2017 Employer Health Benefits Survey
Section 7: Employee Cost Sharing
In addition to any required premium contributions, most covered workers face cost sharing for the medical services they use. Cost sharing for medical services can take a variety of forms, including deductibles (an amount that must be paid before most services are covered by the plan), copayments (fixed dollar amounts), and coinsurance (a percentage of the charge for services). The type and level of cost sharing often vary by the type of plan in which the worker is enrolled. Cost sharing may also vary by the type of service, such as office visits, hospitalizations, or prescription drugs.
The cost-sharing amounts reported here are for covered workers using services provided in-network by participating providers. Plan enrollees receiving services from providers that do not participate in plan networks often face higher cost sharing and may be responsible for charges that exceed plan allowable amounts. The framework of this survey does not allow us to capture all of the complex cost-sharing requirements in modern plans, particularly for ancillary services (such as durable medical equipment or physical therapy) or cost-sharing arrangements that vary across different settings (such as tiered networks). Therefore, we do not collect information on all plan provisions and limits that affect enrollee out-of-pocket liability.
GENERAL ANNUAL DEDUCTIBLES FOR WORKERS IN PLANS WITH DEDUCTIBLES
- A general annual deductible is an amount that must be paid by enrollees before most services are covered by their health plan. Non-grandfathered health plans are required to cover some services such as preventive care without cost sharing. Some plans require enrollees to meet a service-specific deductible, such as on prescription drugs or hospital admissions, in lieu of or in addition to a general annual deductible.
- Eighty-one percent of covered workers are enrolled in a plan with a general annual deductible for single coverage, similar to 83% in 2016, but an increase from 72% in 2012 [Figure 7.2].
- The percentage of covered workers enrolled in a plan with a general annual deductible for single coverage is similar for small firms (3-199 workers) and large firms (200 or more workers) (77% and 83%) [Figure 7.2].
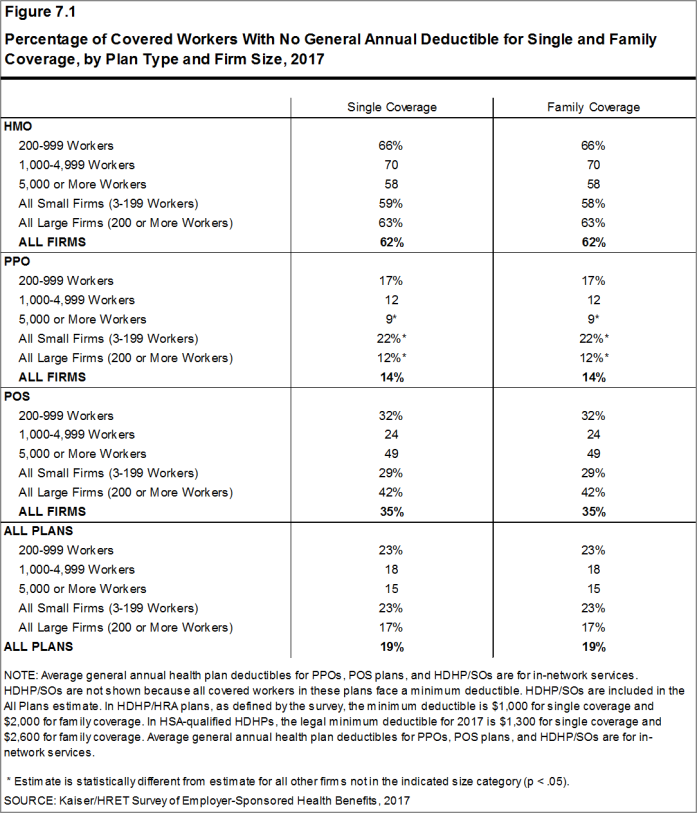
- The likelihood of having a deductible varies by plan type [Figure 7.1]. Covered workers in HMOs are less likely to have a general annual deductible for single coverage than workers in other plan types. Sixty-two percent of workers in HMOs do not have a general annual deductible for single coverage, compared to 35% of workers in POS plans and 14% of workers in PPOs.
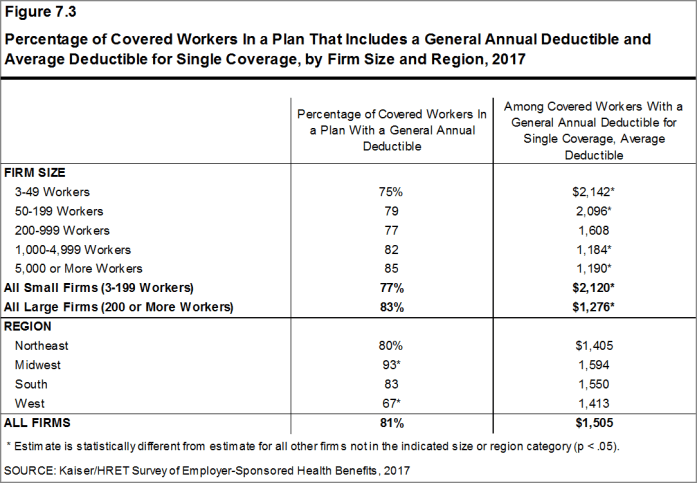
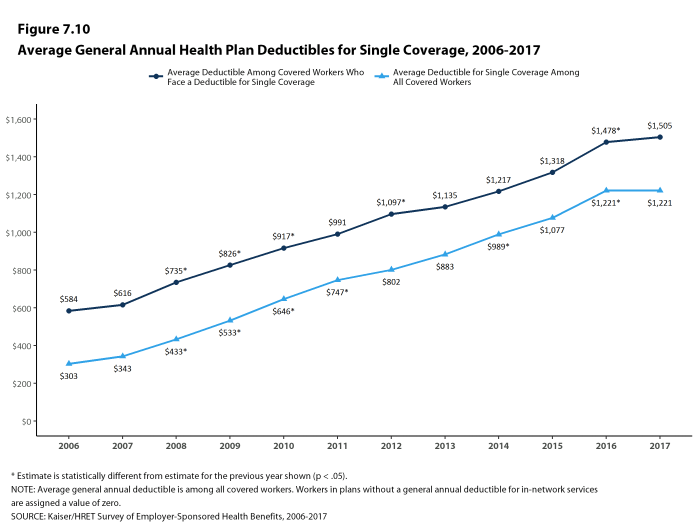
- For covered workers in a plan with a general annual deductible, the average annual deductible for single coverage is $1,505, similar to the average deductible ($1,478) last year [Figures 7.3 and 7.10].
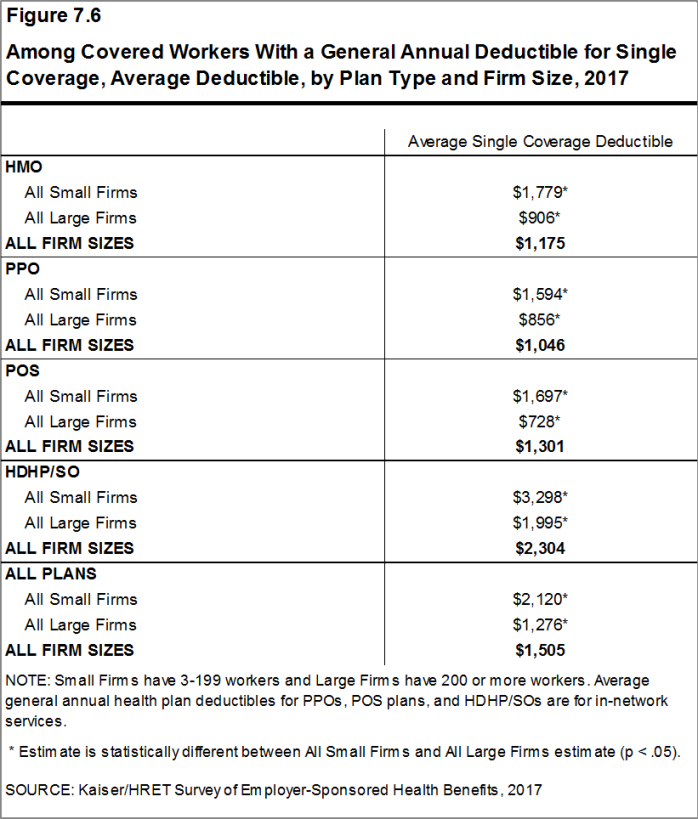
- For covered workers in plans with a general annual deductible, the average deductibles for single coverage are $1,175 in HMOs, $1,046 in PPOs, $1,301 in POS plans, and $2,304 in HDHP/SOs [Figure 7.6].
- The average deductibles for single coverage are higher across plan types for covered workers in small firms than for covered workers in large firms. For covered workers in PPOs with a general annual deductible, for example, the average deductible amount for single coverage in small firms is much higher than the average deductible amount in large firms ($1,594 vs. $856) [Figure 7.6]. Overall, for covered workers in plans with a general annual deductible, the average deductible amount for single coverage in small firms is higher than the average deductible amount in large firms ($2,120 vs. $1,276) [Figure 7.3].
