Racial and Ethnic Disparities in COVID-19 Cases and Deaths in Nursing Homes
Long-term care facilities, such as nursing homes, have experienced a disproportionate share of deaths during the COVID-19 pandemic. The most recently available data show long-term care facilities account for 8% of all coronavirus cases but more than 40% of all COVID-19 deaths. Overall, COVID-19 has taken a disproportionate toll on communities of color. Black, Hispanic, and American Indian and Alaska Native (AIAN) populations have been shown to be at increased risk for cases, deaths, and hospitalizations. However, because the Center for Medicare and Medicaid Services does not require nursing facilities to report race/ethnicity data for COVID-19 cases and deaths, it is not possible to document the full scope of the pandemic on communities of color in nursing homes, or other long-term care settings. Only four states report cases and deaths in long-term care facilities by race/ethnicity (Iowa, Indiana, Louisiana, and Mississippi).
In the absence of these data, this analysis uses linked datasets – one with facility-level cases and deaths as of October 11th and another with 2017 facility-level resident information by race/ethnicity – to examine cases and deaths based on racial/ethnic composition of nursing home residents. Specifically, it assesses whether nursing homes with relatively high shares of Black and Hispanic residents experienced a disproportionate burden of cases and deaths compared to those with lower shares of Black and Hispanic residents as well as a higher share of White residents. Data were not available to separately analyze cases and deaths for other racial/ethnic groups. The analysis is based on data from 13,982 nursing facilities nationwide (approximately 93% of all nursing facilities). In addition to national data, we present similar results at the state level, where sufficient data are available. See methods for more details on how nursing homes were categorized, data limitations, and analytic approach.
Deaths and Cases by Resident Race/Ethnicity
Nursing homes with relatively high shares of Black or Hispanic residents were more likely to report at least one COVID-19 death than nursing homes with lower shares of Black or Hispanic residents (Figure 1). Overall, within the 13,982 nursing homes included in this analysis, 12% of all nursing home residents are Black and 6% are Hispanic. Our analysis finds deaths due to COVID-19 were more common among nursing homes with relatively high shares of Black or Hispanic residents (defined in this analysis as 20% or greater). Nationwide, 63% of nursing homes with a relatively high share of Black residents reported one or more COVID-19 death, higher than the share reported by nursing homes with a lower share of Black residents (40%). Similarly, 55% of nursing homes with a relatively high share of Hispanic residents reported COVID-19 deaths, higher than the share reported by nursing homes with a lower share of Hispanic residents (44%).
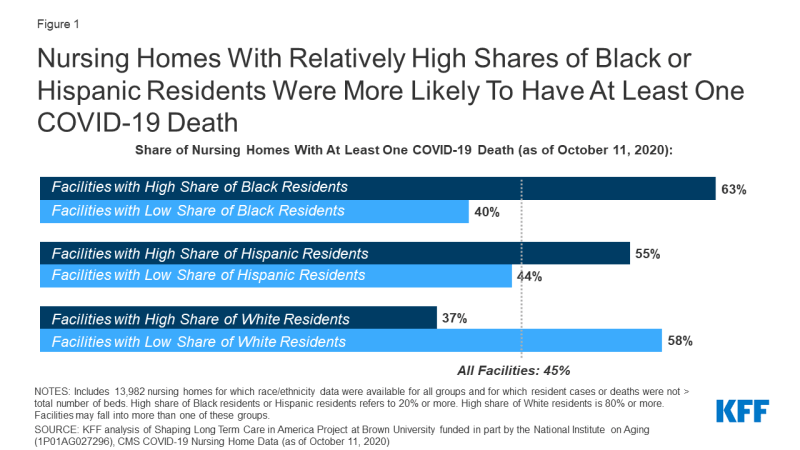
Figure 1: Nursing Homes With Relatively High Shares of Black or Hispanic Residents Were More Likely To Have At Least One COVID-19 Death
Nursing homes with relatively high shares of Black or Hispanic residents were more likely to report coronavirus cases than other nursing homes, although the differences are narrower than for reported COVID-19 deaths (Figure 2). Nursing homes with a high share of Black residents were more likely to report coronavirus cases than nursing homes with a low share of Black residents (87% compared to 79%). Similarly, nursing homes with a relatively high share of Hispanic residents were more likely to report coronavirus cases (84%) than nursing homes with a lower share (81%).
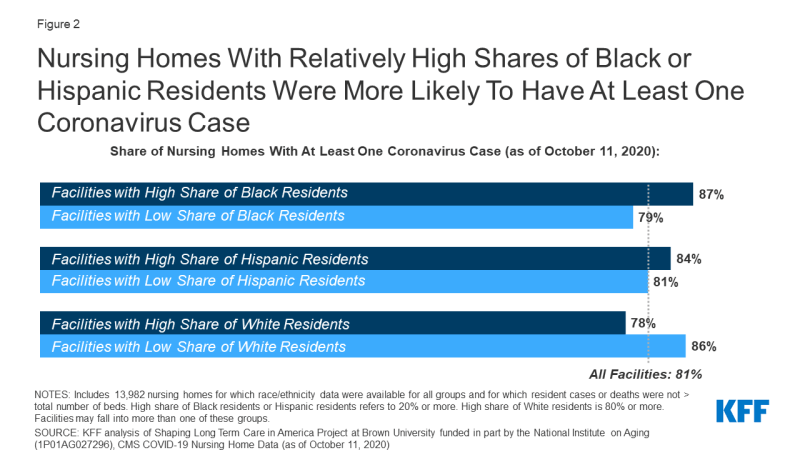
Figure 2: Nursing Homes With Relatively High Shares of Black or Hispanic Residents Were More Likely To Have At Least One Coronavirus Case
Case Outbreak Severity by Resident Race/Ethnicity
Among nursing homes that had at least one case of coronavirus, nursing homes with relatively high shares of Black or Hispanic residents reported more severe case outbreaks than nursing homes with low shares of Black or Hispanic residents, as measured by confirmed or suspected cases as a share of nursing home beds (Figure 3). In nursing homes with a relatively high share of Black residents, positive cases among residents account for 29% of beds, as compared to 25% of beds in nursing homes with a relatively low share of Black residents. Similarly, among nursing homes with a relatively high share of Hispanic residents, positive cases among all residents account for 31% of beds, as compared to 25% of beds in nursing homes with a relatively low share of Hispanic residents.
