State Medicaid Programs Respond to Meet COVID-19 Challenges: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2020 and 2021
Long-Term Services and Supports
Medicaid is the nation’s primary payer for long-term services and supports (LTSS).1 State Medicaid programs must cover LTSS in nursing homes, while most home and community-based services (HCBS) are optional, which results in considerable differences among states in HCBS eligibility, scope of benefits, and delivery systems.2 The COVID-19 pandemic has greater implications for people who utilize LTSS, who may be at increased risk for adverse health outcomes if infected with coronavirus due to their older age, underlying health conditions, and/or residence in congregate settings. Members of the long-term care (LTC) workforce—which is predominantly female and low wage, and disproportionately Black—are also at elevated risk of coronavirus infection.3 LTC facilities have implemented many protocols to mitigate the spread of the virus, such as visitor restrictions and universal testing of residents and staff. These new measures have played an important role in reducing the number of new LTC cases and deaths in later months of the pandemic. 4 However, given the close relationship between community transmission and LTC cases and deaths, there is still enormous state-level variation in patterns of new cases and deaths in LTC facilities. Notably, LTC cases and deaths continue to rise faster in “hotspot” states than “non-hotspot” states.5 As of October 8, 2020, LTC facilities across the country had reported a total of over 500,000 cases of COVID-19 as well as nearly 85,000 deaths related to the virus.6
As the pandemic continues, states have taken a number of Medicaid policy actions to address the impact on seniors and people with disabilities who rely on LTSS to meet daily self-care and independent living needs. These actions include expanding eligibility and streamlining enrollment, easing premium and/or cost-sharing requirements, enhancing benefits, increasing provider payment, modifying provider qualifications, and altering reporting requirements. Many of these policy changes have been adopted through temporary authorities that, according to CMS guidance,7 will expire when the COVID-19 public health emergency (PHE) declaration ends or are otherwise time-limited. Prior to that time, policymakers will need to assess whether any changes can or should be retained and transitioned to other authorities.8
Survey Findings
To better understand the impact of COVID-19 on the LTSS direct care workforce, we asked states to indicate whether they had a variety of concerns about the pandemic’s impact on HCBS and institutional direct care workers. We also asked states about whether COVID-19 has impacted institutional/HCBS rebalancing efforts and whether it has impacted access to non-home and residential HCBS settings. Finally, we asked states to identify the top three LTSS policy changes adopted in response to COVID-19 that they plan to retain after the PHE period.
The majority of responding states reported concerns about the pandemic’s impact on the LTSS direct care workforce, with similar issues across HCBS and institutional settings (Figure 2). Specifically, states reported the following concerns:
- More than three-quarters of states reported concerns about reductions in LTSS direct care workforce supply as a result of the pandemic. At least five states reported that the LTSS direct care workforce supply was an issue prior to COVID-19 but has become a greater issue during the pandemic; in general, LTSS direct care workforce supply was an issue for many states prior to the pandemic.9 Using HCBS Appendix K emergency authority, some states are providing overtime and the use of legally responsible relatives (such as parents or spouses) as paid caregivers to address workforce supply issues.10
- Nearly all states reported concerns about access to personal protective equipment (PPE) for LTSS direct care workers. A few states noted that they were prioritizing supply of PPE for workers in institutional or congregate settings.11
- Nearly three-quarters of states reported concerns about access to COVID-19 tests for LTSS direct care workers. Several states reported the length of COVID-19 test processing times as a particular challenge.
- Over two-thirds of states reported concerns about COVID-19 infections among LTSS direct care workers. Several states noted that better access to PPE and testing would help mitigate concern about infections.
Some states noted some improvements since the beginning of the pandemic in workforce supply, access to PPE and testing, and ability to control infection rates, while a few states identified specific LTSS populations or geographic areas that presented particular issues or concerns. For example, a few states reported issues with workforce, testing, and infection rates specifically for the population with intellectual and developmental disabilities (I/DD). A small number of states noted that workforce issues, distribution of PPE, and testing (due to lack of transportation to testing sites) were of greater concern for rural areas.
