Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity
| Key Findings |
Social determinants of health are the conditions in which people are born, grow, live, work and age that shape health. This brief provides an overview of social determinants of health and emerging initiatives to address them. It shows:
|
Introduction
Efforts to improve health in the U.S. have traditionally looked to the health care system as the key driver of health and health outcomes. However, there has been increased recognition that improving health and achieving health equity will require broader approaches that address social, economic, and environmental factors that influence health. This brief provides an overview of these social determinants of health and discusses emerging initiatives to address them.
What are Social Determinants of Health?
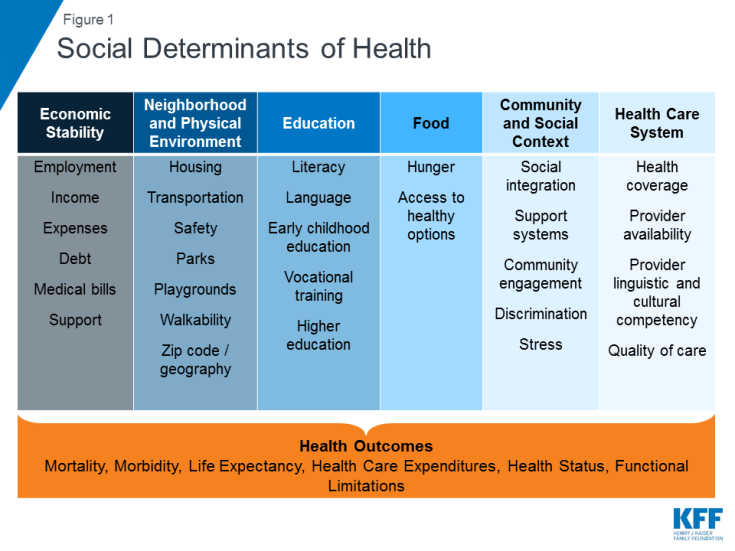
Social determinants of health are the conditions in which people are born, grow, live, work and age.1 They include factors like socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care (Figure 1).
Addressing social determinants of health is important for improving health and reducing health disparities.2 Though health care is essential to health, it is a relatively weak health determinant.3 Research shows that health outcomes are driven by an array of factors, including underlying genetics, health behaviors, social and environmental factors, and health care. While there is currently no consensus in the research on the magnitude of the relative contributions of each of these factors to health, studies suggest that health behaviors, such as smoking, diet, and exercise, and social and economic factors are the primary drivers of health outcomes, and social and economic factors can shape individuals’ health behaviors. For example, children born to parents who have not completed high school are more likely to live in an environment that poses barriers to health such as lack of safety, exposed garbage, and substandard housing. They also are less likely to have access to sidewalks, parks or playgrounds, recreation centers, or a library.4 Further, evidence shows that stress negatively affects health across the lifespan5 and that environmental factors may have multi-generational impacts.6 Addressing social determinants of health is not only important for improving overall health, but also for reducing health disparities that are often rooted in social and economic disadvantages.
Initiatives to Address Social Determinants of Health
A growing number of initiatives are emerging to address social determinants of health. Some of these initiatives seek to increase the focus on health in non-health sectors, while others focus on having the health care system address broader social and environmental factors that influence health.
Focus on Health in Non-Health Sectors
Policies and practices in non-health sectors have impacts on health and health equity. For example, the availability and accessibility of public transportation affects access to employment, affordable healthy foods, health care, and other important drivers of health and wellness. Nutrition programs and policies can also promote health, for example, by supporting healthier corner stores in low-income communities,7 farm to school programs8 and community and school gardens, and through broader efforts to support the production and consumption of healthy foods.9 The provision of early childhood education to children in low-income families and communities of color helps to reduce achievement gaps, improve the health of low-income students, and promote health equity.10
“Health in All Policies” is an approach that incorporates health considerations into decision making across sectors and policy areas.11 A Health in All Policies approach identifies the ways in which decisions in multiple sectors affect health, and how improved health can support the goals of these multiple sectors. It engages diverse partners and stakeholders to work together to promote health, equity, and sustainability, and simultaneously advance other goals such as promoting job creation and economic stability, transportation access and mobility, a strong agricultural system, and improved educational attainment. States and localities are utilizing the Health in All Policies approach through task forces and workgroups focused on bringing together leaders across agencies and the community to collaborate and prioritize a focus on health and health equity.12 At the federal level, the Affordable Care Act (ACA) established the National Prevention Council, which brings together senior leadership from 20 federal departments, agencies, and offices, who worked with the Prevention Advisory Group, stakeholders, and the pubic to develop the National Prevention Strategy.
