Health Coverage and Care for the Adult Criminal Justice-Involved Population
Introduction
Individuals transitioning into and out of the criminal justice system include many low-income adults with significant physical and mental health needs who face a variety of economic and social challenges. The Affordable Care Act (ACA) coverage expansions, particularly the Medicaid expansion, provide new opportunities to increase health coverage for this population, which may contribute to improvements in their ability to access care as well as greater stability in their lives and reduced recidivism rates. This brief provides an overview of the adult criminal justice-involved population and the potential impacts of the ACA on their health coverage. (For information on health coverage and care for youth in the juvenile justice system, see: https://www.kff.org/medicaid/issue-brief/health-coverage-and-care-for-youth-in-the-juvenile-justice-system-the-role-of-medicaid-and-chip/.)
The Criminal Justice System
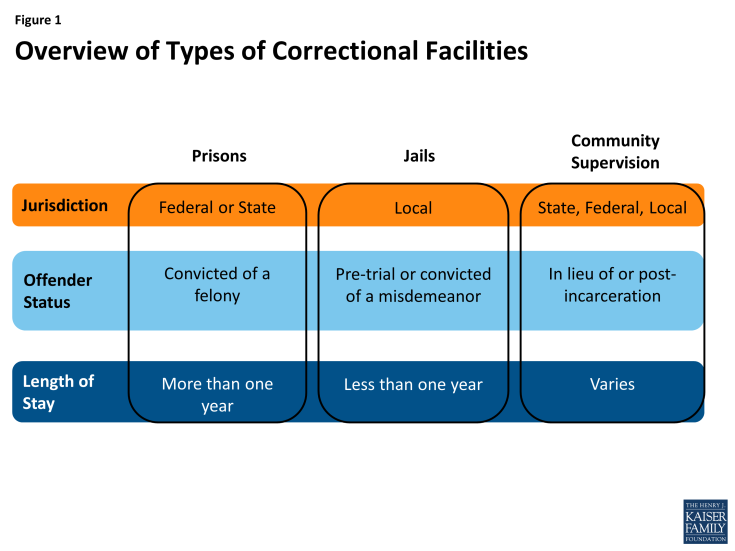
The criminal justice system is comprised of a range of different types of correctional facilities (Figure 1). Correctional facilities include prisons, which typically house longer-term felons or inmates serving a sentence of more than one year, and jails, which house individuals awaiting trial or sentencing and those convicted of misdemeanors and serving shorter terms that are typically less than one year. There also are several forms of community-based corrections, including probation, parole, and halfway houses. Offenders in community corrections often are required to adhere to strict conditions and rules, and failure to comply with these requirements may lead to incarceration or re-incarceration.
Prisons are overseen by the federal government and states, while jails typically are governed by the local city or county. The federal correctional system consists of prisons overseen by the Federal Bureau of Prisons, which house individuals convicted of a federal crime and generally serving a term of more than one year. State correctional systems oversee prisons housing individuals convicted of state crimes and generally serving terms of more than one year. Each state governs its own prison system through a Department of Corrections. There are over 3,200 jails nationwide housing individuals awaiting trial or serving a short sentence for a misdemeanor, with most counties (2,977 out of 3,069) operating their own jails.1
The Criminal Justice-Involved Population
About 2.3 million individuals are incarcerated in prison or jail, but millions more interact with the correctional system annually (Table 1). (See Appendix Table 1 for data by state.) About 1.5 million individuals were incarcerated in prisons as of the end of 2012. Over the course of the year, about 600,000 individuals are admitted to prison and a similar number are released.2 As of mid-year 2013, over 730,000 individuals were in jails.3 About six in ten of these individuals were not convicted and awaiting court action; the remaining four in ten were sentenced or convicted offenders awaiting sentencing.4 Given the shorter terms of jail inmates compared to prisoners, there is rapid churn among the jail population. Between July 2012 and June 2013, an estimated 11.7 million people were admitted to local jails and, on average, jails experienced a weekly turnover rate of 60%.5 The jail population is concentrated in large jails (that have an average daily population of 1,000 or more inmates), which house nearly half (48%) of all jail inmates but only account for 6% of all jail jurisdictions.6 An additional 4.8 million adults were under community supervision as of the end of 2012, and about 4.1 million adults entered and exited community supervision over the course of 2012.7 About 80% of adults under community supervision are on probation, while the remainder is on parole.