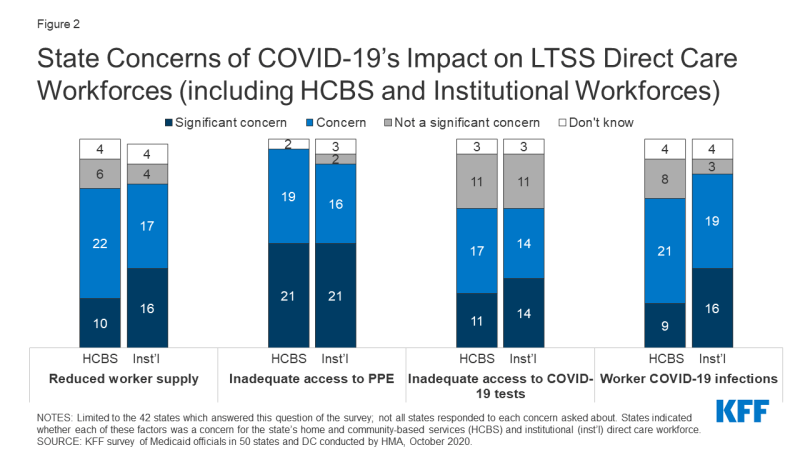
Figure 2: State Concerns of COVID-19’s Impact on LTSS Direct Care Workforces (including HCBS and Institutional Workforces)
State responses regarding COVID-19 implications on state institutional/HCBS rebalancing efforts were mixed. Most frequently, states did not expect the pandemic to have an impact on rebalancing efforts to support more people in community-based over institutional settings. Several states, however, indicated that the pandemic would halt or delay HCBS expansion and others reported that fewer nursing facility transitions to the community would occur. Fewer states indicated that the pandemic would likely drive further rebalancing. Several states reported that the potential impact was unknown and/or was under review. Finally, a few states specifically indicated that negative fiscal and budget impacts resulting from the pandemic may delay rebalancing. When asked about access to existing HCBS services, nearly all responding states reported reduced access to non-home HCBS settings such as adult day health and day habilitation as a result of the COVID-19 pandemic, while fewer states reported reduced access to residential HCBS settings. Although residential settings were less likely to be closed or eliminated in response to the pandemic, these settings were still impacted by the pandemic including by its effects on the direct care workforce (as described above).
States noted plans to retain a variety of LTSS policy changes adopted in response to COVID-19 after the PHE period ends, most commonly citing the continuation of telehealth expansions. As many LTSS emergency policy changes were adopted through time-limited temporary authorities (some of which will expire with the end of the PHE), states may need to assess how to retain changes and transition to other authorities.12 Fourteen states reported they are still evaluating whether LTSS policy changes will be continued and three states reported that there are no plans to retain LTSS policy changes after the PHE declaration or other Medicaid emergency authority (such as HCBS waiver Appendix K) expires. The remaining states indicated plans to continue policy changes including:
- Telehealth expansions. The majority of responding states reported plans to retain telehealth or remote provision of HCBS services (21 states), far exceeding all other types of LTSS policy changes reported. For example, a few states mentioned plans to continue allowing personal care monitoring to be delivered via telehealth. (See Benefits, Cost-Sharing, and Telehealth section for more information on state expansions of telehealth for services including HCBS.)
- Streamlined processes for LTSS eligibility determinations and service authorizations. Six states cited continued remote delivery of assessments, reassessments, and case management (Connecticut, Minnesota, North Carolina, North Dakota, Oklahoma, and Oregon). A small number of states also mentioned continuing to allow verbal consent and electronic signatures, accepting self-attestation to verify Medicaid applications for aged, blind and disabled populations, and streamlining utilization review. (See Eligibility section for more information on changes to eligibility determination processes.)
- Changes to provider enrollment processes. Five states reported an intent to keep changes made to LTSS provider enrollment and training processes including simplification, modified qualifications, and recruitment techniques (Florida, New Hampshire, North Dakota, Oregon, and Washington). A couple of states also mentioned an intent to retain remote provider site inspections.
- Increased access to paid family caregiver services. Three states reported plans to continue allowing family members to provide certain services (Connecticut, Maine,13 and North Dakota).14
- Other LTSS policy changes. Other types of policies cited for retention by one or two states include modifications to provider payments (such as providing overtime or tying nursing facility reimbursement to quality and infection control), expansions of settings where HCBS may be delivered (such as acute hospital settings), and increased access to certain benefits (such as home delivered meals and assistive technology).