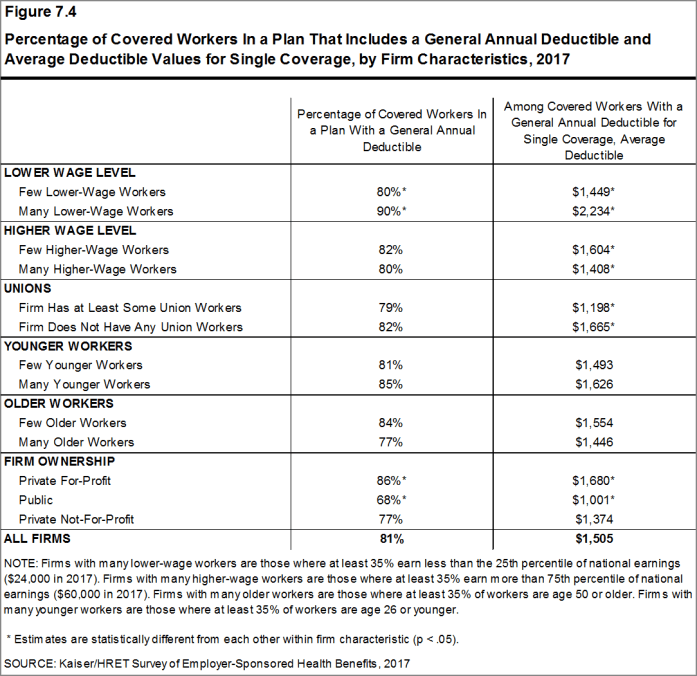
- Among covered workers in plans with a general annual deductible, the average deductible for workers in firms with a relatively large share of lower-wage workers (where at least 35% of workers earn $24,000 a year or less) is higher than the average deductible for covered workers in firms with a smaller share of lower-wage workers ($2,234 vs. $1,449) [Figure 7.4].
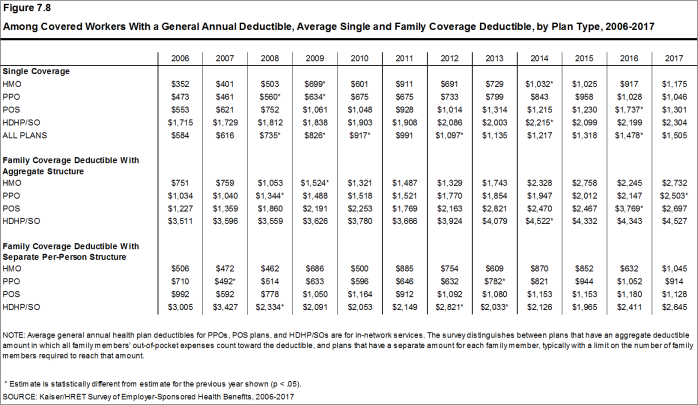
- The average general annual deductible for single coverage for covered workers in plans with a deductible has increased 37% over the last five years, from $1,097 in 2012 to $1,505 in 2017 [Figure 7.8].
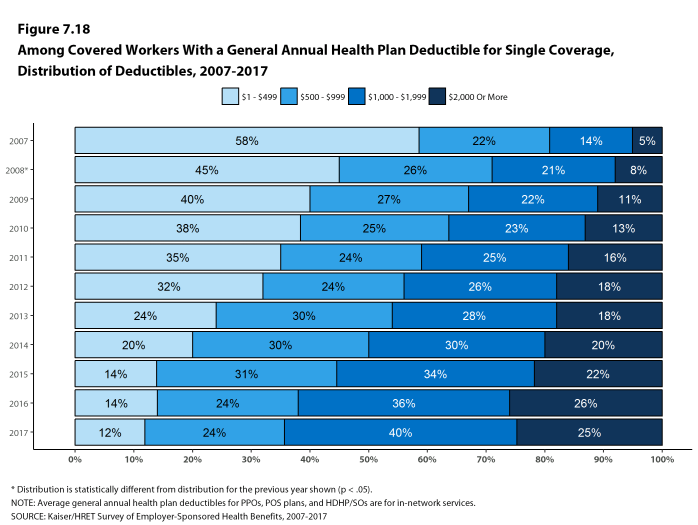
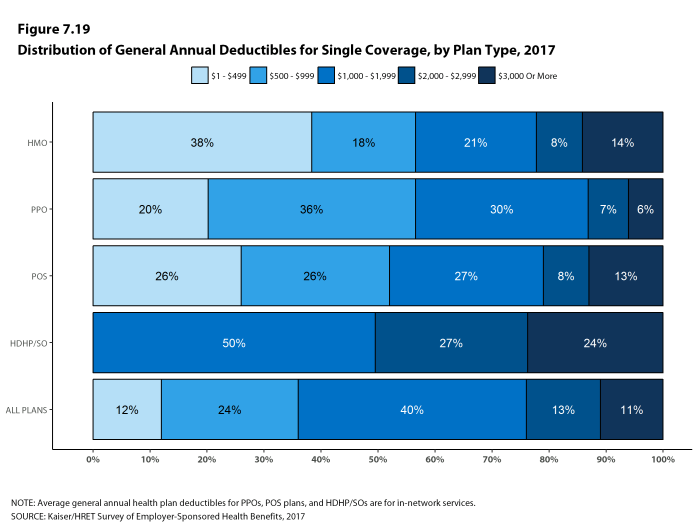
- There is considerable variation in the dollar values of general annual deductibles for covered workers at different firms. For example, 20% of covered workers enrolled in a PPO plan with a general annual deductible for single coverage have a deductible of less than $500, while 13% have a deductible of $2,000 or more [Figure 7.19].
Figure 7.1: Percentage of Covered Workers With No General Annual Deductible for Single and Family Coverage, by Plan Type and Firm Size, 2017
Figure 7.2: Percentage of Covered Workers In a Plan That Includes a General Annual Deductible for Single Coverage, by Plan Type, 2006-2017
Figure 7.3: Percentage of Covered Workers In a Plan That Includes a General Annual Deductible and Average Deductible for Single Coverage, by Firm Size and Region, 2017
Figure 7.4: Percentage of Covered Workers In a Plan That Includes a General Annual Deductible and Average Deductible Values for Single Coverage, by Firm Characteristics, 2017
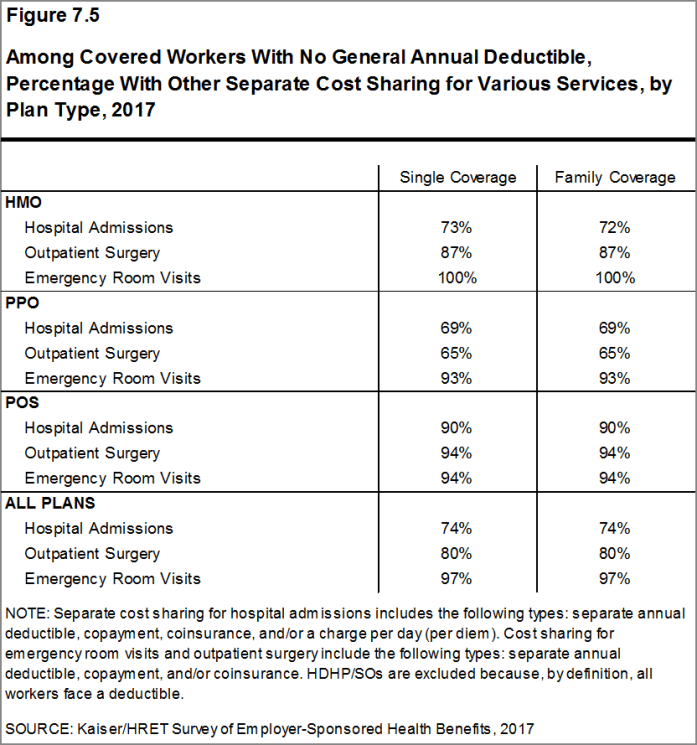
Figure 7.5: Among Covered Workers With No General Annual Deductible, Percentage With Other Separate Cost Sharing for Various Services, by Plan Type, 2017
Figure 7.6: Among Covered Workers With a General Annual Deductible for Single Coverage, Average Deductible, by Plan Type and Firm Size, 2017
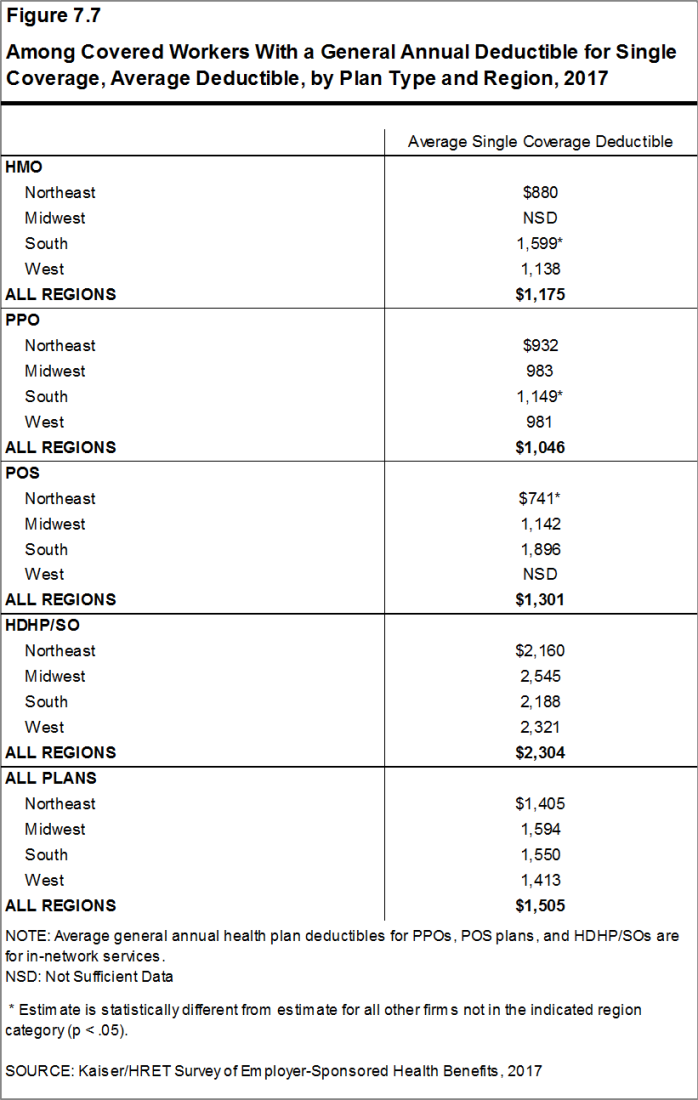
Figure 7.7: Among Covered Workers With a General Annual Deductible for Single Coverage, Average Deductible, by Plan Type and Region, 2017
Figure 7.8: Among Covered Workers With a General Annual Deductible, Average Single and Family Coverage Deductible, by Plan Type, 2006-2017
GENERAL ANNUAL DEDUCTIBLES AMONG ALL COVERED WORKERS