| Table 1: Overview of the Criminal Justice Involved Population | |
| Prisoners | |
| Number of Prisoners as of December 31, 2012 | 1,570,397 |
| Number of Admissions of Sentenced Prisoners during 2012 | 609,781 |
| Number of Releases of Sentenced Prisoners during 2012 | 637,411 |
| Jail Inmates | |
| Number of Inmates in Local Jails as of June 2013 | 731,208 |
| Number of Persons Admitted to Local Jails, July 2012-June 2013 | 11,700,000 |
| Weekly Turnover Rate, week ending June 30, 2013 | 60% |
| Adults Under Community Supervision | |
| Number Under Community Supervision as of December 31, 2012 | 4,781,300 |
| Number Entering Community Supervision during 2012 | 2,544,400 |
| Number Exiting Community Supervision during 2012 | 2,585,900 |
| Sources: Bureau of Justice Statistics, Prisoners in 2012, Trends in Admissions and Releases, 1991-2012, U.S. Department of Justice, December 2013; Bureau of Justice Statistics, Jail Inmates at Midyear 2013 Statistical Tables, U.S. Department of Justice, May 2014, and Bureau of Justice Statistics, Probation and Parole in the United State, 2012, U.S. Department of Justice, Revised April 22, 2014. See sources for methodology and notes. | |
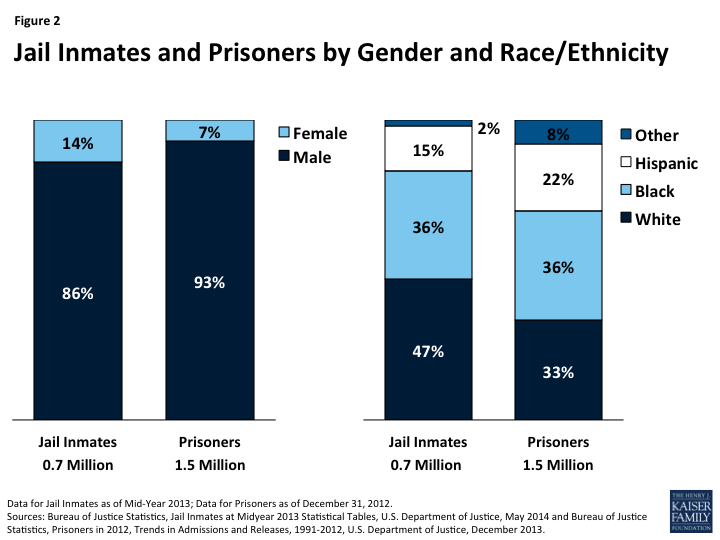
Adult males of color make up the majority of the incarcerated population. As of 2013, 99% of jail inmates were adults and 86% were male. Just over half of the jail population (53%) was people of color, including more than a third who were Black (36%) and 15% who were Hispanic (Figure 2).8 Among prisoners, more than nine in ten are male (93%) and two-thirds (66%) are people of color.9 These patterns reflect higher incarceration rates among people of color compared to Whites. Incarceration rates for Black men are over six times higher than the rate for White men and nearly two and half times higher than the rate for Hispanic men.10 American Indians also have higher rates of incarceration compared to Whites.11
People involved with the criminal justice system are generally low-income and uninsured. Overall, data on the income and insurance status of people moving into and out of the criminal justice system are limited. However, survey data from 2002 show that nearly six in ten jail inmates reported monthly income of less than $1,000 prior to their arrest.12 Data also suggest that the population is largely uninsured. For example, a survey of San Francisco county jails found that about 90% of people who enter county jails have no health insurance.13 Another survey of inmates returning to the community from Illinois jails found that more than eight in ten were uninsured after returning to the community at 16 months post-release.14
The incarcerated population has significant physical and mental health needs. Chronic disease is prevalent among the population with higher rates of tuberculosis, HIV, Hepatitis B and C, arthritis, diabetes, and sexually transmitted disease compared to the general population.15 Over half of prison and jail inmates have a mental health disorder, with local jail inmates experiencing the highest rate (64%).16 These disorders include mania, major depression, and psychotic disorders.17 Prisoners and jail inmates who have a mental health disorder are more likely than those without a disorder to have been homeless in the year prior to their incarceration, less likely to have been employed prior to their arrest, and more likely to report a history of physical or sexual abuse. Moreover, the majority of inmates with a mental health disorder also have a substance or alcohol use disorder.18
Individuals moving into and out of the criminal justice system also face a variety of social challenges. Poverty, unemployment, lower education levels, housing instability, and homelessness are all more prevalent issues among criminal justice-involved population than the general population.19 This population also generally has higher rates of learning disabilities and lower rates of literacy.20
Health Care for Incarcerated Individuals
Correctional facilities are required to provide health services to incarcerated individuals, but many inmates go without needed care. The provision of health care varies significantly across states and types of correctional facilities. Some larger prisons have infirmaries on-site, and many prisons hire independent doctors or contract with private or hospital staff to provide care, with the majority of prisons creating a hybrid system. In jails, health care is primarily provided through contracts with local health care providers, such as public hospitals or other safety-net providers, who come to the jails to provide services. As with large prisons, some large jails have on-site primary care, pharmacy, and mental health and substance abuse centers. Even though these services are available, data show that many inmates go without needed health care while incarcerated. For example, a 2009 study found that, among inmates with a persistent medical problem, approximately 14% of federal inmates, 20% of state inmates, and 68% of local jail inmates did not receive a medical examination while incarcerated.21 About two thirds of prison inmates and less than half of jail inmates who had previously been treated with a psychiatric medication had taken medication for a mental condition since incarceration.22
