Modern Era Medicaid: Findings from a 50-State Survey of Eligibility, Enrollment, Renewal, and Cost-Sharing Policies in Medicaid and CHIP as of January 2015
Eligibility and Enrollment Systems
In order to implement the new modernized, data-driven enrollment and renewal processes outlined in the ACA, most states needed to make major improvements to or build new Medicaid and CHIP eligibility determination systems, often replacing decades-old legacy systems. Harnessing technology within Medicaid and CHIP can enhance the consumer experience and improve the reliability, timeliness and administrative efficiency of eligibility determinations and ongoing case management for enrollees. To support system upgrades and builds, the federal government provided 90 percent federal funding for system design and development. This increased funding was initially set to expire at the end of 2015, but, in October 2014, CMS announced plans to extend the higher federal match permanently.1 The ongoing availability of enhanced funding will give states more time to phase in additional functionality and help systems stay current as technology evolves in the future. States have made significant progress developing efficient, interconnected eligibility and enrollment systems, but ongoing efforts will be needed to refine and enhance systems to fulfill the vision of the ACA.
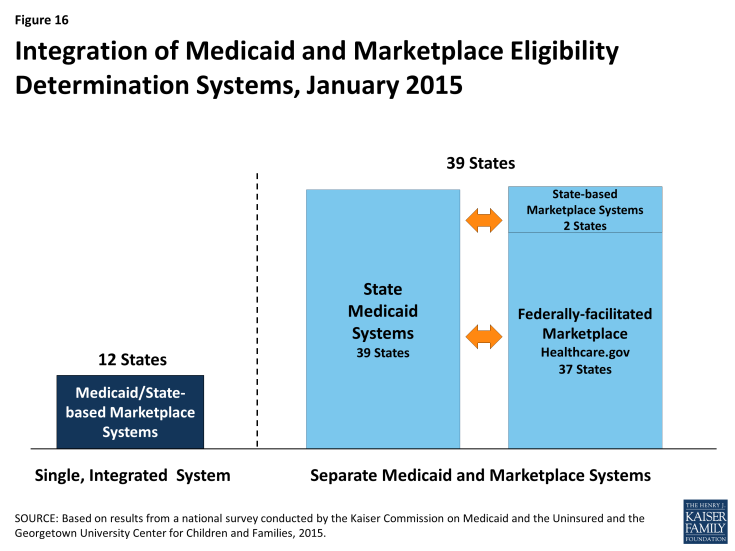
States have made varied choices with regard to the integration of their Medicaid and Marketplace eligibility determination systems, largely influenced by their Marketplace structure. All states must have a Medicaid eligibility determination system, but SBM states may operate a single, integrated system that makes eligibility determinations for both Medicaid and Marketplace coverage, which 12 states do. In the remaining 39 states, separate eligibility determination systems are used for Medicaid and Marketplace coverage. These include two SBM states that have separate state-level systems, three SBM states that are relying on the FFM for Marketplace eligibility and enrollment functions, and all 34 FFM and Partnership Marketplace states (Figure 16). Nearly all states with a separate CHIP program (34 of 36) have integrated CHIP into their Medicaid eligibility determination system.
When systems are not integrated, coordination between Medicaid and Marketplace systems is key to smooth enrollment. The SBM states with a single integrated Medicaid and Marketplace eligibility determination system do not need to transfer accounts between systems to coordinate eligibility determinations across coverage programs, although, in some cases, transfers of data and additional actions must occur after the eligibility determination to complete enrollment. However, in states with separate systems, including all 37 states relying on the FFM for eligibility and enrollment functions, electronic data, known as account transfers, must be exchanged between systems to provide a coordinated, seamless enrollment experience for individuals, as envisioned by the ACA. Ten of the FFM states have authorized the federal system to make final Medicaid eligibility determinations, which can speed the enrollment process. Alternatively, 27 states allow the FFM only to assess rather than determine Medicaid eligibility. These states must review accounts transferred from the FFM and potentially check other data sources or gather additional information from applicants prior to making a final Medicaid eligibility determination. There were technical difficulties with Medicaid and Marketplace coordination during 2014 that contributed to some delays in Medicaid enrollment. The federal government and states have sought to address these issues for 2015, but the extra steps needed to determine eligibility, along with the higher volume of applications generated during open enrollment, may still result in backlogs in some states.2
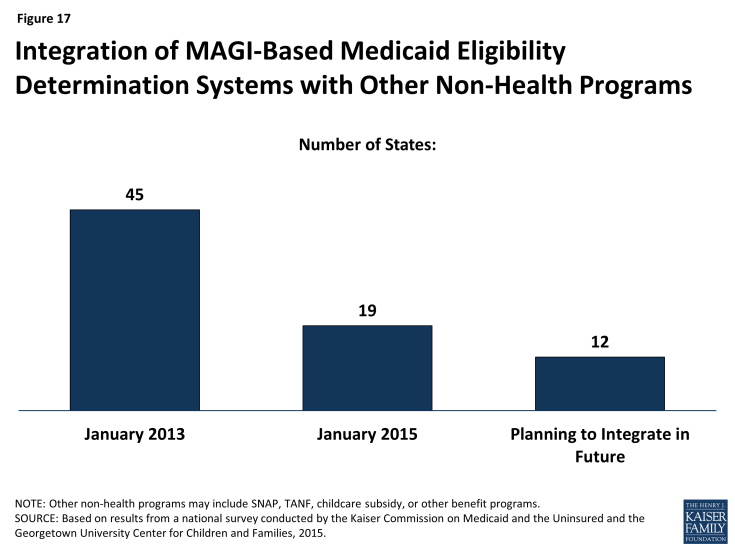
Many states delinked Medicaid eligibility determination systems from other benefit programs as they deployed new MAGI-based systems, but a number plan to reintegrate eligibility for other programs in the future. Prior to the ACA, the majority (45) of state Medicaid eligibility determination systems were integrated with other assistance programs, such as SNAP or TANF. As states implemented new ACA eligibility determination and enrollment processes for Medicaid and upgraded or built new eligibility systems, many delinked Medicaid from these other programs due to the large scale of the changes. As of January 1, 2015, 19 states maintain systems that administer eligibility for Medicaid and other benefit programs (Figure 17). However, this number will likely grow over time, as 12 states indicate that they plan to phase in other assistance programs in 2015 or beyond. These efforts are further supported by CMS’ intent to extend the opportunity for non-health programs to pay only the add-on costs associated with integrating into newly enhanced Medicaid systems through 2018.3