States Focus on Quality and Outcomes Amid Waiver Changes: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2018 and 2019
Benefits and Copayments
| Key Section Findings |
| A total of 19 states expanded or enhanced covered benefits in FY 2018 and 24 states plan to add or enhance benefits in FY 2019. The most common benefit enhancements reported were for mental health/substance use disorder (SUD) services (including waiver of the IMD exclusion for SUD treatment). A handful of states reported expansions related to dental services, telemonitoring/telehealth, physical or occupational therapies, and screening and home visiting services for pregnant women. Eight states reported new or increased copayments and nine states reported policies to eliminate or reduce a copay requirement for FY 2018 or FY 2019.
What to watch:
Tables 14 and 15 provide a complete listing of Medicaid benefit changes for FY 2018 and FY 2019. Table 16 provides a list of states that reported copayment actions for FY 2018 and FY 2019. |
Benefit Changes
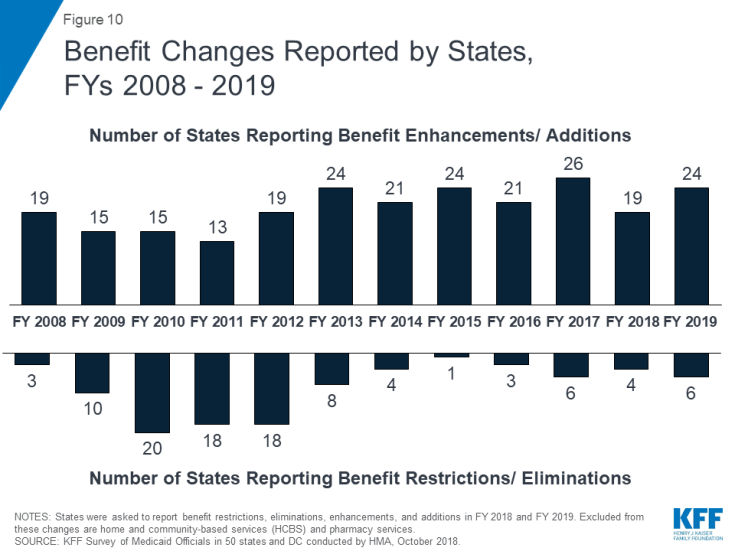
The number of states reporting new benefits and benefit enhancements continues to significantly outpace the number of states reporting benefit cuts and restrictions. Nineteen states reported new or enhanced benefits in FY 2018, and 24 states are adding or enhancing benefits in FY 2019. Few states reported benefit cuts or restrictions – four in FY 2018 and six in FY 2019 (Figure 10 and Table 14).
The most common benefit enhancements reported were for mental health and substance use disorder (SUD) services. Exhibit 17 also highlights states implementing other select benefit enhancements for dental, telemonitoring/telehealth, physical and occupational therapies, screening and home visiting services for pregnant women and children, and alternative therapies.
| Exhibit 17: Select Categories of Benefit Enhancements or Additions | ||||
| Benefit | FY 2018 | FY 2019 | ||
| Mental Health/Substance Use Disorder Services | 9 States | IN, MD, MA, NE, OH, RI, UT, VA, WV | 18 States | AK, DC, HI, IL, IN, KS, KY, MD, NC, NH, NJ, NM, RI, SD, TN, TX, WI, WV |
| Dental Services | 3 States | AZ, CA, UT | 2 States | IL, MD |
| Telemonitoring/ Telehealth Services | 4 States | IN, MD, NY, SC | 1 State | TX |
| Therapy Services (PT, OT) | 3 States | AZ, CO, WI | 1 State | NY |
| Screening and Home Visiting Services for Pregnant Women and/or Children | 3 States | CO, TX, VT | 2 States | IL, NM |
| Alternative Therapies (e.g., Chiropractic and Acupuncture) | 2 States | IN, OH | 1 State | MO |
Similar to our findings in last year’s budget survey, a number of states continue to report expanded mental health and/or SUD services. Many of these expansions are state initiatives to use Medicaid funds for services provided in institutions for mental disease (IMDs) under approved or pending Section 1115 waivers. These expansions include states responding to July 2015 CMS guidance1 stating that states can request federal funding for SUD services delivered to nonelderly adults in IMDs through Section 1115 demonstration waivers, as well as revised November 2017 guidance2 that continues to allow states to seek Section 1115 waivers to pay for SUD services provided in IMDs.