States have been facing rising costs in prison health care spending. As of 2011, state spending on correctional health care was about $7.7 billion, accounting for about a fifth of total prison expenditures.23 Between 2007 and 2011, correctional health care spending rose in 41 states, with a median growth rate of 13 percent.24 This growth reflects a combination of an increase in the prison population and higher per-inmate expenses due to an aging inmate population, the prevalence of physical and mental health needs, and challenges in delivering health care in prisons, such as distances from hospitals and providers.25 However, in most states, spending peaked before fiscal year 2011 and has been declining since then due, in part, to a reduction in state prison populations.26
Medicaid has historically played a very limited role in covering inmate health care costs. Prior to the ACA, Medicaid eligibility was limited to low-income people who fell into certain groups, including children, pregnant women, parents of dependent children, and elderly and disabled adults. Overall, eligibility for non-disabled, non-elderly adults was very limited, with adults without dependent children generally excluded from the program and income eligibility limits for parents remaining very low in most states.27 As such, many inmates historically could not qualify for Medicaid since they did not fit into one of the categorical eligibility categories. Even for inmates who do qualify for Medicaid, federal law prohibits Medicaid payment for most health care services provided to individuals while incarcerated under a policy known as the “inmate exclusion” (see Box 1). Given these limitations, previously, few states pursued Medicaid financing for eligible prisoners’ health care services.28
Box 1: The Medicaid Inmate Exclusion Policy
.
Federal Medicaid law prohibits the payment of federal Medicaid matching funds for the cost of any services provided to an “inmate of a public institution,” except when the individual is a “patient in a medical institution.”29
.
This policy applies to both adults in jails or prisons as well as to youth involuntarily detained in a state or local juvenile facility.This policy does not prohibit individuals from being enrolled in Medicaid while incarcerated; however, even if they are enrolled, Medicaid will not cover the cost of their care, except for care received as an inpatient in a hospital or other medical institution.
.
Because individuals may remain enrolled, states can suspend, rather than terminate, Medicaid coverage for inmates to accommodate the inmate exclusion. However, suspension and termination policies vary across states.
The ACA and the Criminal Justice-Involved Population
The ACA offers new opportunities to increase health coverage among individuals transitioning back into the community from prisons and jails. The ACA established new coverage options by expanding Medicaid eligibility to nearly all adults with incomes at or below 138% FPL ($16,105 for an individual in 2014). The federal government will cover 100% of the cost of coverage for individuals made newly eligible as a result of this expansion, phasing down to a 90% federal match as of 2020. The ACA also created new Health Insurance Marketplaces with premium tax credits available for moderate income individuals. In addition to these coverage expansions, the ACA also requires all states to implement streamlined, coordinated enrollment processes to connect eligible individuals to health coverage.
The ACA coverage expansions provide new coverage options for many individuals who interact with the criminal justice system. Although as enacted in the ACA, the Medicaid expansion would occur in all states, the Supreme Court ruling on the ACA effectively made the expansion a state option. As of August 2014, 28 states are implementing the expansion.30 In states expanding Medicaid to low-income adults, many individuals who interact with the criminal justice system are newly eligible for the program. Moreover, in all states, some individuals being released from prison and jail may qualify for coverage under the new Marketplaces established by the ACA (see Box 2). However, in states not implementing the Medicaid expansion, many poor uninsured adults did not gain a new coverage option and will likely remain uninsured. While the coverage expansions increase coverage options for individuals transitioning through the criminal justice system, targeted outreach and enrollment efforts will be key for translating these new options into increased coverage, particularly since the population faces a broad range of enrollment barriers such as lack of knowledge about coverage options and lower literacy and education levels.31
Box 2: Medicaid and Marketplace Enrollment Policies for Incarcerated Individuals
.
Medicaid. Individuals incarcerated in jail or prison may enroll in Medicaid while incarcerated. However, Medicaid will not pay for most medical care for individuals while they are housed in jail or prison due to the federal inmate exclusion policy.
.
Marketplace coverage. Individuals may not purchase coverage through the Marketplace while serving a term in prison or jail. (This bar on purchasing coverage does not extend to individuals in jail or prison who are pending disposition of charges—i.e., being held but not yet convicted of a crime.) Individuals are provided a 60-day special enrollment period that begins upon discharge from jail or prison. During this time, they may enroll in coverage even if it is outside the Marketplace open enrollment period. However, because this special enrollment period does not begin until the time of release, they will likely experience a gap in coverage between the time of discharge and completion of enrollment in coverage. After the 60-day special enrollment period, individuals are not eligible to purchase coverage through the Marketplace until the next regular open enrollment period or unless they qualify for a different special enrollment period.