Place-based initiatives focus on implementing cross-sector strategies to improve health in neighborhoods or communities with poor health outcomes. There continues to be growing recognition of the relationship between neighborhoods and health, with zip code understood to be a stronger predictor of a person’s health than their genetic code.13 A number of initiatives focus on implementing coordinated strategies across different sectors in neighborhoods with social, economic, and environmental barriers that lead to poor health outcomes and health disparities. For example, the Harlem Children’s Zone (HCZ) project focuses on children within a 100-block area in Central Harlem that had chronic disease and infant mortality rates that exceeded rates for many other sections of the city as well as high rates of poverty and unemployment. HCZ seeks to improve the educational, economic, and health outcomes of the community through a broad range of family-based, social service, and health programs.
Addressing Social Determinants in the Health Care System
In addition to the growing movement to incorporate health impact/outcome considerations into non-health policy areas, there are also emerging efforts to address non-medical, social determinants of health within the context of the health care delivery system. These include multi-payer federal and state initiatives, Medicaid initiatives led by states or by health plans, as well as provider-level activities focused on identifying and addressing the non-medical, social needs of their patients.
Federal and State Initiatives
In 2016, Center for Medicare and Medicaid Innovation (CMMI), which was established by the ACA, announced a new “Accountable Health Communities” model focused on connecting Medicare and Medicaid beneficiaries with community services to address health-related social needs. The model provides funding to test whether systematically identifying and addressing the health-related social needs of Medicare and Medicaid beneficiaries through screening, referral, and community navigation services will affect health costs and reduce inpatient and outpatient utilization. In 2017, CMMI awarded 32 grants to organizations to participate in the model over a five-year period. Twelve awardees will provide navigation services to assist high-risk beneficiaries with accessing community services and 20 awardees will encourage partner alignment to ensure that community services are available and responsive to the needs of enrollees.14
Through the CMMI State Innovation Models Initiative (SIM), a number of states are engaged in multi-payer delivery and payment reforms that include a focus on population health and recognize the role of social determinants. SIM is a CMMI initiative that provides financial and technical support to states for the development and testing of state-led, multi-payer health care payment and service delivery models that aim to improve health system performance, increase quality of care, and decrease costs. To date, the SIM initiative has awarded nearly $950 million in grants to over half of states to design and/or test innovative payment and delivery models. As part of the second round of SIM grant awards, states are required to develop a statewide plan to improve population health. States that received Round 2 grants are pursuing a variety of approaches to identify and prioritize population health needs; link clinical, public health, and community-based resources; and address social determinants of health.
- All 11 states that received Round 2 SIM testing grants plan to establish links between primary care and community-based organizations and social services.15 For example, Ohio is using SIM funds, in part, to support a comprehensive primary care (CPC) program in which primary care providers connect patients with needed social services and community-based prevention programs. As of December 2017, 96 practices were participating in the CPC program. Connecticut’s SIM model seeks to promote an Advanced Medical Home model that will address the wide array of individuals’ needs, including environmental and socioeconomic factors that contribute to their ongoing health.