While IMD waivers approved under the previous administration were contingent on coverage of services across the care continuum, recently approved IMD waivers generally do not address coverage of community-based SUD services. Also, the SUPPORT Act,3 which was expected to be signed into law as this report was being finalized, would create a state plan option from October 1, 2019 to September 30, 2023 to cover IMD services for up to 30 days in a year for non-elderly adults with an SUD. The SUPPORT Act also would codify the 2016 Medicaid Managed Care Final Rule provision allowing “in lieu of” IMD coverage for up to 15 days in a month.
Other non-IMD mental health and SUD service expansions that states reported include expanding access to screening and intervention services and supporting recovery with new services such as peer supports. States also continue to increase access to naloxone and medication assisted treatment (MAT) services. See the “Opioid Harm Reduction Strategies” section of this report for details on these initiatives.
Other noteworthy benefit expansions include:
- Neonatal Abstinence Syndrome (NAS) Treatment Services: In FY 2018, West Virginia became the first state to receive CMS SPA approval to finance NAS services using a bundled payment for providers outside the hospital inpatient setting. The incidence of NAS is directly related to the nation’s opioid epidemic and involves infant withdrawal symptoms due to in utero exposure to certain substances.4 West Virginia’s NAS benefit package includes pharmacological and non-pharmacological interventions to holistically treat the withdrawal symptoms, which can include tremors, seizures, and vomiting. CMS highlighted West Virginia’s approach in a June Informational Bulletin5 as a model that pays an all-inclusive rate for neonatal abstinence treatment professional services and other ancillary services in a pediatric residential center specializing in NAS treatment. In addition, the SUPPORT Act6 would create a new State Plan option, effective upon enactment, to provide inpatient or outpatient residential pediatric recovery centers services for infants under age 1 with NAS and their families.
- Community Health Workers: Both Indiana and South Dakota reported plans to cover services provided by Community Health Workers (CHWs). Indiana began covering CHW services on July 1, 2018, adopting the American Public Health Association’s definition of a CHW. For services to be covered, the CHW must be certified by a recognized organization, employed by a Medicaid-enrolled provider, and have delivered services under their supervision. The CHW is part of the health care team and provides patient education, facilitates communication when cultural factors may be a barrier to care, promotes healthy behaviors, and provides direct preventive services or services intended to slow the progression of chronic disease.7
- Diabetes Prevention: Two states reported plans to cover Diabetes Prevention Program services in FY 2019. Diabetes Prevention Programs aim to delay or prevent the onset of type 2 diabetes with targeted health behavior interventions. California will start covering these services for beneficiaries diagnosed with prediabetes in FY 2019. New Jersey is also adding coverage of Diabetes Prevention Program services in FY 2019, as well as diabetes self-management education.
- Enhanced Screening, Identification, and Other Support Services for New Mothers: In FY 2018, Colorado and Texas started covering depression screenings for mothers in the first 12 months of a child’s life. In Texas, the screening is provided through the child’s benefit package as part of a well child visit. In FY 2019, New Mexico will pilot a home visiting program as part of its pending Section 1115 waiver that will focus on prenatal care, postpartum care, and early childhood development. Home visits will include patient education, skill building, screenings for risk factors (including depression and substance misuse), breast feeding support and education, and child developmental screenings. Illinois also plans to cover home visiting services for new mothers and/or at risk children in FY 2019, targeting women who give birth to babies born with withdrawal symptoms.
Most benefit restrictions in FY 2018 or FY 2019 are narrowly targeted. Benefit restrictions reflect the elimination of a covered benefit, benefit caps, or the application of utilization controls for existing benefits. The most common benefit restrictions limited dental coverage (Alaska, Connecticut, Iowa, Kentucky, Nevada, and Oklahoma) or implemented new prior authorization requirements (Colorado and Nevada). Other notable benefit restrictions that are pending CMS approval include proposals in New Mexico and Utah to eliminate Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) coverage for individuals ages 19 and 20 in FY 2019 and Kentucky’s proposals to eliminate non-emergency medical transportation (NEMT) services for the Medicaid expansion group and eliminate NEMT for methadone services for all non-pregnant adults in FY 2019 (Table 15).