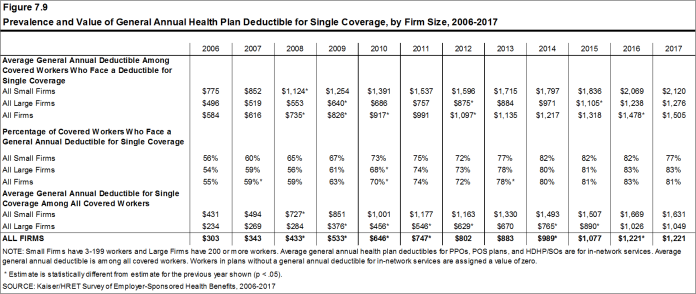
- As discussed above, the share of covered workers in plans with a general annual deductible has increased significantly over time: from 59% in 2007, to 72% in 2012, to 81% in 2017 [Figure 7.2], as have the average deductible amounts for covered workers in plans with deductibles: from $616 in 2007, to $1,097 in 2012, to $1,505 in 2017 [Figure 7.10]. Neither trend by itself captures the full impact of changes in deductibles on covered workers. We can look at the average impact of both trends together on covered workers by assigning a zero deductible value to covered workers in plans with no deductible and looking at how the resulting averages change over time. These average deductible amounts are lower in any given year but the changes over time reflect both the higher deductibles in plans with deductibles and the fact that more workers face them.
- Using this approach, the average general annual deductible for single coverage for all covered workers in 2017 is $1,221 [Figures 7.9 and 7.10].
- The 2017 value is 52% higher than the average general annual deductible of $802 in 2012 and 255% higher than the average general annual deductible of $343 in 2007 [Figures 7.9 and 7.10].
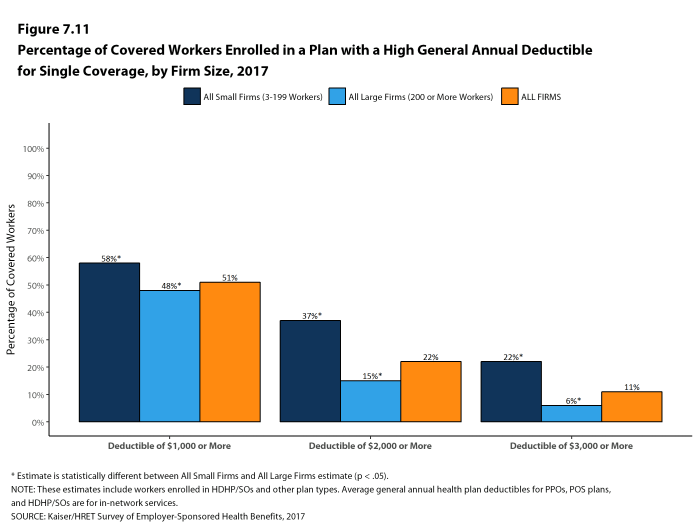
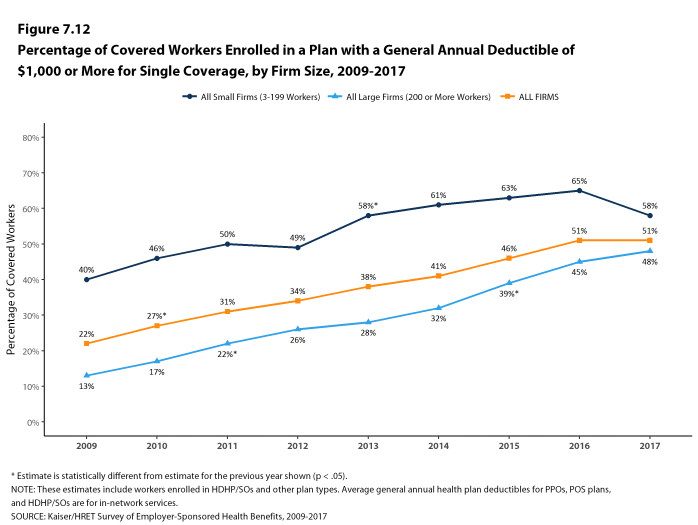
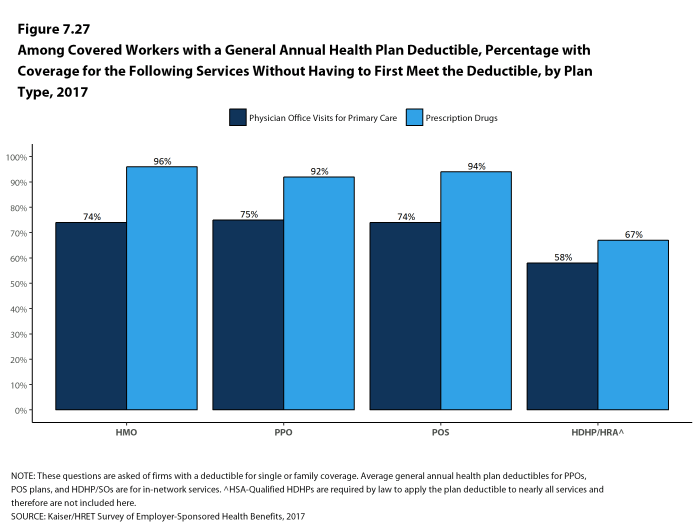
- Another way to look at deductibles is the percentage of all covered workers who are in a plan with a deductible that exceeds certain thresholds. Fifty-one percent of covered workers are in plans with a general annual deductible of $1,000 or more for single coverage, the same percentage as last year [Figure 7.12].
- Over the last five years, the percentage of covered workers with a general annual deductible of $1,000 or more for single coverage has grown substantially, increasing from 34% to 51% [Figure 7.12].
- Workers in small firms are more likely to have a general annual deductible of $1,000 or more for single coverage than workers in large firms (58% vs. 48%) [Figure 7.11].
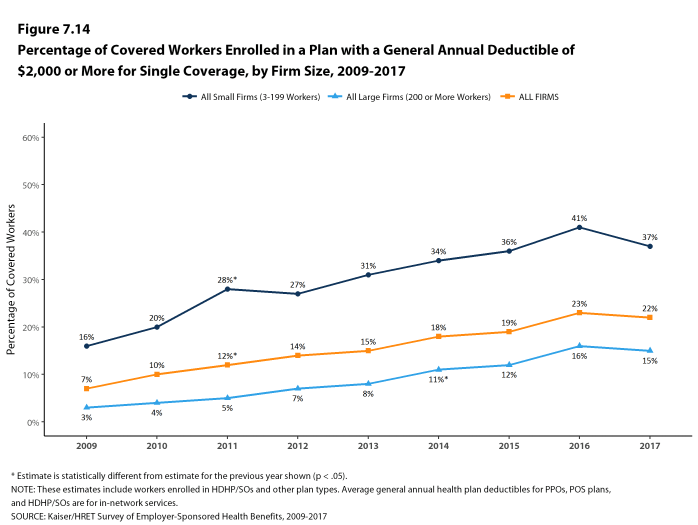
- Twenty-two percent of covered workers are enrolled in a plan with a deductible of $2,000 or more, similar to the percentage last year (23%) [Figure 7.14]. Thirty-seven percent of covered workers in small firms have a general annual deductible of $2,000 or more, as compared to 15% in large firms [Figure 7.14].
