Medicare Part D at Ten Years: The 2015 Marketplace and Key Trends, 2006-2015
Section 5: Part D Performance Ratings
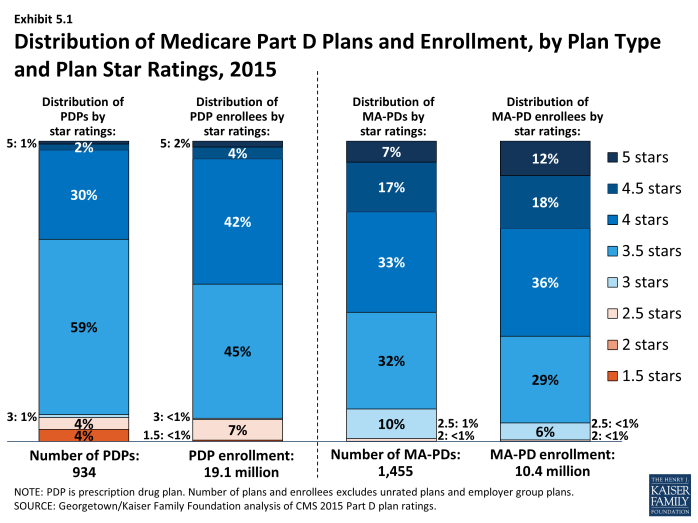
Nearly half (48 percent) of all PDP enrollees are in plans with ratings of four stars or higher, and most of the rest (45 percent) are in plans with average ratings (3 and 3.5 of 5 stars). But about 7 percent are in plans with low ratings (fewer than 3 stars) (Exhibit 5.1). A higher share of MA-PD plan enrollees (65 percent) are in plans that are rated four stars or higher for the drug plan rating measures (Medicare Advantage plans also have star ratings based on Part A and Part B services).
CMS has reported performance ratings for Part D plans since the fall of 2006 and has used a five-star scale since the fall of 2008.1 In 2015, the Part D ratings are based on 13 measures in 4 categories. Over time, CMS has moved toward more use of outcome and patient experience measures (such as medication adherence for statins or diabetes medications), rather than process measures (such as call center performance). For 2015, the agency dropped two measures (call center foreign language interpreter and TTY availability, beneficiary access and performance problems), but did not add any new measures. In contrast to the ratings for Medicare Advantage plans, however, CMS does not use quality ratings for Part D plans to determine bonus payments to these plans. Nor does CMS use ratings when making plan assignments for LIS beneficiaries.
Overall Part D plan ratings in 2015 are up considerably from 2014. The degree to which differences reflect changing performance by the PDPs or modifications of the rating measures used by CMS is unclear. In 2015, the share of enrollees in plans with 4 or more stars rose from 5 percent to 48 percent. Plans offered by the two firms with the most enrollees (Humana and UnitedHealth) gained a half star to shift from 3.5 to 4.0. About 91 percent of PDPs have ratings of 3.5 stars or higher in 2015, compared to 50 percent of PDPs in 2014 and 39 percent of PDPs in 2013. Plans offered by CVS Health gained two stars as they emerged from CMS-imposed sanctions, and plans offered by Aetna, Cigna, and WellCare each gained a half star, moving from 3.0 to 3.5 stars. About 89 percent of MA-PD plans have drug plan ratings of 3.5 stars or higher in 2015, nearly the same share as PDPs.2 But more MA-PD plans have the highest ratings; about 24 percent have 4.5 or 5.0 stars, compared to just 3 percent of PDPs.
Based on the pattern of enrollment by plan ratings, there is little evidence to suggest that beneficiaries use ratings to guide their enrollment decisions. In 2015, the share of PDP enrollees in plans with relatively high ratings (3.5 stars or more)—92 percent—is nearly identical to the share of PDPs (91 percent) with those ratings (Exhibit 5.1). However, an analysis of plan switching between 2009 and 2010 shows that enrollees in plans with at least 4 stars were actually more likely to switch than those in lower rated plans (16 percent versus 10 percent). The analysis also shows that those who did switch plans were only slightly more likely to end up in a higher-rated plan (29 percent versus 20 percent).3 In focus groups, most seniors on Medicare said they were not aware of the star ratings. Overall, they thought ratings could be helpful, but thought they were unlikely to be a major factor in their plan choice.4 More research is needed to determine the role of performance ratings on individual beneficiary choices.
Under current CMS policy, plans with ratings of less than 3 stars for three years in a row are subject to a special “low performance” flag on the Medicare Plan Finder website and may have their contracts terminated. In 2015, no PDPs and only 14 MA-PD plans have this designation, with a total of about 80,000 enrollees. Anthem had received this designation for the past two years for its MedicareRx Rewards Standard and Plus PDPs (about 48,000 enrollees in 24 regions), but the firm terminated these plans at the end of 2014.
Starting in 2012, beneficiaries have been eligible at any time outside the regular open enrollment period to switch from their current drug plan to a PDP with a 5-star rating (or a MA-PD plan with an overall 5-star rating). The only firms offering PDPs with 5-star ratings in 2015 actually had fewer enrollees in 2015 than in 2014 (289,000 versus 296,000). Among MA-PD plans, 102 plans with about 1.2 million enrollees earned five stars. They include 21 Kaiser Permanente plans with about half of the enrollees and a variety of other plans sponsored by different firms. Information is not available on how many people have used this special enrollment period, but aggregate monthly enrollment numbers suggest that most Part D enrollees have not acted on this option.