Public Health in Puerto Rico after Hurricane Maria
On September 20, 2017, Hurricane Maria made landfall in Puerto Rico. A “Category 4” storm when it hit the island,1 Maria was the strongest hurricane to hit Puerto Rico in almost a century, and it caused significant, widespread damage. The total number of people who died due to Hurricane Maria is unknown; as of November 4, officials have confirmed 55 deaths from the storm on the island, but the death toll is feared to be much higher.2
| Source: public domain image, contains materials originally from Central Intelligence Agency’s World Factbook. |
Hurricanes can have both near and long-term effects on public health (see Box 1). In Puerto Rico, these effects have been compounded by pre-existing fiscal, societal and health challenges. Drawing on federal and Puerto Rican government statistics and official statements, along with media reports, this issue brief provides a snapshot of key public health challenges in Puerto Rico after Hurricane Maria.
| Box 1. Public Health Effects of Hurricanes3 |
| The high winds and flooding from hurricanes have direct health impacts during the storm itself and immediately after. Storms can also damage infrastructure and interrupt essential needs and public systems such as shelter, food, water, electrical, transportation, and communication, which have indirect, and longer-term effects on public health.
Immediate/Short-term impacts:
Medium- and long-term impacts:
|
Status before the Hurricane
The Commonwealth of Puerto Rico is a U.S. territory located in the Caribbean, with a population of approximately 3.41 million residents as of July 2016.4 Puerto Ricans are U.S. citizens by birth. Prior to Hurricane Maria, Puerto Rico faced a number of economic and public health challenges. The island was already in the midst of a debt crisis, following years of economic recession, and in May of this year filed for bankruptcy relief.5 Close to half of Puerto Rico’s residents lived at or below the federal poverty level in 2016 (43.5%), compared to just 12.7% in the U.S. overall.6 The median household income in Puerto Rico over 2011-2015 was $19,350, almost one-third the median household income in the US overall ($53,889).7 The unemployment rate was estimated at 10.1%, a figure more than two times higher than that for US overall (4.1%).8
The health care system also faced challenges. Puerto Ricans were much less likely to have employer sponsored health insurance compared to rest of the U.S. (35% compared to 60%) and more likely to rely on Medicaid (49% compared to 20%), though a smaller proportion were uninsured (6% compared to 9%). Unlike the 50 US states and Washington, DC, Medicaid spending in Puerto Rico has been subject to a statutory cap, which means that under normal circumstances once federal funds are exhausted, the island no longer receives financial support for its Medicaid program for that fiscal year.9 Many residents of Puerto Rico access primary health care services through community health centers (CHCs), which rely heavily on federal Medicaid funding; there were 93 CHCs in Puerto Rico before the storm serving over 350,000 residents on the island, primarily in rural areas.10 In one indicator of basic health care access, the Health Resources and Services Administration (HRSA) estimated that at the end of 2016, there were just over 19,000 people living in primary “healthcare provider shortage areas” (HPSAs) with just 32% of the need for physicians in these areas being met.11
Basic health statistics in Puerto Rico also indicate that the island faced significant health concerns even before the storm. Puerto Ricans were much more likely to report having fair or poor general health compared to the U.S. overall (34% compared to 18%). The percentage of people living with a disability (estimated for 2011-2015) was 15.4% compared to 8.6% in the U.S. overall.12 Puerto Rico had a higher percentage of low-birthweight infants and a higher infant mortality rate compared to the US overall. The prevalence of diabetes was 50% higher in Puerto Rico compared to the rest of the U.S., including a death rate due to diabetes that was more than three times higher.13 The HIV death rate in Puerto Rico was nearly four times higher than that of the U.S. overall, and second highest of any state, territory, or federal district in the country (after Washington D.C.) in 2014. The number of people living with HIV in Puerto Rico in 2014 was estimated at 17,072, which represented one of the highest rates of people living with HIV per 100,000 in the U.S.
Puerto Rico has also seen outbreaks of mosquito-borne viral diseases over the last several years, including dengue, chikungunya, and Zika. Zika was first detected on the island in December 2015, and since that time Puerto Rico has reported the vast majority (84%) of all U.S. Zika cases. In 2016, the island experienced almost 35,000 symptomatic cases of Zika infection, compared with 6,218 cases in the rest of the U.S. and territories.14 So far in 2017 there have been far fewer Zika cases in Puerto Rico; 476 infections were reported through October (433 cases were reported in the rest of the U.S./territories). Some public health experts believe the decline in cases stems from the fact that a large proportion of the population was infected earlier and is now immune, creating a level of “herd immunity.”15 Still, the potential for further Zika outbreaks does exist. Other endemic infectious diseases of concern in Puerto Rico include leptospirosis, a serious, sometimes fatal bacterial infection usually transmitted via exposure to contaminated surface water.