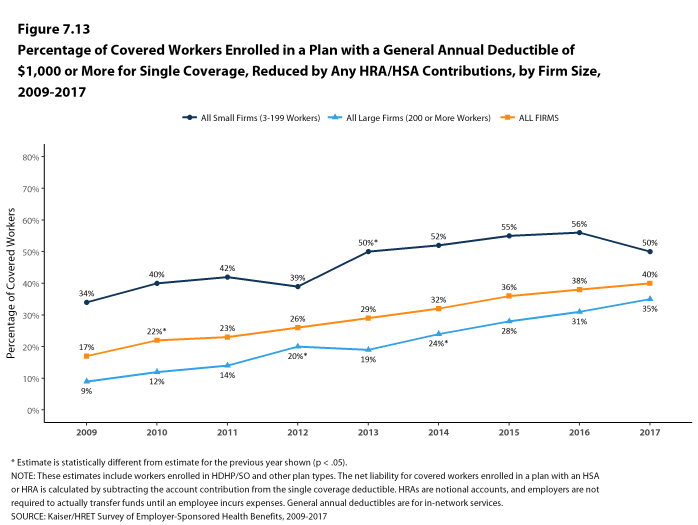
- One of the reasons for the growth in deductible amounts has been the growth in enrollment in HDHP/SOs, which have higher deductibles than other plans. While growing deductibles in other plan types generally increases enrollee out-of-pocket liability, the shift in enrollment to HDHP/SOs does not necessarily do so because most HDHP/SO enrollees receive an account contribution from their employers, which in essence reduces the high cost sharing in these plans.
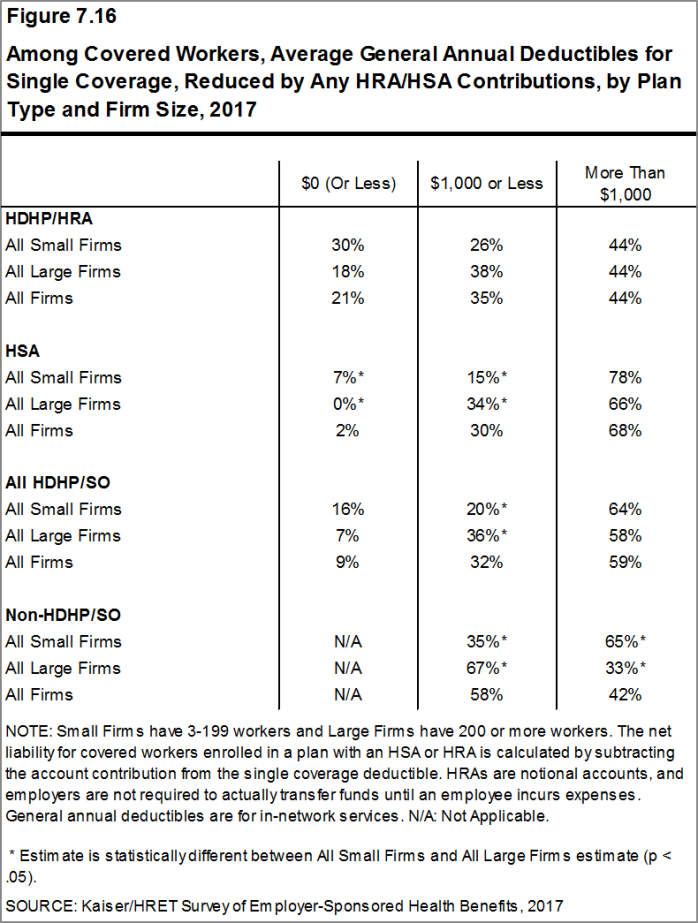
- Twenty-one percent of covered workers in an HDHP with an HRA and 2% of covered workers in an HSA-qualified HDHP receive an account contribution for single coverage at least equal to their deductible, while another 35% of covered workers in an HDHP with an HRA and 30% of covered workers in an HSA-qualified HDHP receive account contributions that, if applied to their deductible, would reduce the deductible to $1,000 or less [Figure 7.16].
- If we reduce the deductibles that workers face by employer account contributions, the percentage of covered workers with a deductible liability of $1,000 or more would be reduced from 51% to 40% [Figures 7.12 and 7.13].
Figure 7.11: Percentage of Covered Workers Enrolled In a Plan With a High General Annual Deductible for Single Coverage, by Firm Size, 2017
Figure 7.12: Percentage of Covered Workers Enrolled In a Plan With a General Annual Deductible of $1,000 or More for Single Coverage, by Firm Size, 2009-2017
Figure 7.13: Percentage of Covered Workers Enrolled In a Plan With a General Annual Deductible of $1,000 or More for Single Coverage, Reduced by Any HRA/HSA Contributions,
Figure 7.14: Percentage of Covered Workers Enrolled In a Plan With a General Annual Deductible of $2,000 or More for Single Coverage, by Firm Size, 2009-2017
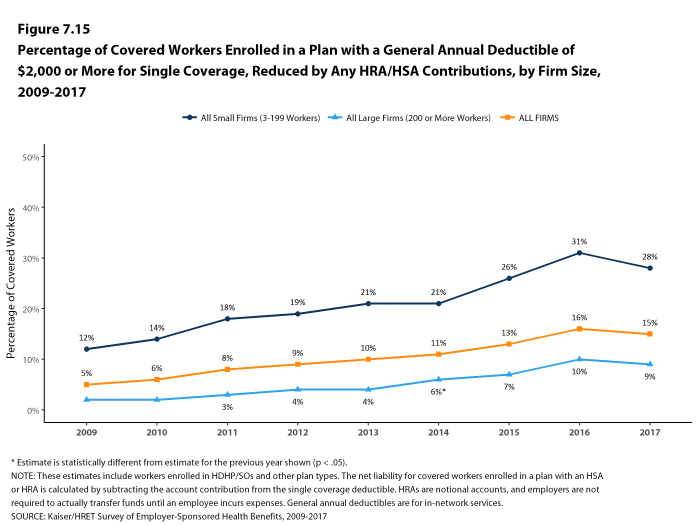
Figure 7.15: Percentage of Covered Workers Enrolled In a Plan With a General Annual Deductible of $2,000 or More for Single Coverage, Reduced by Any HRA/HSA Contributions, by Firm Size, 2009-2017
Figure 7.16: Among Covered Workers, Average General Annual Deductibles for Single Coverage, Reduced by Any HRA/HSA Contributions, by Plan Type and Firm Size, 2017
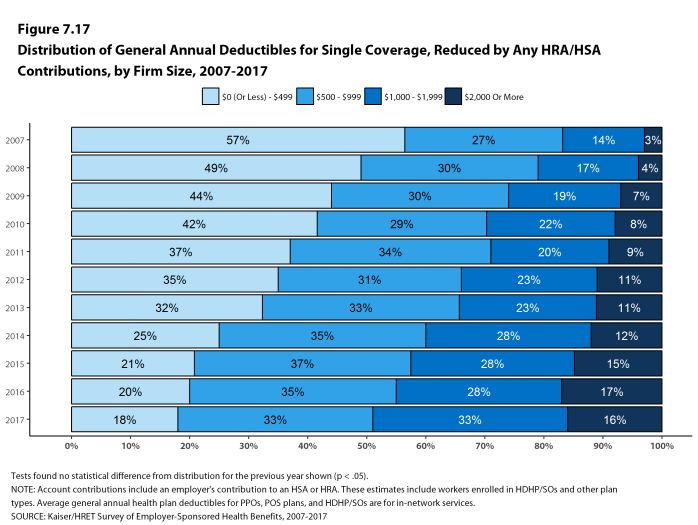
Figure 7.17: Distribution of General Annual Deductibles for Single Coverage, Reduced by Any HRA/HSA Contributions, by Firm Size, 2007-2017
Figure 7.18: Among Covered Workers With a General Annual Health Plan Deductible for Single Coverage, Distribution of Deductibles, 2007-2017
GENERAL ANNUAL DEDUCTIBLES FOR WORKERS ENROLLED IN FAMILY COVERGE
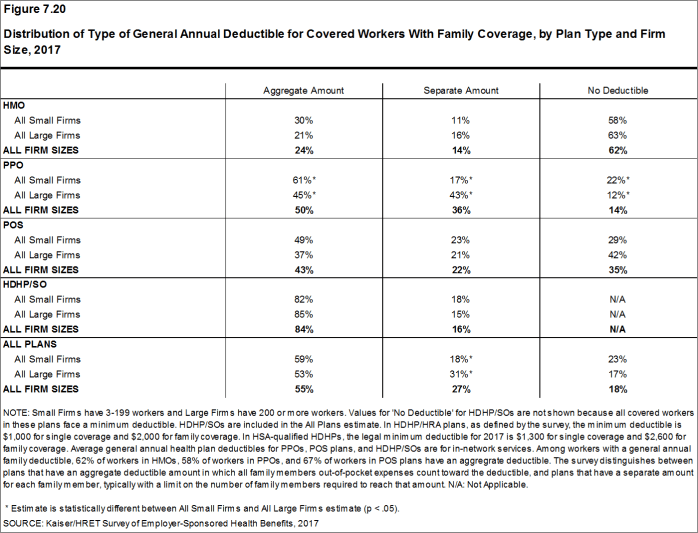
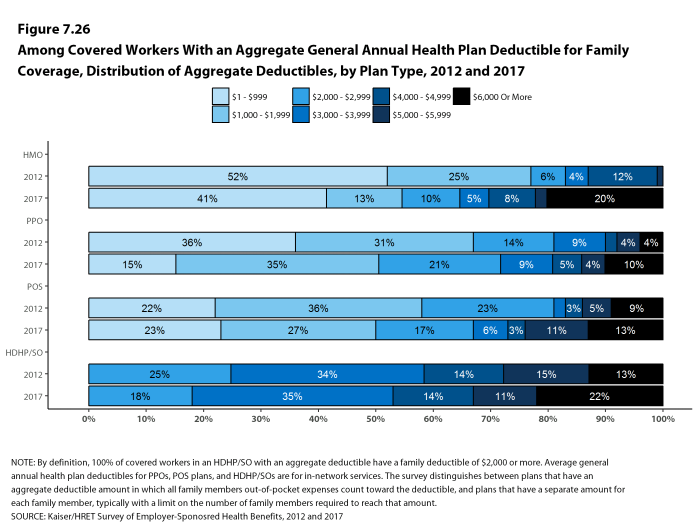
- For family coverage, the majority of covered workers with general annual deductibles have an aggregate deductible, which means that all family members’ out-of-pocket expenses count toward meeting the deductible amount. Among covered workers in a plan with family coverage, the percentages of covered workers with an average aggregate general annual deductible are 24% for workers in HMOs, 50% for workers in PPOs, and 43% for workers in POS plans [Figure 7.20].
