Racial and Ethnic Health Inequities and Medicare
COVID-19
COVID-19 Death Rates Among Hispanic, American Indian/Alaska Native, and Black Adults Ages 65 and Older are Nearly Double the Rate Among Older White Adults
People of color have experienced disproportionate rates of COVID-19 cases, hospitalizations, and deaths. Specifically, among adults ages 65 and older, the mortality rates per 100,000 people were higher for older Hispanic adults (1,050 deaths per 100,000), older American Indian/Alaska Native adults (966 deaths per 100,000), and older Black adults (900 deaths per 100,000) than for older White adults (561 deaths per 100,000) (Figure 24).
Among Adults Ages 65 and Older, COVID-19 Represents a Larger Share of Deaths Among People of Color than White People Since January 2020
Among older Hispanic adults, COVID-19 deaths account for 25% of all causes of death—2.3 times higher than the share among older White adults (11%) (Figure 25). For older American Indian/Alaska Native, Asian, Black, and Native Hawaiian or Other Pacific Islander adults, COVID-19 deaths account for 23%, 17%, 16%, and 16% of deaths from all causes, respectively.
COVID-19 Cases Are Higher Among American Indian/Alaska, Hispanic, and Black Beneficiaries Than Among White Beneficiaries
From January 1 to November 21, 2020, COVID-19 cases among American Indian and Alaska Native, Black, and Hispanic Medicare beneficiaries (4,598, 4,343, and 4,243 cases per 100,000 respectively) were 1.7, 1.6, and 1.6 times higher, respectively, than among White beneficiaries (2, 655 cases per 100,000) (Figure 26).
COVID-19 Hospitalization Rates Are Higher Among American Indian/Alaska Native, Black, and Hispanic Beneficiaries Than Among White Beneficiaries
From January 1, 2020 to November 21, 2020, hospitalization rates for American Indian/Alaska Native, Black, and Hispanic Medicare beneficiaries were 2.9 times, 2.7 times, and 2.1 times respectively, higher than White beneficiaries (592 hospitalizations per 100,000) (Figure 27).
Analysis of patient data from health records shows that in addition to having higher rates of infections, hospitalizations, and mortality, people of color have been more likely to require more intensive level of treatment at the time of COVID-19 diagnosis, such as inpatient hospitalization or the use of oxygen and ventilation. Further, the COVID-19 pandemic has exacerbated mental health outcomes among older Hispanic adults, with older Hispanic adults reporting higher rates of depression or anxiety (33%) than older White (23%), Black (26%), and Asian (17%) adults.
The CARES Act includes a provision requiring Medicare Part B to cover a vaccine for COVID-19 at no cost to Medicare beneficiaries. However, 35% of Black adults ages 18 and older say they would definitely or probably not get a vaccine even if it was deemed safe by scientists and offered at no cost, with about half (48%) saying they are not confident that the needs of Black people are being accounted for in the COVID-19 vaccine development process. This finding reflects well-founded medical mistrust among African Americans, based on a history of racial abuse and malpractice within the medical system, as exemplified by the Tuskegee syphilis experiment, involuntary medical experimentation of Henrietta Lacks,1 and ongoing forms of medical racism, such as under prescribing of pain medications for Black people due to racial bias.
Nursing Homes with Relatively High Shares of Black or Hispanic Residents Were More Likely to Have At Least One COVID-19 Death
Older adults in long-term care facilities, such as nursing homes, have also been disproportionately impacted by the COVID-19 pandemic, with long-term facilities accounting for 7% of total cases and 40% of total deaths in the U.S. More than half of nursing homes with a high share (defined as 20% or more of residents) of Black residents (63%) and Hispanic residents (55%) reported at least one COVID-19 death, compared to 37% of nursing homes with a high share of White residents (Figure 28).
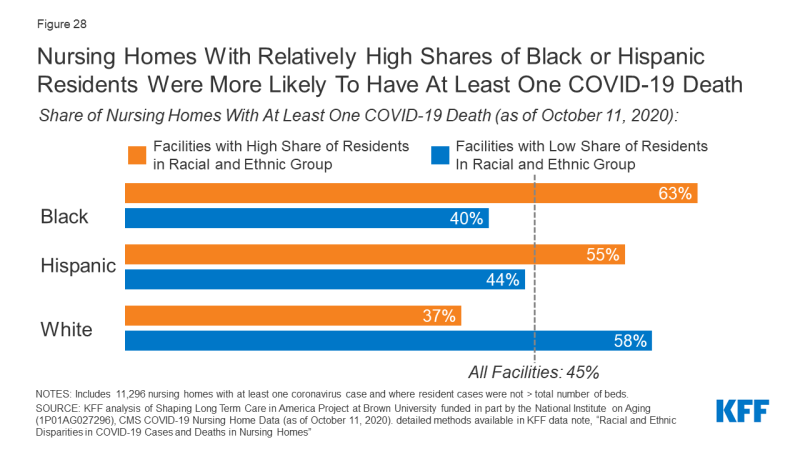
Figure 28: Nursing Homes With Relatively High Shares of Black or Hispanic Residents Were More Likely To Have At Least One COVID-19 Death
Nancy Ochieng, Juliette Cubanski, Tricia Neuman, and Samantha Artiga are with KFF. Anthony Damico is an independent consultant.