Post-Hurricane Public Health Status
Hurricane Maria has significantly damaged key transportation, communication, and electricity infrastructure across the island which in turn have exacerbated already challenged health conditions. Immediately after the hurricane, there was virtually no electricity, available water, or transportation access on the island. On October 12, three weeks after the hurricane struck, only 392 miles of Puerto Rico’s 5,073 miles of roads were open according to the Federal Emergency Management Agency;16 it is unclear how many of the islands’ roads remain impassible now. Damage to cell towers and antennae, still being repaired, has left a reported 28% of people without telecommunication access as of November 8. While access to electricity has been increasing, it stood at 43% on November 16 (by comparison, the percent of population with access to electricity at the global level is over 80%; the country with the lowest access in the world, Papua New Guinea, has 40%); the remainder rely on generators or go without power. The ongoing power outage on the island has been named the “largest blackout in American history”.17 On November 9 and again on November 14, major power outages following power line failures and technical issues at the main power plant left 80% of the island without power, underscoring systemic weaknesses in the power grid.18,19 The goal of the Puerto Rico government is to be able to restore power to 50 percent of the population by the end of November, and power to all by spring or summer 2018.
With these broader issues in mind, major public health concerns on Puerto Rico post-hurricane include the following:
Mortality
The official death toll on Puerto Rico from Hurricane Maria, as of November 4, stood at 55, primarily from more immediate impacts, but this is widely understood to be an underestimate.20,21,22 Officials have stated that there were 472 additional deaths in September 2017 compared to September 2016, though the cause of many of these excess deaths or their potential link to the hurricane has not been certified.23 Barriers to an accurate and updated accounting of deaths include insufficient resources and challenges in transportation, communication, and organization in confirming and certifying causes of death. The official count of the number of deaths caused by the Hurricane is likely to increase over time as more deaths and their causes are counted and confirmed and longer term health complications set in.
Food, Water and Sanitation
Many island residents have had difficulties accessing groceries and fresh food, relying on meals provided by FEMA, the Red Cross, World Central Kitchen, and other entities. According to Puerto Rico officials, emergency responders are still providing 1 million meals per day on the island as of the first week of November.24 Lack of access to adequate food results in malnutrition, which can cause and exacerbate other health issues.
Right after the storm, access to water was minimal, with water treatment and pumping stations knocked out by the storm. Even by October 1, almost two weeks later, it was still at less than 50%. Since that time, access has increased slowly (see Figure 1). As of November 16, Puerto Rico’s water authority reports that 91% of the population had access to water, leaving about 9% (about 300,000 people) still without access. While the percentage with access in Puerto Rico has been improving over time (see Figure 1), it is still variable across the territory. San Juan metro region has the highest percentage with access to potable water (97%), while the West region has the lowest (86%). While the water authority reports the water is safe to drink, the Puerto Rico health department is still recommending residents boil or otherwise disinfect all water before drinking or cooking.
Some of those without access to safe water have been using natural fresh water sources such as ponds, lakes, and streams. Ingesting or other exposure to untreated fresh surface water is potentially dangerous due to possible contamination with disease-causing microbes. While no official case numbers are available, there are many reports in the media, from health care providers on the island, and from government officials that there has been an increase in conditions related to unclean water, ranging from vomiting and diarrhea to conjunctivitis (pink eye), scabies and asthma.25,26 In addition, by the end of October Puerto Rico had already reported 121 cases and 4 confirmed deaths from leptospirosis since the hurricane (compared to about 60 cases in total in a regular year)2728 One difficulty in diagnosing infectious diseases is that public health laboratory testing on the island has been interrupted due to damage from the storm.29
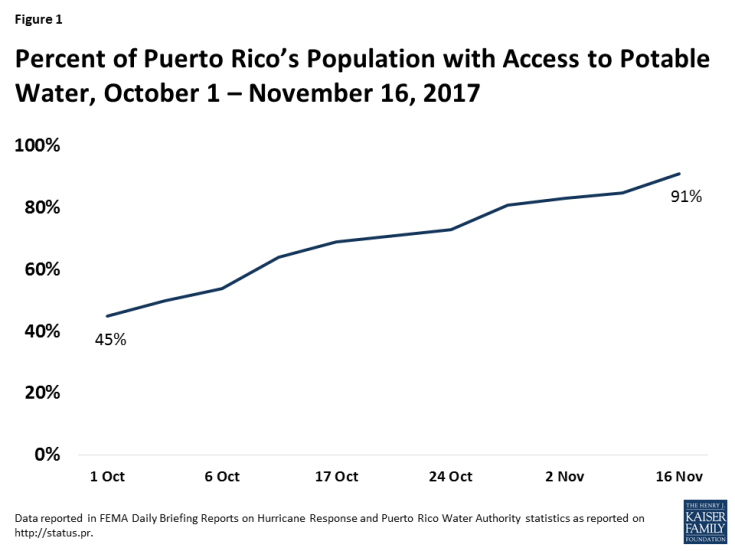
Figure 1: Percent of Puerto Rico’s Population with Access to Potable Water, October 1 – November 16, 2017
Another concern is the leaching of raw sewage or other contamination into drinking water sources. A reported 20 of the island’s 51 sewage treatment plants were out of service as of October 17, due mainly to lack of power. As a result, sewage has been identified as contaminating sources people are using for drinking water.30 In addition, the water authority briefly distributed water taken from a well at an EPA-designated groundwater contamination (“Superfund”) site,31 but this is no longer the case. Authorities have barred residents from accessing water at other groundwater wells with potentially dangerous levels of chemical or other contamination.