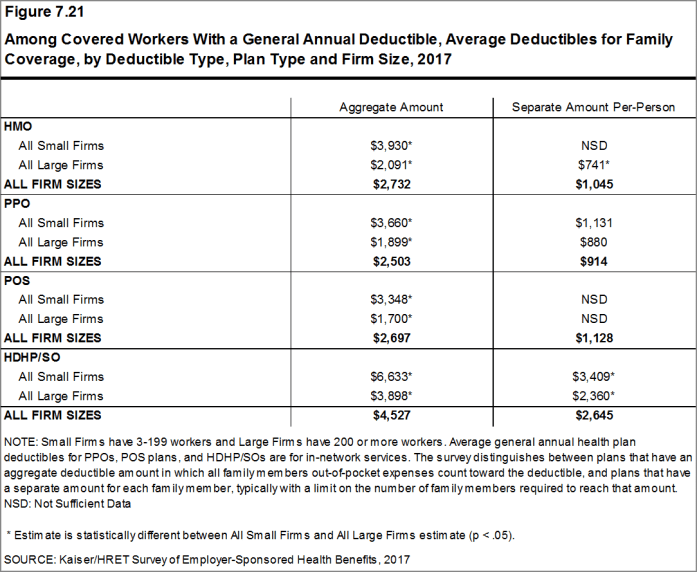
- The average deductible amounts for covered workers with an aggregate deductible for family coverage are $2,732 for HMOs, $2,503 for PPOs, $2,697 for POS plans, and $4,527 for HDHP/SOs [Figure 7.21]. Deductible amounts for aggregate family deductibles are similar to last year for plan types other than PPOs.
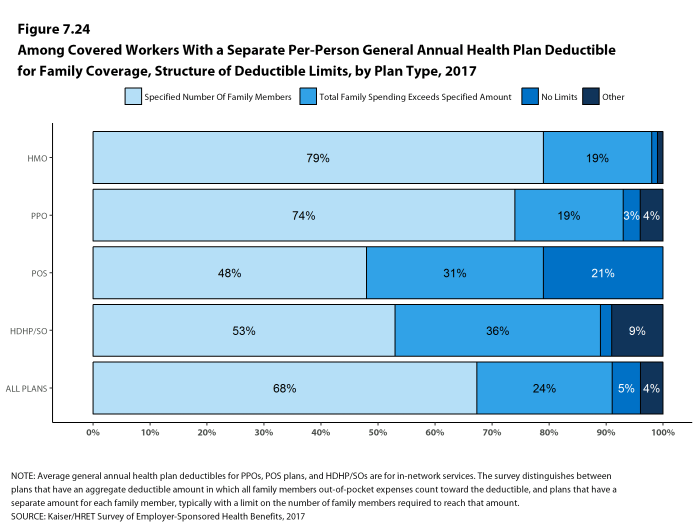
- The other type of family deductible, a separate per-person deductible, requires each family member to meet a separate per-person deductible amount before the plan covers expenses for that member. About two-thirds of covered workers in plans with separate per-person family deductibles (68%) consider the deductible met for all family members if a prescribed number of family members each reaches his or her separate deductible amounts [Figure 7.24].24 Plans may also require each family member to meet a separate per-person deductible until the family’s combined spending reaches a specified dollar amount.
- For covered workers in health plans that have separate per-person general annual deductible amounts for family coverage, the average deductibles are $1,045 for HMOs, $914 for PPOs, $1,128 for POS plans, and $2,645 for HDHP/SOs [Figure 7.21].
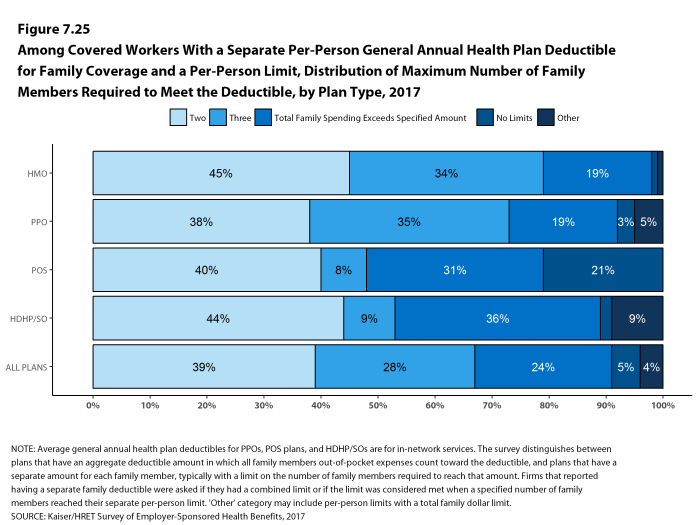
- Most covered workers in plans with a separate per-person general annual deductible for family coverage have a limit to the number of family members required to meet the separate deductible amounts [Figure 7.24]. Among those covered workers in plans with a limit on the number of family members, the most frequent number of family members required to meet the separate deductible amounts is two (39%) [Figure 7.25].
- For covered workers in plans with an aggregate deductible for family coverage, the average annual family deductibles in small firms are higher than the average annual family deductibles in large firms across plan types [Figure 7.21].
Figure 7.20: Distribution of Type of General Annual Deductible for Covered Workers With Family Coverage, by Plan Type and Firm Size, 2017
Figure 7.21: Among Covered Workers With a General Annual Deductible, Average Deductibles for Family Coverage, by Deductible Type, Plan Type and Firm Size, 2017
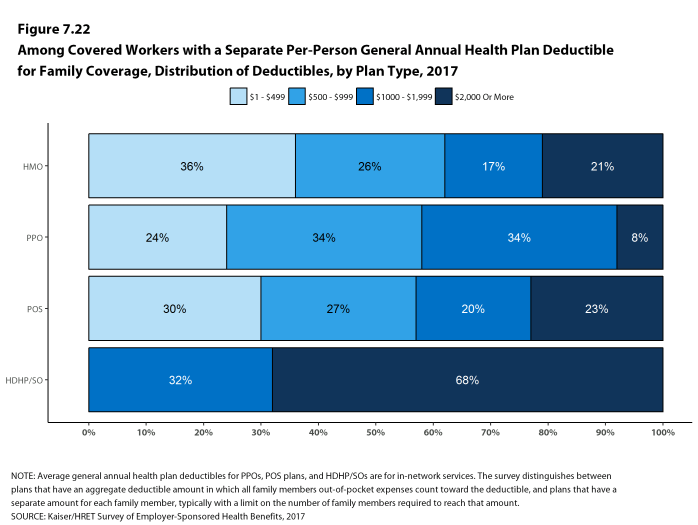
Figure 7.22: Among Covered Workers with a Separate Per-Person General Annual Health Plan Deductible for Family Coverage, Distribution of Deductibles, by Plan Type, 2017
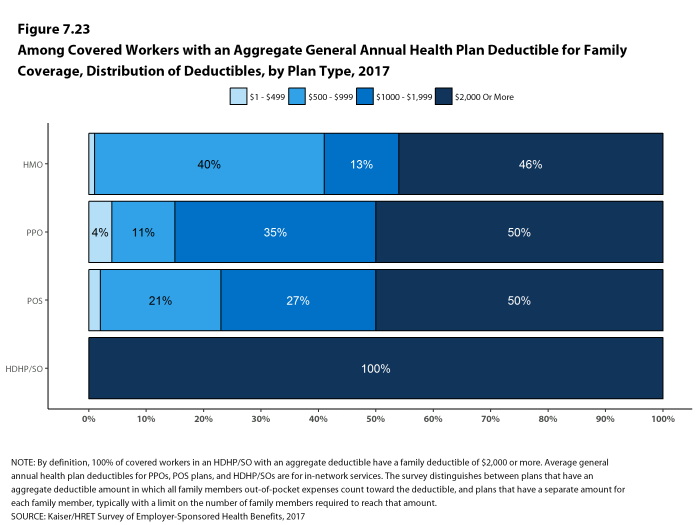
Figure 7.23: Among Covered Workers With an Aggregate General Annual Health Plan Deductible for Family Coverage, Distribution of Deductibles, by Plan Type, 2017
Figure 7.24: Among Covered Workers With a Separate Per-Person General Annual Health Plan Deductible for Family Coverage, Structure of Deductible Limits, by Plan Type, 2017
Figure 7.25: Among Covered Workers With a Separate Per-Person General Annual Health Plan Deductible for Family Coverage and a Per-Person Limit, Distribution of Maximum Number of Family Members Required to Meet the Deductible, by Plan Type, 2017
CHARACTERISTICS OF GENERAL ANNUAL DEDUCTIBLES
- The majority of covered workers with a general annual deductible are in plans where the deductible does not have to be met before certain services, such as physician office visits or prescription drugs, are covered.