- A number of the states with Round 2 testing grants are creating local or regional entities to identify and address population health needs and establish links to community services. For example, Washington State established nine regional “Accountable Communities of Health,” which will bring together local stakeholders from multiple sectors to determine priorities for and implement regional health improvement projects.16 Delaware plans to implement ten “Healthy Neighborhoods” across the state that will focus on priorities such as healthy lifestyles, maternal and child health, mental health and addiction, and chronic disease prevention and management.17 Idaho is creating seven “Regional Health Collaboratives” through the state’s public health districts that will support local primary care practices in Patient-Centered Medical Home transformation and create formal referral and feedback protocols to link medical and social services providers.18
- The Round 2 testing grant states also are pursuing a range of other activities focused on population health and social determinants. Some of these activities include using population health measures to qualify practices as medical homes or determine incentive payments, incorporating use of community health workers in care teams, and expanding data collection and analysis infrastructure focused on population health and social determinants of health.19
Medicaid Initiatives
Delivery System and Payment Reform
A number of delivery and payment reform initiatives within Medicaid include a focus on linking health care and social needs. In many cases, these efforts are part of the larger multi-payer SIM models noted above and may be part of Section 1115 Medicaid demonstration waivers.20 For example, Colorado and Oregon are implementing Medicaid payment and delivery models that provide care through regional entities that focus on integration of physical, behavioral, and social services as well as community engagement and collaboration.
- In Oregon, each Coordinated Care Organization (or “CCO”) is required to establish a community advisory council and develop a community health needs assessment.21 CCOs receive a global payment for each enrollee, providing flexibility for CCOs to offer “health-related services” – which supplement traditional covered Medicaid benefits and may target the social determinants of health.22 Early experiences suggest that CCOs are connecting with community partners and beginning to address social factors that influence health through a range of projects. For example, one CCO has funded a community health worker to help link pregnant or parenting teens to health services and address other needs, such as housing, food, and income.23 Another CCO worked with providers and the local Meals on Wheels program to deliver meals to Medicaid enrollees discharged from the hospital who need food assistance as part of their recovery.24 An evaluation conducted by the Oregon Health & Science University’s Center for Health Systems Effectiveness released in 2017 found CCOs were associated with reductions in spending growth and improvement in some quality domains.25 According to the evaluation, most CCOs believed health-related flexible services were effective at improving outcomes and reducing costs.26
- Similarly, in Colorado, the Regional Collaborative Organizations (RCCOs), which are paid a per member per month payment for enrollees, help connect individuals to community services through referral systems as well as through targeted programs designed to address specific needs identified within the community.27 A study published in 2017 comparing Oregon’s CCO program to Colorado’s RCCO program found that Colorado’s RCCO program generated comparable reductions in expenditures and inpatient care days.28
Several other state Medicaid programs have launched Accountable Care Organization (ACO) models that often include population-based payments or total cost of care formulas, which may provide incentives for providers to address the broad needs of Medicaid beneficiaries, including the social determinants of health.29
Some state Medicaid programs are supporting providers’ focus on social determinants of health through “Delivery System Reform Incentive Payment” (DSRIP) initiatives. DSRIP initiatives emerged under the Obama Administration as part of Section 1115 Medicaid demonstration waivers. DSRIP initiatives link Medicaid funding for eligible providers to process and performance metrics, which may involve addressing social needs and factors. For example, in New York, provider systems may implement DSRIP projects aimed at ensuring that people have supportive housing. The state also has invested significant state dollars outside of its DSRIP waiver in housing stock to ensure that a better supply of appropriate housing is available.30 In Texas, some providers have used DSRIP funds to install refrigerators in homeless shelters to improve individuals’ access to insulin.31 The California DSRIP waiver has increased the extent to which the public hospital systems focus on coordination with social services agencies and county-level welfare offices.32 To date, data on the results of DSRIP programs are limited, but a final federal evaluation report is scheduled to for 2019.33