Copayments
Federal law limits cost-sharing for people with income below 100% FPL to “nominal” amounts (defined in federal regulations), with higher amounts allowed for beneficiaries at higher income levels. Certain groups are exempt from cost-sharing, including mandatory eligible children, pregnant women, most children and adults with disabilities, people residing in institutions, and people receiving hospice care. In addition, certain services are exempt from cost-sharing: emergency services, preventive services for children, pregnancy-related services, and family planning services. Also, total Medicaid premiums and cost-sharing for a family cannot exceed 5% of the family’s income on a quarterly or monthly basis.8
Most state Medicaid programs require beneficiary copayments, but to varying degrees. Thirteen states reported changes to copayment requirements in either FY 2018, FY 2019, or both years. Details about state actions related to copayments can be found in Table 16 and key changes are described below.
Eight states reported new or increased copayment requirements for FY 2018 or FY 2019. Key changes include:
- Five states (Colorado, Kentucky, Maine,9 Massachusetts, and New Mexico) reported new or increased copayments for non-emergency use of a hospital emergency department (ED). These changes are part of pending Section 1115 waiver requests in Kentucky, Maine, and New Mexico.
- Colorado, New Mexico, and Utah are adding or increasing pharmacy copayments. Colorado, Michigan, and Utah reported increased copayments for hospital outpatient services.
Nine states reported policies that eliminate or reduce a copayment requirement for some or all covered populations in FY 2018 or FY 2019. Key changes include:
- One state (Indiana)10 decreased copays in FY 2018 for non-emergency use of the ED to the state plan amount ($8). The state previously imposed graduated copays of up to $25 for non-emergency ED use under Section 1115 waiver authority.
- New Mexico is eliminating copayments for behavioral health services for working disabled adults and Michigan is eliminating behavioral health copays for all beneficiaries.
- Delaware is eliminating copayments for naloxone, Massachusetts is eliminating copayments for SUD treatment, aspirin, and statin drugs, and South Carolina is eliminating copayments for a subset of prescription drug classes deemed to be of the highest value.
TABLE 14: BENEFIT CHANGES IN ALL 50 STATES AND DC, FY 2018 AND FY 2019
| States | FY 2018 | FY 2019 | ||
| Enhancements/Additions | Restrictions/Eliminations | Enhancements/Additions | Restrictions/Eliminations | |
| Alabama | ||||
| Alaska | X | X | ||
| Arizona | X | |||
| Arkansas | ||||
| California | X | X | ||
| Colorado | X | X | X | |
| Connecticut | X | |||
| Delaware | ||||
| DC | X | |||
| Florida | ||||
| Georgia | X | |||
| Hawaii | X | |||
| Idaho | ||||
| Illinois | X | |||
| Indiana | X | X | ||
| Iowa | X | |||
| Kansas | X | |||
| Kentucky | X | X | ||
| Louisiana | X | |||
| Maine | ||||
| Maryland | X | X | ||
| Massachusetts | X | |||
| Michigan | ||||
| Minnesota | ||||
| Mississippi | X | |||
| Missouri | X | |||
| Montana | ||||
| Nebraska | X | |||
| Nevada | X | X | X | |
| New Hampshire | X | |||
| New Jersey | X | |||
| New Mexico | X | X | ||
| New York | X | X | ||
| North Carolina | X | |||
| North Dakota | ||||
| Ohio | X | |||
| Oklahoma | X | |||
| Oregon | ||||
| Pennsylvania | ||||
| Rhode Island | X | X | ||
| South Carolina | X | |||
| South Dakota | X | |||
| Tennessee | X | |||
| Texas | X | X | ||
| Utah | X | X | ||
| Vermont | X | |||
| Virginia | X | |||
| Washington | ||||
| West Virginia | X | X | ||
| Wisconsin | X | X | ||
| Wyoming | ||||
| Totals | 19 | 4 | 24 | 6 |
|
NOTES: States were asked to report benefit restrictions, eliminations, enhancements, and additions in FY 2018 and FY 2019. Home and community-based services (HCBS) and pharmacy benefit changes are excluded from this table. SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2018. |
||||
Table 15: States Reporting Benefit Actions Taken in FY 2018 and FY 201911
|
State |
Fiscal Year | Benefit Changes |
| Alabama | 2019 | Children (nc): Add coverage of Applied Behavior Analysis (ABA) services for individuals under age 21 (October 1, 2018). |
| Alaska | 2018 | Adults (-): Recategorize emergent and enhanced dental service codes, and eliminate coverage of other codes. |
| 2019 | Children (nc): Add coverage of Applied Behavior Analysis (ABA) services under the EPSDT benefit.