- Large majorities of covered workers (74% in HMOs, 75% in PPOs, and 74% in POS plans) with general annual deductibles are enrolled in plans where the deductible does not have to be met before physician office visits for primary care are covered [Figure 7.27].
- Similarly, among workers with a general annual deductible, large shares of covered workers in HMOs (96%), PPOs (92%), and POS plans (94%) are enrolled in plans where the general annual deductible does not have to be met before prescription drugs are covered [Figure 7.27].
HOSPITAL ADMISSIONS, OUTPATIENT SURGERY AND EMERGENCY ROOM VISITS
- Whether or not a worker has a general annual deductible, most workers face additional types of cost sharing (such as a copayment, coinsurance, or a per diem charge) when admitted to a hospital or having outpatient surgery. The distribution of workers with cost sharing for hospital admissions, outpatient surgery and emergency room visits does not equal 100% as workers may face a combination of types of cost sharing. In some cases, these cost-sharing arrangements are very complicated; for example workers visiting an emergency room may have some forms of cost-sharing waived if they are admitted to the hospital but still face other cost-sharing. In addition, the average copayment and coinsurance rates include workers who may have a combination of these types of cost sharing.
- Beginning this year, to reduce burden on respondents, we revised the survey to ask respondents about cost sharing for inpatient admissions, outpatient surgery and emergency room visits only in their largest health plan type; previously, we asked for this information for the largest plan for each of the plan types that they offered. After reviewing the responses and comparing them to prior years where we asked about each plan type, we find that the information we are receiving is quite similar to responses from previous years. For this reason, we will continue to report our results for these questions weighted by the number of covered workers in the responding firms. There is a more detailed discussion in the survey design and methods section on this topic.
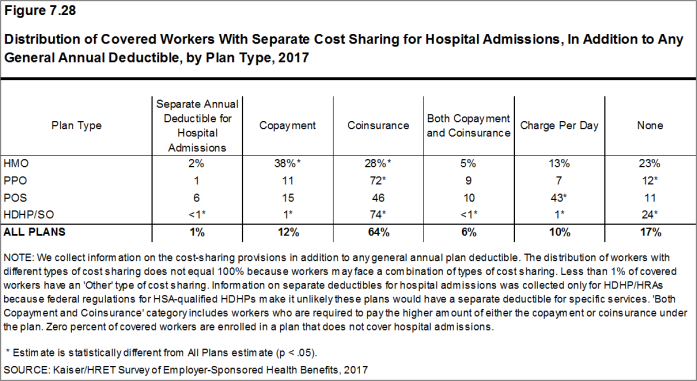
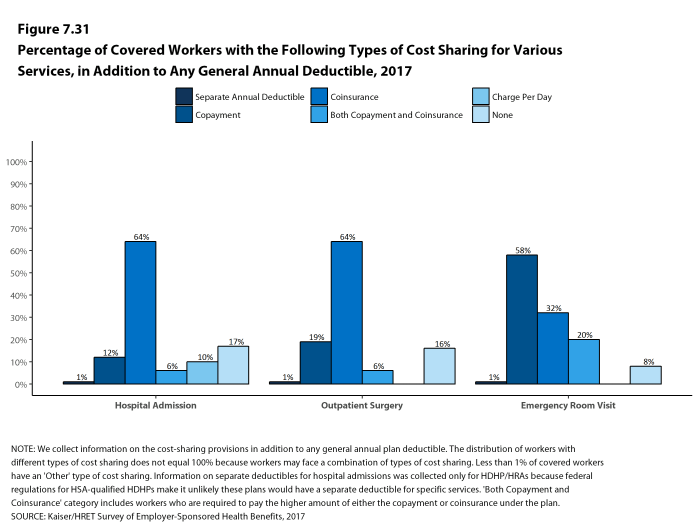
- For hospital admissions, 64% of covered workers have coinsurance and 12% have copayments. Lower percentages of workers have per day (per diem) payments (10%), a separate hospital deductible (1%), or both a copayment and coinsurance (6%), while 17% have no additional cost sharing for hospital admissions after any general annual deductible has been met [Figure 7.28].
- For covered workers in HMO plans, copayments are more common (38%) and coinsurance (28%) is less common than the average for all covered workers [Figure 7.28].
- HDHP/SOs, on average, have a different cost-sharing structure than other plan types for hospital admissions. Only 1% of covered workers in HDHP/SOs have a copayment for hospital admissions, lower than the average for all covered workers [Figure 7.28].
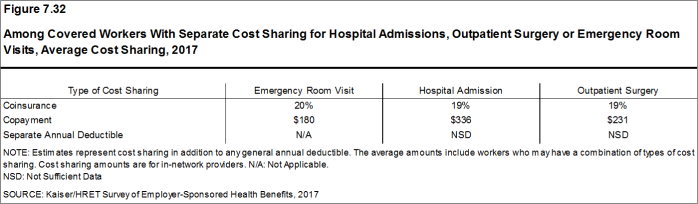
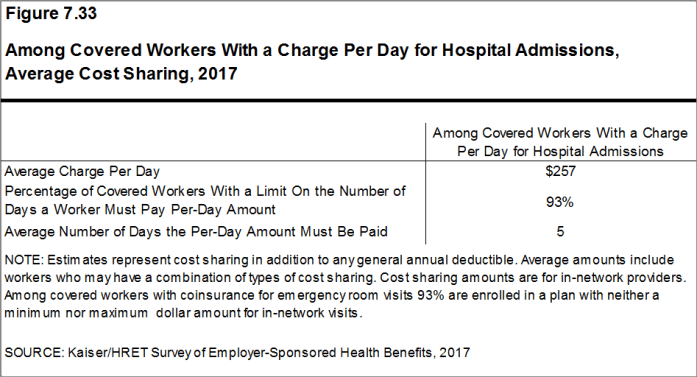
- The average coinsurance rate for a hospital admission is 19%, the average copayment is $336 per hospital admission, and the average per diem charge is $257 [Figure 7.32]. Ninety-three percent of workers enrolled in a plan with a per diem for hospital admissions have a limit on the number of days a worker must pay the amount [Figure 7.33].
- The cost-sharing provisions for outpatient surgery are similar to those for hospital admissions, as most workers have coinsurance or copayments. In 2017, 19% of covered workers have a copayment and 64% have coinsurance for outpatient surgery. In addition, 6% have both a copayment and coinsurance, while 16% have no additional cost sharing after any general annual deductible has been met [Figure 7.29].
- For covered workers with cost sharing for outpatient surgery, the average coinsurance rate is 19% and the average copayment is $231 [Figure 7.32].
- The large majority of covered workers have cost sharing when they visit an emergency room. In 2017, 58% percent of covered workers have a copayment for emergency room visits and 32% have a coinsurance [Figure 7.30].
- For covered workers with cost sharing for an emergency room visit, the average coinsurance rate is 20% and the average copayment is $180 [Figure 7.32].
- Among covered workers in HDHP/SO plans, 21% have no cost sharing for an emergency room visit after any general annual deductible has been met, compared to 8% of covered workers in all plans [Figure 7.30].