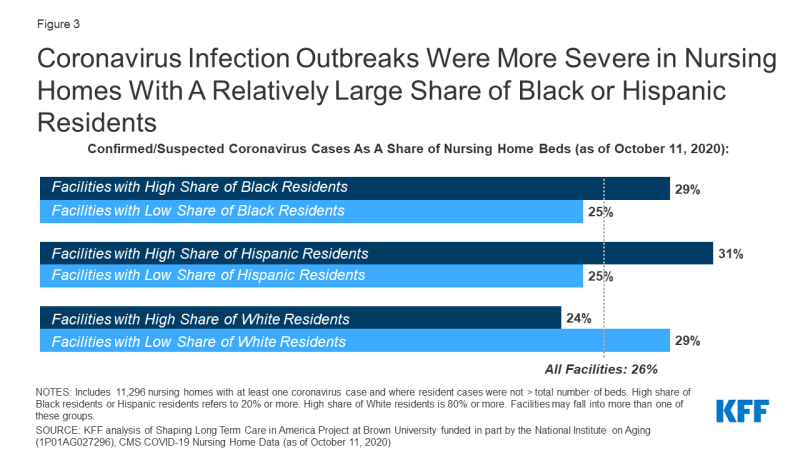
Figure 3: Coronavirus Infection Outbreaks Were More Severe in Nursing Homes With A Relatively Large Share of Black or Hispanic Residents
Cases and Deaths by Resident Race/Ethnicity in Select States
National patterns of COVID-19 deaths and cases in nursing homes with relatively high shares of Black or Hispanic residents generally persist at the state-level, based on data from 21 states. State-level analysis allows for a better understanding of whether observed national racial disparities may be attributed to regional outbreaks and geographic variations in the composition of the population by race/ethnicity. This analysis is limited to the twenty-one states with a sufficient number of nursing homes that had either a high share of Black or Hispanic residents, as described in greater detail in the methods section. Among these states, the experience of nursing homes with a high share of Black or Hispanic residents generally mirrored the national pattern.
In 19 of the 21 states for which there were sufficient data, nursing homes with a relatively high share of Black or Hispanic residents were more likely to report one or more death than other nursing homes in the state (Appendix Table 1). In some instances, these differences were relatively large, some with a gap of 20 percentage points or more. For example, in Florida, the share of nursing homes reporting one or more death due to COVID-19 was substantially higher among nursing homes with a high share of Hispanic residents than in other nursing homes (85% vs 63%). A similar gap between nursing homes with high and low share residents of Black residents was observed in five states (Illinois, Maryland, Michigan, New York, and Pennsylvania), where the gap in the share that reported at least one death was equal to or exceeded 20 percentage points. In Michigan, for example, 64% of nursing homes with a high share of Black residents reported 1 or more death, as compared to 35% in nursing homes with a low share of Black residents. The gap in the share of reported at least one death was not as pronounced in all states. For example, the gap between nursing homes with high versus lower shares of Black residents was fewer than 10 percentage points in Alabama, Florida, and Ohio.
Similarly, differences in the share of facilities that reported at least one case and case severity by resident race/ethnicity seen nationally generally also held in these states. Like the national data, state data shows that nursing homes with relatively more Black or Hispanic residents were more likely to report at least one COVID-19 case, though differences were less pronounced than death patterns; the exception to this pattern is Florida, Louisiana, North Carolina, and South Carolina where nursing facilities with higher and lower shares of Black residents were either equally likely to report at least one case (Florida and South Carolina) or facilities with a lower share of Black residents were slightly more likely to report a case (Louisiana and North Carolina).
With respect to the severity of outbreaks at the state level, the pattern observed at the national level was generally evident at the state level. However, in a few states, including Arkansas, Georgia, Louisiana, New Jersey, Ohio, and South Carolina, facilities with low shares of Black residents had equal or slightly more severe outbreak severity as facilities with high shares of Black residents.
Discussion
These findings confirm that nursing homes with a relatively large share of Black or Hispanic residents have been disproportionately affected by COVID-19, as measured by the share reporting deaths, share reporting cases, and the severity of outbreak. This analysis amplifies prior research that finds that the coronavirus has disproportionately impacted communities of color, including residents in nursing homes, potentially reflecting patterns of community transmission or nursing home quality. Research supports a strong relationship between nursing home cases and community transmission. There have been more mixed results when evaluating the relationship between nursing homes coronavirus outbreaks and nursing home quality, with some research finding a relationship and some not. Nursing homes are now required by the Center for Medicare and Medicaid services to report cases and deaths on a regular basis, but they are not required to report the data by race and ethnicity, and few states include such information in their own public reporting; such information is needed to document the direct impact of the pandemic on older residents of color, and the underlying factors that drive these disparities. Even without such data, this analysis makes it clear that residents in facilities that serve a relatively large share of Black and Hispanic residents have been disproportionately affected by the coronavirus.