Medicaid programs also are providing broader services to support health through the health homes option established by the ACA. Under this option, states can establish health homes to coordinate care for people who have chronic conditions. Health home services include comprehensive care management, care coordination, health promotion, comprehensive transitional care, patient and family support, as well as referrals to community and social support services. Health home providers can be a designated provider, a team of health professionals linked to a designated provider, or a community health team. A total of 21 states report that health homes were in place in fiscal year 2017.34 A federally-funded evaluation of the health homes model found that most providers reported significant growth in their ability to connect patients to nonclinical social services and supports under the model, but that lack of stable housing and transportation were common problems for many enrollees that were difficult for providers to address with insufficient affordable housing and rent support resources.35
Housing and Employment Supports
Some states are providing housing support to Medicaid enrollees through a range of optional state plan and waiver authorities. While states cannot use Medicaid funds to pay for room and board, Medicaid funds can support a range of housing-related activities, including referral, support services, and case management services that help connect and retain individuals in stable housing.36 For example, the Louisiana Department of Health formed a partnership with the Louisiana Housing Authority to establish a Permanent Supportive Housing (PSH) program with the dual goals of preventing and reducing homelessness and unnecessary institutionalization among people with disabilities. Louisiana’s Medicaid program covers three phases of tenancy support services for Medicaid beneficiaries in permanent supportive housing: pre-tenancy services (housing search assistance, application assistance etc.), move-in services, and ongoing tenancy services.37 Louisiana reports a 94% housing retention rate since the program began housing tenants in 2008. A preliminary analysis shows statistically significant reductions in hospitalizations and emergency department utilization after the PSH intervention, and an early independent analysis of the PSH program’s impact on Medicaid spending found a 24% reduction in Medicaid acute care costs after a person was housed.38
Through a range of optional and waiver authorities, some states are providing voluntary supported employment services to Medicaid enrollees. Supported employment services may include pre-employment services (e.g., employment assessment, assistance with identifying and obtaining employment, and/or working with employer on job customization) as well as employment sustaining services (e.g., job coaching and/or consultation with employers). States often target these services to specific Medicaid populations, such as persons with serious mental illness or substance use disorders and individuals with intellectual or developmental disabilities. For example, under a Section 1115 waiver, Hawaii offers supportive employment services to Medicaid enrollees with serious mental illness (SMI), individuals with serious and persistent mental illness (SPMI), and individuals who require support for emotional and behavioral development (SEBD).39
Medicaid Managed Care Organizations (MCOs)
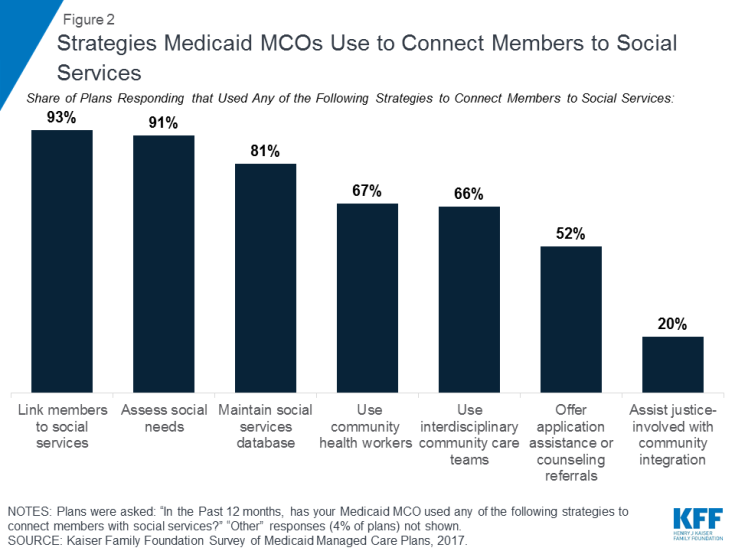
Medicaid MCOs are increasingly engaging in activities to address social determinants of health. Data from the Kaiser Family Foundation’s 50-state Medicaid budget survey show that a growing number of states are requiring Medicaid MCOs to address social determinants of health as part of their contractual agreements (Box 1). In 2017, 19 states required Medicaid MCOs to screen beneficiaries for social needs and/or provide enrollees with referrals to social services and six states required MCOs to provide care coordination services to enrollees moving out of incarceration, with additional states planning to implement such requirements in 2018.40 Other data from a 2017 Kaiser Family Foundation survey of Medicaid managed care plans show that almost all responding MCOs41 (91%) reported activities to address social determinants of health, with housing and nutrition/food security as the top areas of focus.42 The most common activities plans reported engaging in were working with community -based organizations to link members to social services (93%), assessing members’ social needs (91%), and maintaining community or social service resource databases (81%) (Figure 2).43 Some plans also reported using community health workers (67%), using interdisciplinary community care teams (66%), offering application assistance and counseling referrals for social services (52%), and assisting justice-involved individuals with community reintegration (20%).
|
Box 1: Examples of States Integrating Social Determinants into Medicaid Managed Care Contracts |
|
PROVIDER ACTIVITIES
Under the ACA, not-for-profit hospitals are required to conduct a community health needs assessment (CHNA) once every three years and develop strategies to meet needs identified by the CHNA. The CDC defines a community health assessment as “the process of community engagement; collection, analysis, and interpretation of data on health outcomes and health determinants; identification of health disparities; and identification of resources that can be used to address priority needs.”44 Under the ACA, the assessment must take into account input from people who represent the broad interests of the community being served, including those with public health knowledge or expertise.