All (+) Pending Sec. 1115 Waiver: Begin phasing in a revised and expanded behavioral health services benefit package (TBD). |
|
| Arizona | 2018 | Non-LTSS Adults (+): Add a $1,000 per year benefit for emergency dental services (October 1, 2017).
Non-LTSS Adults (+): Add coverage of outpatient occupational therapy services (October 1, 2017). |
| California | 2018 | All (nc): Reaffirm coverage of non-emergency medical transportation as provided in state law (July 1, 2017).
Adults (+): Fully restore coverage for dental services (January 1, 2018). Children (nc): Expand coverage of Behavioral Health Treatment (BHT) to individuals under age 21 without a diagnosis of Autism Spectrum Disorder (ASD) (March 1, 2018). |
| 2019 | Adults (+): Add Diabetes Prevention Program (DPP) for individuals diagnosed with prediabetes who meet qualifying criteria (January 1, 2019). | |
| Colorado | 2018 | Pregnant Women (+): Add coverage of up to three postpartum depression screenings in the first year following a child’s birth (July 1, 2017).
Children (+): Restore coverage of routine circumcisions as an elective benefit (July 1, 2017). Adults (+): Add coverage for physical therapy/occupational therapy services above the 12-hour cap with prior authorization (November 1, 2017). |
| 2019 | All (+): Add coverage of 12-month supply of birth control pills, after an initial three-month dispensing period (January 1, 2019).
All (+): Expand non-emergency medical transportation (NEMT) services benefit to meet urgent transportation needs (January 1, 2019). All (-): Implement prior authorization requirements for certain medical benefits and physician administered drugs (January 1, 2019). All (-): Implement a comprehensive hospital admission review program (January 1, 2019). |
|
| Connecticut | 2018 | Adults (-): Apply $1,000 annual cap on coverage for dental services, with exception for medical necessity (January 1, 2018). |
| District of Columbia | 2019 | All (+): Add coverage of Clubhouse peer support services for individuals with a mental health diagnosis living in the community (TBD). |
| Georgia | 2018 | Children (nc): Add coverage for Autism Spectrum Disorders (ASD) services for individuals under the age of 21 (January 1, 2018). |
| 2019 | All (+): Add coverage of Emergency Medical Services (EMS) transportation to a non-hospital destination and treatment without transport (July 1, 2018).
Pregnant Women (+): Add coverage for group prenatal care services/CenteringPregnancy (October 1, 2018). |
|
| Hawaii | 2019 | Adults (+) Pending Sec. 1115 Waiver: Expand mental health and substance abuse benefits including addition of intensive case management and tenancy supports for beneficiaries classified as chronically homeless (TBD). |
| Illinois | 2019 | Adults (+): Restore adult dental benefit (July 1, 2018).
All (+) Approved Sec. 1115 Waiver: Add coverage of residential and inpatient treatment for individuals with substance use disorder at institutions for mental disease (IMD) under a statewide pilot (January 1, 2019). All (+) Approved Sec. 1115 Waiver: Expand coverage of the following behavioral health services through pilot programs approved under a Section 1115 waiver: clinically managed residential withdrawal management; substance use disorder case management services; peer recovery support services; crisis intervention services; and supported employment services (January 1, 2019). Pregnant women and children (+) Approved Sec. 1115 Waiver: Cover evidence-based home visiting services under a pilot program, including postpartum home visits and child home visits to postpartum mothers who gave birth to a baby born with withdrawal symptoms (January 1, 2019). Children (+) Approved Sec. 1115 Waiver: Add coverage of intensive in-home clinical and support services under a pilot program to support and stabilize a child/youth in their home or home-like setting (January 1, 2019). Children (+) Approved Sec. 1115 Waiver: Add coverage of respite services under a pilot program to provide families scheduled relief to help prevent stressful situations (January 1, 2019). |
| Indiana | 2018 | Adults (+): Add coverage of chiropractic spinal manipulation for Healthy Indiana Plan (HIP) Plus enrollees (January 1, 2018).
