HIV and the Opioid Epidemic: 5 Key Points
Background
The opioid epidemic represents a significant and worsening public health crisis in the United States. In 2016, 2.1 million Americans were estimated to have an opioid use disorder and nearly 12 million to have misused opioids at some point during the preceding year.1 Death rates from opioid overdoses nearly doubled between 2012 and 2016, rising from 7.4 to 13.3 per 100,000, and in 2016, an estimated 115 people per day died of an opioid overdose.2
As the opioid epidemic has worsened, there has been growing concern about how injection drug use might fuel transmission of infectious disease. Those misusing opioids commonly move from oral use to insufflation to injection use.3 In fact, an estimated 10-20% of people who abuse prescription opioids move on to inject either opioids or heroin.4 Injection drug use increases the risk of blood-borne infections including HIV, hepatitis, and bacterial endocarditis, which spread efficiently through needle sharing.
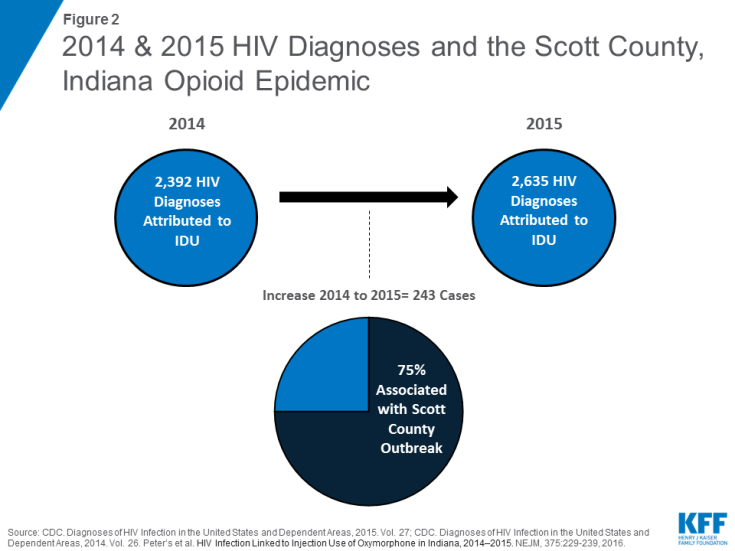
In 2015, opioid use resulted in an HIV outbreak in Scott County, Indiana, with 181 individuals diagnosed with HIV by year-end, most of whom were co-infected with hepatitis C (HCV).5,6 In response to this outbreak and the threat posed by the opioid epidemic more broadly, the Centers for Disease Control and Prevention (CDC) identified 220 jurisdictions particularly vulnerable to a similar type of outbreak in an effort to detect and prevent additional events.7 Indeed, recent reports suggest new outbreaks may in fact be occurring. In the context of HIV, this has raised particular concerns given that, prior to the opioid epidemic, HIV infections due to injecting drug use had fallen dramatically.
This graphic series highlights key things to know about the intersection of the nation’s HIV and opioid epidemics.
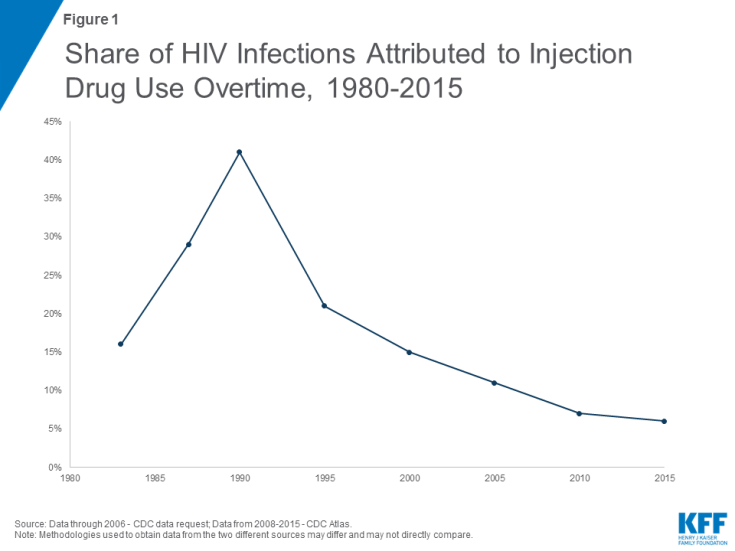
1. The decline in HIV infections associated with injection drug use has been a major success in the fight against HIV in the U.S., with the share of new HIV infections attributed to injection drug use falling from an estimated 40% in 1990 to just 6% in 2015.