.
Source: “Health coverage for incarcerated people,” at https://www.healthcare.gov/incarceration/
Correctional facilities can play a key role in connecting eligible individuals to coverage and care to facilitate their reintegration back into the community. Correctional facilities can help connect eligible individuals to coverage by providing outreach and education about coverage options as well as direct enrollment assistance either through staff or by bringing in external enrollment assisters. Providing this assistance within jails may be challenging since there is often limited time to connect individuals with resources or support community re-entry given the short-terms of jail inmates. However, several states and localities have already launched initiatives to enroll individuals into coverage and facilitate connections to community providers as individuals transition back into the community (see Box 3).
Increased coverage among the criminal justice-involved population may lead to improved access to care and broader benefits, including reduced recidivism rates. As noted, individuals transitioning into and out of prisons and jails have significant physical and mental health needs. Upon release from prison and jail, individuals are often uninsured, making it difficult to access stable sources of care in the community to address these needs. Expanding health insurance to these individuals will likely facilitate their ability to access needed care and manage their ongoing conditions. Improved connections to services and better management of health conditions may also contribute to reduced rates of recidivism, particularly among individuals with mental health and substance abuse disorders. For example, in Michigan, rates of recidivism fell following implementation of an initiative that links newly released prisoners to a medical home in the community, helps them access needed medications and primary and specialty care, and assists them in obtaining their medical records upon release.32 In addition, studies in Florida and Washington found that people with severe mental illness who were enrolled in Medicaid at jail release were more likely to access community mental health and substance abuse services than those without Medicaid, and that 12 months after release, Medicaid enrollees had 16% fewer detentions and stayed out of jail longer than those who either were not enrolled or had been enrolled for a shorter time.33
Box 3: Connecting Individuals to Coverage and Care to Support Community Re-Entry
.
Application Assistance in Cook County Jail. Cook County Health and Hospital System (CCHHS) partnered with Cook County Sheriff’s Office (CCSO) and a non-profit organization, Treatment Alternatives for Safe Communities (TASC), to screen detainees entering Cook County Jail for eligibility for CountyCare, the county’s Medicaid expansion program. By using information gathered at intake, TASC employees are able to validate identity and meet application requirements onsite. As of April 1, 2014, approximately 3,845 people received coverage after starting an application in jail and there is a 94% approval rate for applications submitted from Cook County Jail.34
.
Connections Correctional Health Care Services in Delaware. Connections is a community based not-for-profit organization that provides behavioral health care in all of the Delaware Department of Corrections facilities. Through a partnership with Community Oriented Correctional Health Services (COCHS), Connections is maximizing continuity of care by connecting individuals in correctional facilities with providers in the community. The system brings providers into the facilities that the inmate can also connect with for care after being released. Approximately 25,000 inmates cycle through Delaware’s correctional facilities annually and, on average, Connections works with about 7,000 prisoners per day.35
Expanding health coverage among the criminal justice-involved population may contribute to offsetting savings for states. Although the Medicaid inmate exclusion policy limits Medicaid payments for most health care services provided to individuals while incarcerated in prison or jail, Medicaid reimbursement is available for care provided to eligible individuals admitted to an inpatient facility, such as a hospital, nursing home, or psychiatric center. Prior to the ACA, only a few states had pursued Medicaid reimbursement for these services given the limited share of the incarcerated population that could qualify for Medicaid. However, those that did pursue federal matching dollars for inmate inpatient services demonstrated state savings.36 The Medicaid expansion offers greater potential savings to states from reimbursement for inpatient services provided to incarcerated individuals, since a larger share of the incarcerated population may qualify for Medicaid and because the federal government is providing states an enhanced federal matching rate for newly eligible adults. Several states have projected substantial state savings from obtaining Medicaid reimbursement for inpatient care provided to prisoners.37 Increased coverage among the formerly incarcerated population as they return to the community may also contribute to other state and local savings through reductions in uncompensated care and savings in other indigent care programs.
Conclusion
Individuals moving into and out of the criminal justice population are a low-income population with significant physical and mental health needs. Historically, this population has had high uninsured rates and very limited access to Medicaid coverage given the program’s limited eligibility for adults prior to the ACA. The ACA’s Medicaid expansion and Marketplaces, coupled with targeted outreach and enrollment efforts, provide opportunities to increase coverage among this population that should help to improve their ability to access needed care and contribute to greater stability in their lives and reduced rates of recidivism. States expanding Medicaid may also reduce spending for their incarcerated population and achieve other state and local savings stemming from gains in coverage through Medicaid and the Marketplaces among formerly incarcerated individuals who are returning to the community.