Adults (+) Approved Sec. 1115 Waiver: Expand coverage of opioid use disorder and substance use disorder treatment services to include inpatient substance use treatment at institutions for mental disease (IMD) (February 1, 2018). All (+) Approved Sec. 1115 Waiver: Add coverage for short-term low-intensity and high-intensity residential treatment for opioid use disorder and substance use disorder in settings of all sizes, including IMDs (March 1, 2018). All (+): Revise coverage for telemedicine services, including an elimination of the distance requirement between distant and originating sites (April 1, 2018). |
| 2019 | All (+): Add coverage for certain services provided by community health workers, including but not limited to patient education, health promotion, and facilitation of cultural brokering between an individual and their health care team (July 1, 2018).
All (+): Expand coverage for peer support recovery, crisis intervention, and intensive outpatient behavioral health services (TBD). |
|
| Iowa | 2019 | Adults (-): Apply a $1,000 annual maximum to dental benefits, excluding preventive services and dentures (September 1, 2018). |
| Kansas | 2019 | Adults (+) Pending Sec. 1115 Waiver: Add coverage of inpatient behavioral health services at publicly-owned and non-public institutions for mental disease (IMD) for Medicaid managed care enrollees (January 1, 2019). |
| Kentucky | 2018 | All (nc): Expand non-emergency medical transportation services to include travel to pharmacies (July 1, 2017). |
| 2019 | Adults (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Change access to enhanced benefits, such as vision and dental, such that individuals must access through My Rewards Account (TBD).
All (+): Approved Sec. 1115 Waiver: Add coverage of substance use disorder treatment services at institutions for mental disease (IMD) under pilot program (TBD). Expansion Adults (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Waive coverage of NEMT services (TBD). Adults (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Waive coverage of NEMT services for methadone treatment, with exceptions for children under age 21 (EPSDT), former foster care youth, and pregnant women (TBD). |
|
| Louisiana | 2018 | All (+): Remove home health visit limits (January 20, 2018).
Family Planning Eligibility Group (+): Remove family planning services visit limit (March 20, 2018). |
| Maryland | 2018 | Adults (+) Approved Sec. 1115 Waiver: Add coverage of substance use disorder residential treatment services in ASAM Level 3.3, 3.5, and 3.7 settings (July 1, 2017).
All (+): Add coverage of remote patient monitoring for beneficiaries who meet qualifying medical criteria (January 1, 2018). |
| 2019 | Adults (nc): Add coverage of audiology services and hearing aids (July 1, 2018).
Adults (+) Approved Sec. 1115 Waiver: Add coverage of substance use disorder residential treatment services in ASAM Level 3.1 settings (January 1, 2019). Dual Eligibles (+): Implement pilot for coverage of adult dental services (January 1, 2019). |
|
| Massachusetts | 2018 | All (+) Approved Sec. 1115 Waiver: Add coverage of recovery support navigator services and recovery coach services (March 1, 2018). |
| Michigan | 2018 | Adults (nc): Add coverage of hearing aids for adults age 21 and older (September 1, 2018). |
| Mississippi | 2019 | Children (+): Add coverage of pharmacist-administered vaccines for children ages 10 to 18 years old (TBD). |
| Missouri | 2019 | All (+): Add coverage of acupuncture and chiropractic services in lieu of an opioid prescription as an alternative pain management strategy (February 2019). |
| Nebraska | 2018 | All (+): Add coverage of nutrition services (July 1, 2017).
All (+): Add coverage of peer support services (July 1, 2017). |
| Nevada | 2018 | All (-): Implement a prior authorization requirement for hospice services (July 1, 2017).