2. However, 2015 marked the first time in two decades where the number of HIV diagnoses attributed to IDU increased, largely associated with the opioid epidemic and subsequent HIV outbreak in Scott County, Indiana. (Early data suggests a decline in 2016, back to 2014 levels, after the peak of this localized outbreak.)8
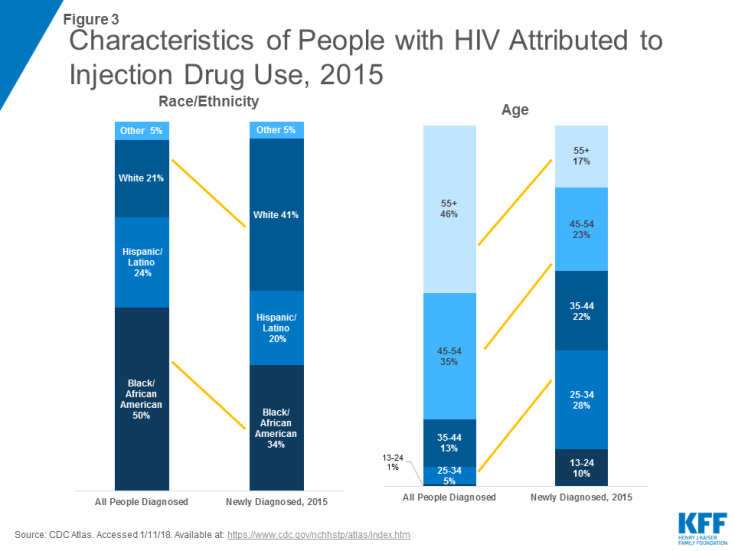
3. The demographics of people with HIV attributed to injection drug are increasingly similar to those most at risk for opioid use and addiction, with greater shares of those newly diagnosed being white and younger, relative to earlier years in the epidemic.
4. While there are several proven strategies available to reduce risk of infectious disease associated with injection drug use, including the provision of Syringe Exchange Programs (SEPs), access varies significantly across the country and does not always align with opioid epidemic epicenters.9 Of the 220, mostly rural, counties CDC determined were potentially vulnerable to an HIV or HCV outbreak among people who inject drugs, just 8% have an SEP in place.10,11
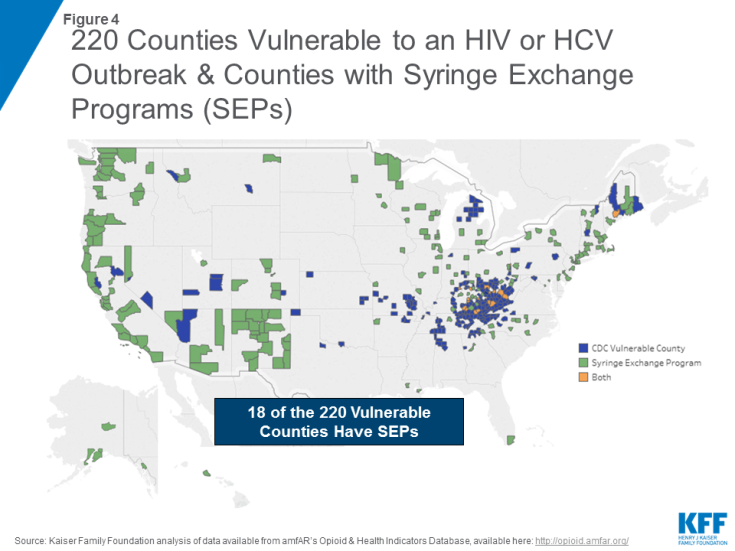
Figure 4: 220 Counties Vulnerable to an HIV or HCV Outbreak & Counties with Syringe Exchange Programs (SEPs)
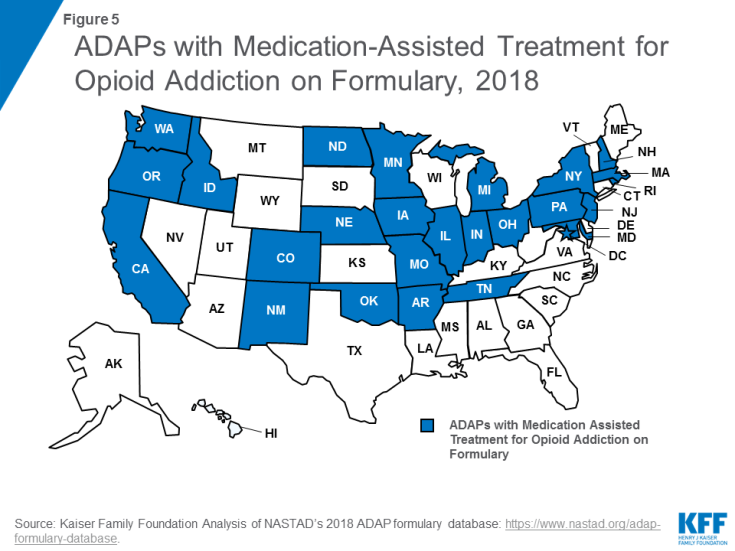
5. While all Medicaid programs and some private plans cover Medication-Assisted Treatments (MATs) to address substance use problems, the AIDS Drug Assistance Program (ADAP) of the federal Ryan White HIV/AIDS Program offers an additional source of support for people with HIV with limited or no insurance coverage.12,13 However, access varies across the country with just half (26) of state ADAPs covering at least one of the three commonly prescribed MATs for opioid addiction.14,15