Figure 7.28: Distribution of Covered Workers With Separate Cost Sharing for Hospital Admissions, In Addition to Any General Annual Deductible, by Plan Type, 2017
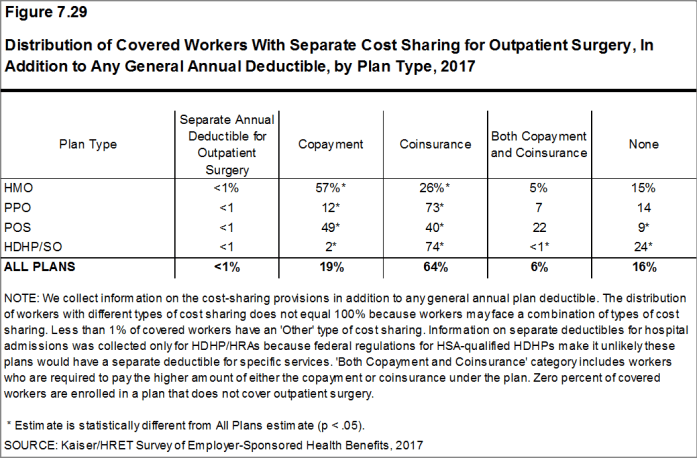
Figure 7.29: Distribution of Covered Workers with Separate Cost Sharing for Outpatient Surgery, in Addition to Any General Annual Deductible, by Plan Type, 2017
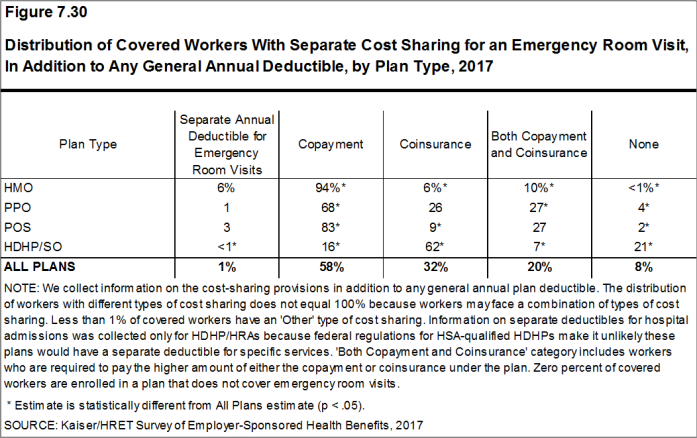
Figure 7.30: Distribution of Covered Workers with Separate Cost Sharing for an Emergency Room Visit, in Addition to Any General Annual Deductible, by Plan Type, 2017
Figure 7.31: Percentage of Covered Workers With the Following Types of Cost Sharing for Various Services, In Addition to Any General Annual Deductible, 2017
Figure 7.32: Among Covered Workers With Separate Cost Sharing for Hospital Admissions, Outpatient Surgery or Emergency Room Visits, Average Cost Sharing, 2017
Figure 7.33: Among Covered Workers With a Charge Per Day for Hospital Admissions, Average Cost Sharing, 2017
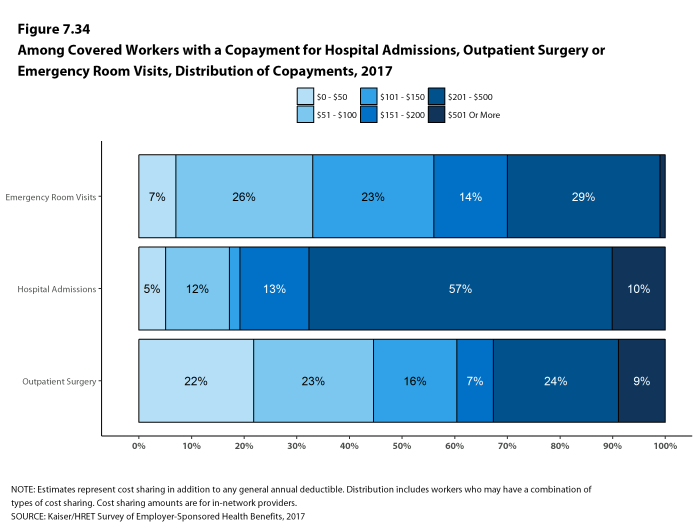
Figure 7.34: Among Covered Workers With a Copayment for Hospital Admissions, Outpatient Surgery or Emergency Room Visits, Distribution of Copayments, 2017
COST SHARING FOR PHYSICIAN OFFICE VISITS
- The majority of covered workers are enrolled in health plans that require cost sharing for an in-network physician office visit, in addition to any general annual deductible.25
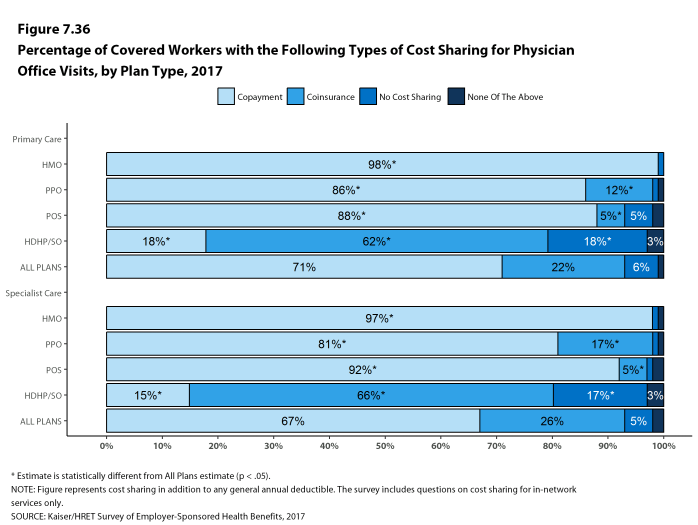
- The most common form of physician office visit cost sharing for in-network services is copayments. Seventy-one percent of covered workers have a copayment for a primary care physician office visit and 22% have coinsurance. For office visits with a specialty physician, 67% of covered workers have copayments and 26% have coinsurance [Figure 7.36].
- Over the last five years, the percentage of covered workers with coinsurance for office visits with a specialist has risen from 19% to 26%.
- Covered workers in HMOs, PPOs, and POS plans are much more likely to have copayments for both primary care and specialty care physician office visits than workers in HDHP/SOs. For primary care physician office visits, 62% of covered workers in HDHP/SOs have coinsurance, 18% have no cost sharing after the general annual plan deductible is met, and 18% have copayments [Figure 7.36].
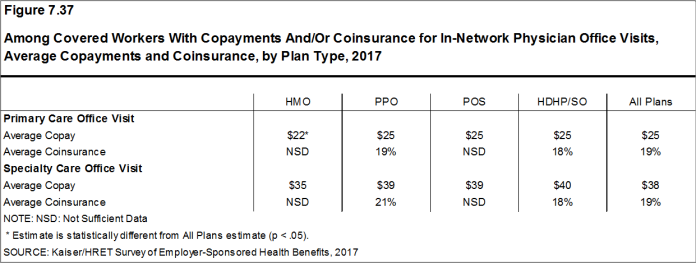
- Among covered workers with a copayment for in-network physician office visits, the average copayment is $25 for primary care and $38 for specialty physician office visits [Figure 7.37], similar to the amounts last year.
- Among covered workers with coinsurance for in-network physician office visits, the average coinsurance rates are 19% for a visit with a primary care physician and 19% for a visit with a specialist [Figure 7.37], similar to the rates last year.