Children (-): Limit coverage of orthodontia services (July 1, 2017). All (+): Add coverage of gender dysphoria services (January 1, 2018). All (+): Add coverage of medical nutrition therapy services (January 1, 2018). All (+): Add coverage of 12-month supply of birth control pills (January 1, 2018). Adults (+): Add coverage of podiatry services (January 1, 2018). All (nc): Expand definition of covered durable medical equipment services (June 26, 2018). |
| 2019 | All (-): Establish basic skills training services tiers (TBD). | |
| New Hampshire | 2019 | Adults (+) Approved Sec. 1115 Waiver: Add coverage of substance use disorder treatment services at institutions for mental disease (IMD) (TBD).
Expansion Adults (nc) Pending Sec. 1115 Waiver: Align alternative benefit package with standard Medicaid benefits as state terminates the current Premium Assistance Program and transitions Medicaid expansion beneficiaries into the state’s Medicaid managed care delivery system (January 1, 2019). |
| New Jersey | 2019 | All (+): Eliminate prior authorization requirements for nicotine replacement therapies (July 1, 2018).
Adults (+) Approved Sec. 1115 Waiver: Add coverage of short-term residential services for substance use disorder and withdrawal management services at an institution for mental disease (IMD) (July 1, 2018). Adults (+) Approved Sec. 1115 Waiver: Add coverage of long-term residential services for substance use disorder at an institution for mental disease (IMD) (October 1, 2018). Children (nc): Expand coverage of Autism Spectrum Disorder (ASD) services statewide (January 1, 2019). All (+): Add coverage of Diabetes Prevention Program services and self-management education (TBD). |
| New Mexico | 2019 | All (+) Pending Sec. 1115 Waiver: Add coverage of behavioral health services, substance use disorder treatment in adult residential treatment centers, expanded Opioid Treatment Program services, expanded provider types for Comprehensive Community Support Services, and teaming crisis treatment services (January 1, 2019).
All (+): Add coverage of Screening, Brief Intervention, and Referral to Treatment (SBIRT) services. All (+) Pending Sec. 1115 Waiver: Add coverage of inpatient services in an institution for mental disease (IMD) for beneficiaries with severe mental illness or a substance use disorder (January 1, 2019). Children (-) Pending Sec. 1115 Waiver: Waive coverage of Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) services for 19- and 20-year-olds (January 1, 2019). Pregnant Women (+) Pending Sec. 1115 Waiver: Pilot home visiting program that focuses on prenatal care, postpartum care, and early childhood development (January 1, 2019). Adults (+) Pending Sec. 1115 Waiver: Add coverage of pre-tenancy and tenancy support services to adults who are Seriously Mentally Ill (January 1, 2019). |
| New York | 2018 | All (+): Add coverage of digital breast tomosynthesis (DBT) screening services (September 1, 2017 for fee-for-service and November 1, 2017 for Medicaid managed care).
All (+): Add coverage of continuous glucose monitoring devices for beneficiaries with Type 1 diabetes (November 1, 2017 for fee-for-service and January 1, 2018 for Medicaid managed care). Children (+): Add coverage of pasteurized donor human breast milk for infants <1500 grams (December 1, 2017 for fee-for-service and February 15, 2018 for Medicaid managed care). |
| 2019 | All (+): Expand coverage of physical therapy services by increasing cap from 20 visits to 40 visits for eligible beneficiaries (July 1, 2018).
All (+): Add limited infertility benefit for beneficiaries between the ages of 21 to 44 (TBD, pending CMS approval). |
|
| North Carolina | 2019 | Adults (+): Add coverage of adult vision services (January 1, 2019).
Adults (+) Pending Sec. 1115 Waiver: Add coverage of substance use disorder services in institutions for mental disease (IMD) (TBD). |
| North Dakota | 2018 | All (nc): Update and clarify the services covered under the Rehabilitation Services benefit category, and the provider types who may render the service (April 1, 2018). |
| Ohio | 2018 | All (+): Expand coverage of behavioral health services to include assertive community treatment for adults, family counseling, intensive home-based treatment for youth at risk of out-of-home placement, and primary care services delivered by a behavioral health provider (January 1, 2018).
All (+): Expand provider types who may provide acupuncture services to treat pain (January 1, 2018). |
| Oklahoma | 2018
|
Adults (-): Limit cap on Targeted Case Management services from 25 units per month to 16 units per year (September 1, 2017).
