds.
Over half of reproductive-aged women (57%) and almost half of men (48%) say that they have heard of medication abortion (Figure 21). Rates are lower though among Hispanic women, those with lower incomes, and those living in rural areas.
Conclusion
Sexual and reproductive health is multi-faceted and an integral part of a person’s overall health. In recent years, state and federal policies have had a major impact on access to sexual and reproductive health care across the nation, in some cases limiting access and in other broadening availability of care. The Affordable Care Act (ACA) enabled more women to obtain sexual and reproductive health care by expanding access to Medicaid and private insurance coverage and strengthening the scope of that coverage. While it made several preventive sexual and reproductive health services and counseling available without cost-sharing, many women are still saying that affordability is a barrier to contraceptive care, are not using the contraceptive of their choice, and are not getting the recommended levels of preventive sexual and reproductive health care services to which they are entitled under federal law.
Federal support for the family planning safety-net, the types of clinics that may participate in federal programs like Medicaid and Title X as well as state choices regarding Medicaid expansion all have an effect on the ability of low-income and uninsured women to gain access to reproductive care. While the COVID-19 pandemic has challenged providers to find new ways to make contraceptives, STI services, and in some cases abortion care, available via telehealth, it has brought the long-standing structural inequities in the health system into stark focus. Understanding how women use reproductive and sexual health care and the challenges they face could help leaders at the federal, state, and community level make such care more accessible and equitable.
Methodology
The 2020 KFF Women’s Health Survey was designed and analyzed by researchers at the Kaiser Family Foundation (KFF) of a representative sample of 4,805 adults, ages 18-64 years old (3,661 women and 1,144 men). The survey was conducted online and telephone using AmeriSpeak®, the probability-based panel of NORC at the University of Chicago. U.S. households are recruited for participation using address-based sampling methodology and initial invitations for participation are sent by mail, telephone, and in-person interviews. Interviews were conducted in English and Spanish online (4,636) and via the telephone (169). Our previous Women's Health Surveys were conducted exclusively by telephone, so trend data are not included in our 2020 survey. Interviews for this survey were conducted between November 19 and December 17, 2020, among adults living in the United States. KFF paid for all costs associated with the survey.
The sample for this study was stratified by age, race/ethnicity, education, and gender as well as disproportionate stratification aimed at reaching uninsured women, women who identify as LGBT, Asian women, and women 18-49 years old. The sampling also took into consideration differential survey completion rates by demographic groups so that the set of panel members with a completed interview for a study is a representative sample of the target population. This survey includes people who self-identified as 'female' or 'male’ regardless of their sex at birth. While our goal was to be as inclusive as possible, we were not able to obtain a large enough sample to support a separate questionnaire that addresses the unique health concerns and experiences of non-binary or gender-fluid people to include them in this survey. We recognize that additional study is needed to better understand the health and access issues faced by non-binary people.
A series of data quality checks were run and cases determined to be poor-quality, as defined by surveys with a length of interview of less than 33% of the mean length of interview and with high levels of question refusal (>50%) were removed from the final data (n=96). Weighting involved multiple stages. First, the sample was weighted to match estimates for the national population from the 2020 Current Population Survey on age, gender, census division, race/ethnicity, and education. The second round of weights adjusted for the study’s sampling design. All statistical tests of significance account for the effect of weighting.
The margin of sampling error including the design effect for the full sample of women is plus or minus 2 percentage points. Numbers of respondents and margins of sampling error for key subgroups are shown in the table below. For results based on other subgroups, the margin of sampling error may be higher. Sample sizes and margins of sampling error for other subgroups are available by request. Note that sampling error is only one of many potential sources of error in this or any other public opinion poll.
| Group | N (unweighted) | M.O.S.E |
| Men Ages 18-64 | 1,144 | +/- 4 percentage points |
| Women Ages 18-64 | 3,661 | +/- 2 percentage points |
| Women Ages 18-49 | 2,695 | +/- 2 percentage points |
| White Women Ages 18-64 | 1,813 | +/- 3 percentage points |
| Black Women Ages 18-64 | 603 | +/- 5 percentage points |
| Hispanic Women Ages 18-64 | 801 | +/- 5 percentage points |
| Asian Women Ages 18-64 | 246 | +/- 8 percentage points |
| LGB Women Ages 18-64 | 392 | +/- 7 percentage points |
| Heterosexual Women Ages 18-64 | 3,239 | +/- 2 percentage points |
| Women < 200% FPL | 1,471 | +/- 3 percentage points |
| Women ≥200% FPL | 1,943 | +/- 3 percentage points |

