Some providers have adopted screening tools within their practices to identify health-related social needs of patients. For example, according to a survey of nearly 300 hospitals and health systems conducted by the Deloitte Center for Health Solutions in 2017, nearly 9 in 10 (88%) hospitals screen patients to gauge their health-related social needs, though only 62% report screening target populations in a systematic or consistent way.45 These hospitals are mostly screening inpatient and high-utilizer populations.46 The National Association for Community Health Centers, in coordination with several other organizations, developed the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) tool to help health centers and other providers collect data to better understand and act on their patients’ social determinants of health. Other organizations and entities have created screening tools, including Health Leads, a non-profit organization funded by the Robert Wood Johnson Foundation, which has developed a social needs screening toolkit for providers and CMMI, which released an Accountable Health Communities screening tool to help providers identify unmet patient needs.47
Looking Ahead
The ACA provided a key opportunity to help improve access to care and reduce longstanding disparities faced by historically underserved populations through both its coverage expansions and provisions to help bridge health care and community health. To date, millions of Americans have gained coverage through the coverage expansions, but coverage alone is not enough to improve health outcomes and achieve health equity. With growing recognition of the importance of social factors to health outcomes, an increasing number of initiatives have emerged to address social determinants of health by bringing a greater focus on health within non-health sectors and increasingly recognizing and addressing health-related social needs through the health care system.
Within the health care system, a broad range of initiatives have been launched at the federal and state level, including efforts within Medicaid. Many of these initiatives reflect new funding and demonstration authorities provided through the ACA to address social determinants of health and further health equity. They also reflect a broader system movement toward care integration and “whole-person” delivery models, which aim to address patients’ physical, mental, and social needs, as well as a shifts towards payments tied to value, quality, and/or outcomes.
Although there has been significant progress recognizing and addressing social determinants of health, many challenges remain. Notably, these efforts require working across siloed sectors with separate funding streams, where investments in one sector may accrue savings in another. Moreover, communities may not always have sufficient service capacity or supply to meet identified needs. Further, there remain gaps and inconsistencies in data on social determinants of health that limit the ability to aggregate data across settings or to use data to inform policy and operations, guide quality improvement, or evaluate interventions.48 Within Medicaid, the growing focus on social determinants of health raises new questions about the appropriate role Medicaid should play in addressing non-medical determinants of health and how to incentivize and engage Medicaid MCOs in addressing social determinants of health.49
The Trump Administration is pursuing policies that may limit individuals’ access to assistance programs to address health and other needs and reduce resources to address social determinants of health. The Administration has begun phasing out DSRIP programs,50 is revising Medicaid managed care regulations,51 and has signaled reductions in funding for prevention and public health. It has also announced plans to change the direction of models under the CMMI.52, 53, 54 The Administration also is pursuing approaches to enforce and expand work requirements in public programs,55 including Medicaid.56 CMS asserts that this policy is designed to “improve Medicaid enrollee health and well-being through incentivizing work and community engagement” and that state efforts to make participation in work or other community engagement a requirement for Medicaid coverage may “help individuals and families rise out of poverty and attain independence.”57 In guidance, CMS has specified that states implementing such programs will be required to describe strategies to assist enrollees in meeting work requirements (e.g., linking individuals to job training, childcare assistance, transportation, and other work supports), but that states may not use federal Medicaid funds for supportive services to help people overcome barriers to work.58 Data show that most nonelderly Medicaid adults already are working or face significant barriers to work, leaving a small share of adults to whom these policies are directed.59 However, eligible individuals could lose Medicaid coverage due to difficulty navigating documentation and administrative processes associated with these requirements.60