Adults (-): Limit coverage of tooth extractions to emergency services only (September 14, 2017). Adults (-): Eliminate coverage of non-mandatory over-the-counter drugs (October 1, 2017). |
| Rhode Island | 2018 | Adults (+) Approved Sec. 1115 Waiver: Add coverage of Recovery Navigation Program services for individuals with substance use disorder. |
| 2019 | Adults (+) Approved Sec. 1115 Waiver: Add coverage of peer recovery specialist services for individuals with substance use disorder.
Adults (+) Pending Sec. 1115 Waiver: Add coverage of residential mental health and substance use disorder treatment services in institutions for mental disease (IMD) (TBD). All (+) Pending Sec. 1115 Waiver: Add coverage for a Behavioral Health Link triage center to support crisis stabilization and short-term treatment for individuals experiencing a mental health or substance use disorder crisis (TBD). |
|
| South Carolina | 2018 | All (+): Expand coverage of telemedicine services (July 1, 2017).
Children (nc): Add Autism Spectrum Disorder (ASD) services to the State Plan for eligible beneficiaries up to age 21 (July 1, 2017). |
| South Dakota | 2019 | Adults (+): Expand coverage of substance use disorder treatment services to all adults (SUD services were previously only covered for pregnant women) (July 1, 2018).
All (+): Expand definition of mental health practitioners (January 1, 2019). All (+): Add coverage of services provided by community health workers (April 1, 2019). |
| Tennessee | 2019 | Adults (+) Pending Sec. 1115 Waiver: Add coverage of inpatient and residential substance use disorder treatment services in institutions for mental disease (IMD) (TBD). |
| Texas | 2018 | Children (+): Add coverage for one postpartum depression screening for mother during infant’s Texas Health Steps medical visit during the first year (July 1, 2018). |
| 2019 | Children (+): Expand coverage of telemedicine services to occupational therapy and speech-language pathology provided in a school-based setting (TBD).
Adults (+): Add coverage of peer specialist services for adults with mental health conditions or substance use disorders (TBD). |
|
| Utah | 2018 | All (+): Add coverage of Screening, Brief Intervention, and Referral to Treatment (SBIRT) services for beneficiaries age 13 and older (July 1, 2017).
People with Disabilities (+): Add coverage of dental services for individuals with disabilities (July 1, 2017). Adults (+) Approved Sec. 1115 Waiver: Add coverage of residential treatment services in an institution of mental disease (IMD) for individuals with a substance use disorder (November 9, 2017). |
| 2019 | Children (-) Pending Sec. 1115 Waiver: Waive coverage of Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) services for certain 19 and 20 year olds (TBD). | |
| Vermont | 2018 | All (+): Add coverage of in-home lactation consultations (June 1, 2018). |
| Virginia | 2018
|
All (+): Add coverage for peer support services for beneficiaries with serious mental illness and/or substance use disorders (for all members other than family planning-only beneficiaries) (July 1, 2017).
Limited Adult Coverage Group (+) Approved Sec. 1115 Waiver: Expand coverage of residential addiction recovery and treatment services for beneficiaries with serious mental illnesses and/or substance use disorders in the GAP waiver population (October 1, 2017). |
| West Virginia | 2018 | Children (+): Add coverage of neonatal abstinence syndrome (NAS) treatment services (October 31, 2017).
All (+) Approved Sec. 1115 Waiver: Add coverage of screening, brief intervention, and referral to treatment (SBIRT) services (January 14, 2018). |
| 2019 | All (+) Approved Sec. 1115 Waiver: Add coverage of substance use disorder services, including adult residential treatment services, peer recovery support services, and withdrawal management services (July 1, 2018). | |
| Wisconsin | 2018 | Children (+): Redesign targeted case management services for children with complex medical conditions (September 1, 2017).
All (+): Eliminate prior authorization requirements for therapy services evaluations and re-evaluations (January 1, 2018). Children (+): Add coverage of pharmacist-administered vaccines for children ages six to 18 years old (January 1, 2018). Children (+): Eliminate prior authorization requirements for environmental lead investigation services (March 1, 2018). |
| 2019 | Adults (+) Pending Sec. 1115 Waiver: Add coverage of residential substance use disorder treatment services in institutions for mental disease (IMD) for managed care and fee-for-service populations (TBD). |
table 16: Copayment actions taken in the 50 states and dc, FY 2017 and 2018
|
State |
Fiscal Year | Copayment Changes |
| Colorado | 2018 | Increase (all non-exempt eligibility groups): Increase pharmacy copayment to $3.00 per prescription (January 1, 2018).