Health Care Infrastructure
Hospitals and other health care infrastructure suffered extensive damage from the storm, and most hospitals were left without electricity and with limited access to generators with fuel. Only three major hospitals were functioning on the island three days after the hurricane, but repair has progressed since then. At this point, while all hospitals tracked by the Puerto Rico government are open and functioning, 26 of the 65 hospitals (40%) with available information were still running on generators rather than regular electric power as of November 8.32 This means power may be available on an intermittent or limited basis (especially when generators fail or run out of fuel), which can result in the need to rely on alternative light sources such as flashlights when conducting surgery or providing other medical care.33,34 Community health Centers (CHCs) have also been affected by the storm, with 10 of the 93 (11%) CHC sites reported closed as of October 20 (four weeks after the hurricane); it is unclear how many remain closed currently.35
Given the high burden of diabetes on Puerto Rico, dialysis centers are an important part of the health care system. Almost all of the island’s 47 dialysis centers lost power after the Hurricane, though most of these centers have now re-opened. Still, many dialysis centers do not have regular electrical power and must rely on generators. Generator power has failed at some dialysis centers, and patients have been transported to other areas (including some to the continental U.S.) for treatment.36
In another indicator of the challenges faced by Puerto Ricans in accessing health care on the island, the latest estimates from HRSA indicate that 1,689,212 people – almost half of the population –lived in HPSAs as of November 7, with less than 2% of the need for physicians being met.37
Other Infectious Diseases
As mentioned above, Puerto Rico faces a number of endemic mosquito-borne diseases such as Zika, dengue, and chikungunya. Although it is common for mosquito populations to increase in the weeks after major rain events, raising the potential risk for mosquito-borne disease outbreaks, at this time there is no evidence that the island is experiencing any large-scale outbreaks of these diseases. Likewise, Puerto Rico faced a significant public health challenge from HIV prior to the hurricane, so there is increased concern about people living with HIV, and their access to medicines and other support services. While HIV program authorities on the island continue to face intermittent communication and power challenges, thus far no major interruptions in services have been reported or are evident and all Ryan White HIV/AIDS Program funded clinics are open.38
Mental Health
Media reports and statements from public health officials on the island indicate that many Puerto Ricans are struggling with mental health issues in the wake of the hurricane. Thirty-two suicides have been reported and demand for mental health services has increased sharply in the nearly two months since the storm struck.39 Anxiety and depression are frequently reported, even by those who never experienced these issues before. An ongoing concern is lack of access to drug treatment and and mental health services for those who need them. Mental health concerns may even increase over the coming months and years as people move beyond the immediate crisis and attempt to return to a normal life. Studies of those affected by Hurricane Katrina, for example, found that rates of mental illness remained elevated for more than a year after that disaster.40,41
Conclusion
Given the state of emergency on the island and the fact that many basic services are still not fully functioning, the full impact of the Hurricane on public health is difficult to assess. What is clear is that even before Hurricane Maria struck Puerto Rico, the island faced a host of economic and public health concerns, and that the storm exacerbated many of these challenges while introducing new ones. Concerns may change over time as the immediate crisis response transitions to recovery, and additional health issues may manifest over the longer-term. Ultimately, the public health toll from the storm on the people of Puerto Rico will depend on a number of factors including the level and effectiveness of external support, and continued attention to and funding for response and recovery from policymakers now and going forward.