Figure 7.36: Percentage of Covered Workers With the Following Types of Cost Sharing for Physician Office Visits, by Plan Type, 2017
Figure 7.37: Among Covered Workers With Copayments And/Or Coinsurance for In-Network Physician Office Visits, Average Copayments and Coinsurance, by Plan Type, 2017
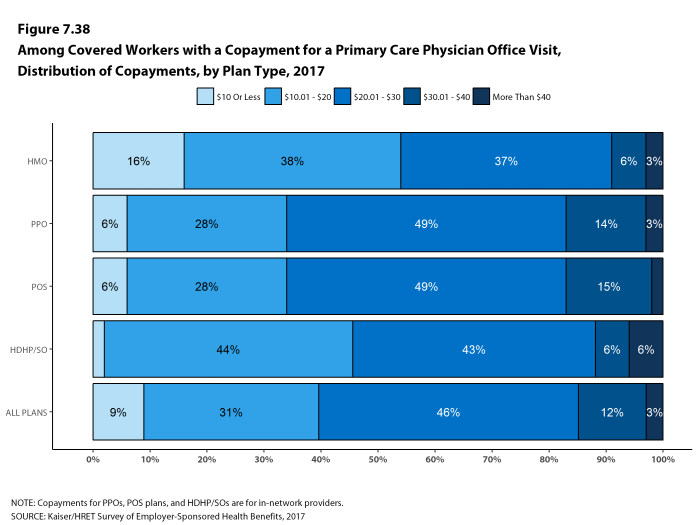
Figure 7.38: Among Covered Workers With a Copayment for a Primary Care Physician Office Visit, Distribution of Copayments, by Plan Type, 2017
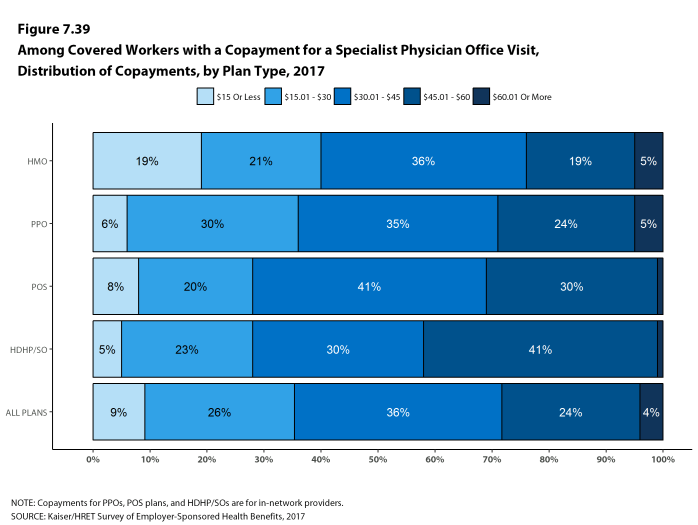
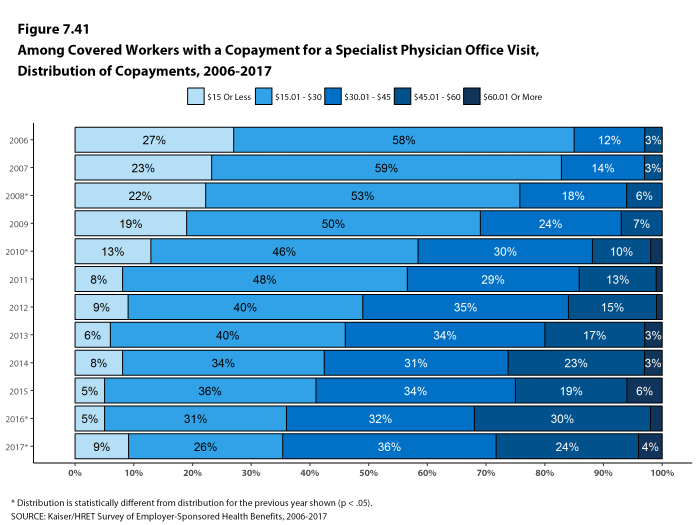
Figure 7.39: Among Covered Workers With a Copayment for a Specialist Physician Office Visit, Distribution of Copayments, by Plan Type, 2017
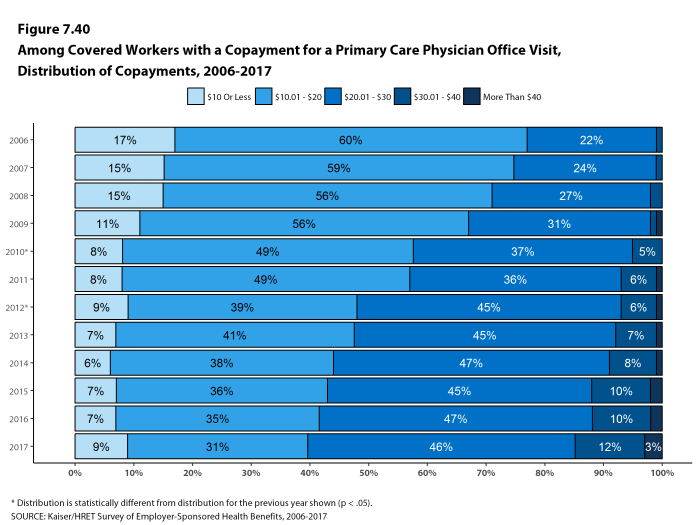
Figure 7.40: Among Covered Workers With a Copayment for a Primary Care Physician Office Visit, Distribution of Copayments, 2006-2017
OUT-OF-POCKET MAXIMUM AMOUNTS
- Most covered workers are in a plan that partially or totally limits the cost sharing that a plan enrollee must pay in a year. These limits are generally referred to as out-of-pocket maximum amounts. The Affordable Care Act (ACA) requires that non-grandfathered health plans have an out-of-pocket maximum of $7,150 or less for single coverage and $14,300 for family coverage.26 Many plans have complex out-of-pocket structures, which makes it difficult to accurately collect information on this element of plan design.
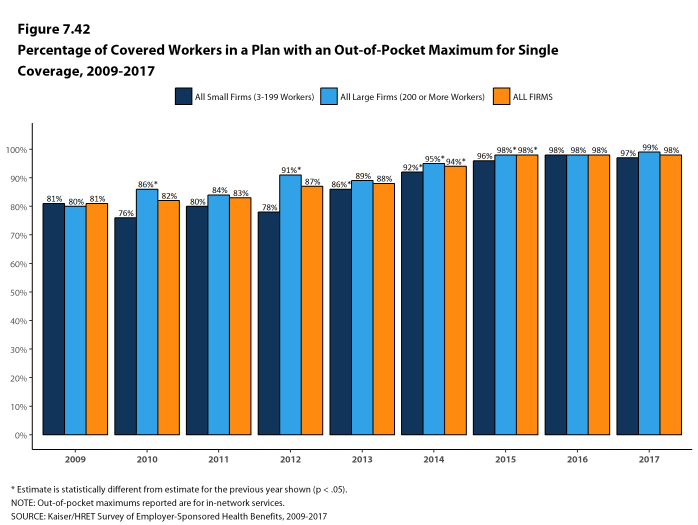
- In 2017, 98% percent of covered workers are in a plan with an out-of-pocket maximum for single coverage. This is a significant increase from 87% in 2012 [Figure 7.42].
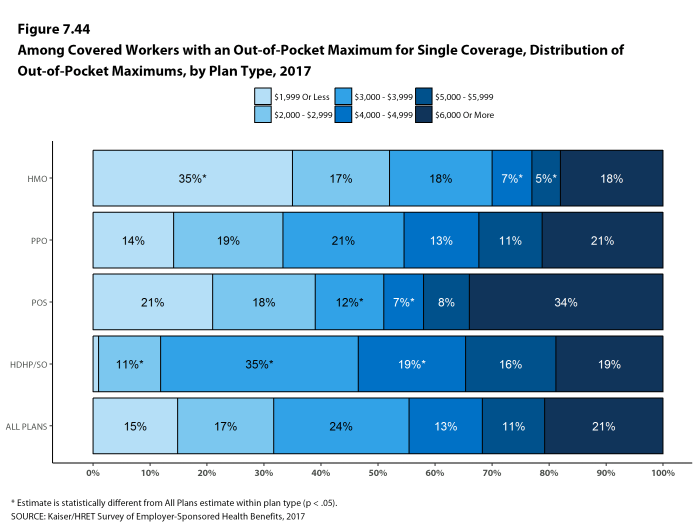
- For covered workers in plans with out-of-pocket maximums for single coverage, there is wide variation in spending limits.
- Fifteen percent of covered workers in plans with an out-of-pocket maximum for single coverage have an out-of-pocket maximum of less than $2,000, while 21% have an out-of-pocket maximum of $6,000 or more [Figure 7.44].
Figure 7.42: Percentage of Covered Workers In a Plan With an Out-Of-Pocket Maximum for Single Coverage, 2009-2017
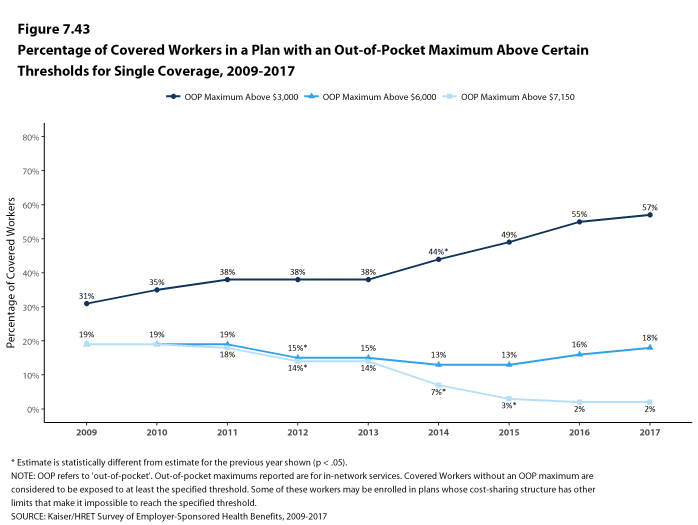
Figure 7.43: Percentage of Covered Workers In a Plan With an Out-Of-Pocket Maximum Above Certain Thresholds for Single Coverage, 2009-2017
Figure 7.44: Among Covered Workers With an Out-Of-Pocket Maximum for Single Coverage, Distribution of Out-Of-Pocket Maximums, by Plan Type, 2017
- Some workers with separate per-person deductibles or out-of-pocket maximums for family coverage do not have a specific number of family members that are required to meet the deductible amount and instead have another type of limit, such as a per-person amount with a total dollar amount limit. These responses are included in the averages and distributions for separate family deductibles and out-of-pocket maximums.↩
- Starting in 2010, the survey asked about the prevalence and cost of physician office visits separately for primary care and specialty care. Prior to the 2010 survey, if the respondent indicated the plan had a copayment for office visits, we assumed the plan had a copayment for both primary and specialty care visits. The survey did not allow for a respondent to report that a plan had a copayment for primary care visits and coinsurance for visits with a specialist physician. The changes made in 2010 allow for variations in the type of cost sharing for primary care and specialty care visits. The survey includes cost sharing for in-network services only.↩
- For those enrolled in an HDHP/HSA, the out-of-pocket maximum is $6,550 for an individual plan and $13,100 for a family plan.↩