Increase (all non-exempt eligibility groups): Double the hospital outpatient copayments (January 1, 2018). Increase (all non-exempt eligibility groups): Increase emergency room copayment for non-emergency events (January 1, 2018). |
| Delaware | 2018 | Decrease (LTSS population): Treatment of pre-eligibility medical expenses in determining post eligibility cost of care contribution for LTSS population; “look-back” period expanded from 30 days to 90 days. Potential to reduce the monthly “patient pay” amount (July 1, 2017). |
| 2019 | Elimination (all eligibility groups): Eliminate copayment for naloxone (July 1, 2018). | |
| Indiana | 2018 | Decrease (for HIP 2.0 expansion population): Eliminating the graduated copayment for non-emergent ER use and replaced with a flat $8 copay (February 1, 2018) (Approved Sec. 1115 Waiver). |
| Kentucky | 2019 | Increase (Expansion Adults and Parents/Caretakers): MCOs will not be authorized to waive copayments that apply in fee-for-service (TBD).
New (Expansion Adults and Parents/Caretakers): Incentive account funds deducted for non-emergent use of the ER (Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering). New (Expansion Adults and Parents/Caretakers): Incentive account funds deducted for missed appointments (Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering). |
| Maine | 2019 | New (all non-exempt groups): Impose a copayment of $10 on all populations for non-emergent use of the ED (dual eligibles, those in institutions and a few other groups are exempt) (Pending Sec. 1115 Waiver). |
| Massachusetts | 2019 | Elimination (all groups): Eliminate pharmacy copays for SUD treatment, aspirin, and statin drugs (TBD).
Elimination (Persons with income at or below 50% FPL): Eliminate all copayments for those with income below 50% FPL (TBD). Increase (adults above 50% FPL); Implement new copayments for specialty services and non-emergent use of the emergency room (TBD). Decrease (all groups): Implementing a 2% cost-sharing cap for those below 150% FPL and 5% for those above 150% FPL (TBD). |
| Michigan | 2019 | Increase (all non-exempt groups): Increase outpatient hospital copay from $1 to $2 (October 1, 2018).
Elimination (all groups): Eliminate cost sharing for mental health and substance use disorder services (October 1, 2018). |
| Montana | 2018 | Increase (expansion population with incomes from 51% to 138% FPL): Premium credit of 2% eliminated and members now pay point of service copayments (January 1, 2018) (Approved Sec. 1115 Waiver). |
| New Hampshire | 2019 | Decrease (adult enrollees with incomes between 100% and 133% FPL): Cost sharing will be aligned with standard Medicaid (January 1, 2019) (Approved Sec. 1115 Waiver). |
| New Jersey | 2018 | Decrease (nursing facility residents): Personal needs allowance was increased from $35 to $50 per month (July 1, 2017). |
| New Mexico | 2018 | Elimination (for Working Disabled Adults): Eliminated copayments for behavioral health services (January 1, 2018). |
| 2019 | New (for most populations): Copays for brand-name prescriptions when there is a less expensive generic equivalent medicine available (March 1, 2019).
New (for most populations): Copays for non-emergent use of the emergency department (March 1, 2019) (Pending Sec. 1115 Waiver). New (for most populations): A fee of $5 for missing 3 or more appointments in a calendar year (March 1, 2019) (Pending Sec. 1115 Waiver). Elimination (for Working Disabled Adults): Eliminate most copayments (January 1, 2019). |
|
| South Carolina | 2019 | Elimination (all populations): Copayments eliminated for a subset of prescription drug classes deemed to be of the highest value. |
| Utah | 2018 | Neutral (all but children and pregnant women): Change inpatient copayments from $220 per year to $75 per stay (October 1, 2017).
Increase (all but children and pregnant women): Increase outpatient copayments (July 1, 2017). Increase (all but children and pregnant women): Increase pharmacy copayment from $2 to $4 per prescription (July 1, 2017). |