Racial Disparities in COVID-19 Impacts and Vaccinations for Children
Introduction
Although children have not borne the most severe brunt of COVID-19 relative to adults, some do become hospitalized, suffer long-term consequences, and even death from the disease. There is growing attention to how children are being affected by the pandemic, particularly as in-person school returns, and those younger than age 12 are not yet eligible for vaccination. While data remain limited, available research and data to date suggest that children of color have been disproportionately affected by COVID-19 and may be less likely to have been vaccinated, mirroring racial disparities observed among the broader population. These disparities may leave children of color at increased risk, particularly as they return to in-person school. Together the findings point to the importance of increasing data available to understand racial disparities in COVID-19 impacts and vaccinations among children and efforts to mitigate disproportionate impacts of COVID-19 for children of color going forward.
Findings
Disparities in COVID-19 Impacts among Children
Research suggests COVID-19 has disproportionately affected the health of children of color in ways that mirror patterns observed among adults. Studies find that, compared to their White counterparts, Black, Hispanic, and Asian children had lower rates of testing but were significantly more likely to be infected; Black and Hispanic children were more likely to be hospitalized and more likely to have multisystem inflammatory syndrome (MIS-C (a serious and sometimes deadly condition where different body parts become inflamed, including the heart, lungs, kidneys, and brain); Black children were more likely to be admitted to intensive care units due to MIS-C; and Hispanic, Black, and American Indian and Alaska Native (AIAN) children had higher rates of death. Recent data from CDC also show racial disparities in COVID-19 health impacts. As of August 31, 2021, there were almost 4.9 million infections, over 39,000 hospitalizations, and 725 deaths due to COVID-19 among children 19 and younger, which showed:
- Infection rates were highest among AIAN, Native Hawaiian and Other Pacific Islander (NHOPI), and Hispanic children at over 500 cases per 10,000 people (Figure 1). White and Black children had over 300 cases per 10,000 people, while Asian children had the lowest infection rate at just over 200 cases per 10,000 people.
- AIAN and Hispanic children had the highest rates of hospitalization, followed by NHOPI and Black children, who are two to three times as likely to be hospitalized than White children. Asian children had the lowest hospitalization rate.
- There were large disparities in deaths for AIAN and Black children, whose death rates were over 3.5 and 2.7 times higher than the rate for White children, respectively. Hispanic children also were more likely to die than their White counterparts, while Asian children had a lower death rate. Deaths among NHOPI children were not reported due to insufficient data.
The pandemic has also adversely impacted children’s mental, social and academic growth, with Hispanic and Black children bearing the brunt of these impacts. A recent KFF Vaccine Monitor report shows that half of Hispanic parents say one of their children fell behind academically as a result of the pandemic compared to about a third (35%) of White parents who say the same. Additionally, half of Hispanic parents (52%) say one of their children experienced difficulty concentrating on school work, issues with sleeping and eating, or frequent headaches or stomachaches since the pandemic began, compared to less than four in ten (40%) White parents. Black and Hispanic parents also are more likely to say their household suffered a job disruption due to childcare needs in the past year and to say that the disruption has had a major impact on their family’s finances and stress level. These findings are consistent with a 2020 McKinsey analysis finding that Black and Latino students would disproportionately experience learning loss during the pandemic due to a variety of reasons, including a lack of access to high-quality remote learning, and high-speed internet. These disproportionate impacts of the pandemic may further widen existing gaps in academic performance for children of color.
Disparities COVID-19 Vaccinations among Children
Children ages 12 and older became eligible for COVID-19 vaccination on May 10, 2021, while children under age 12 are not yet eligible for vaccination at this time. Ensuring equity in COVID-19 vaccinations among children is important for mitigating the disproportionate impacts of COVID-19 and preventing widening disparities going forward. Moreover, because children make up a significant share of the population and are more racially diverse than the rest of the population, equitable vaccination among this group is key for achieving an overall high rate of vaccine coverage among the population and may help to reduce disparities in vaccination rates more broadly.
There is a dearth of data to examine vaccination rates by race/ethnicity among children, but the available data point to potential racial disparities in vaccinations among children. As of September 7, 2021, federal data were not available on vaccinations among children by race/ethnicity and just seven states were reporting these data. White children had higher vaccination rates than Black children in all seven reporting states, although the size of these differences varied widely across states (Figure 2). The vaccination rate for White children was higher than the rate for Hispanic children in two states (Connecticut, and Wisconsin), although the differences between rates were generally smaller than the differences in rates between White and Black children. Hispanic children had a similar or higher vaccination rate than White children in the remaining five states. In the five states for which we were able to calculate vaccination rates for Asian children, the rate for Asian children was higher compared to that of White children.
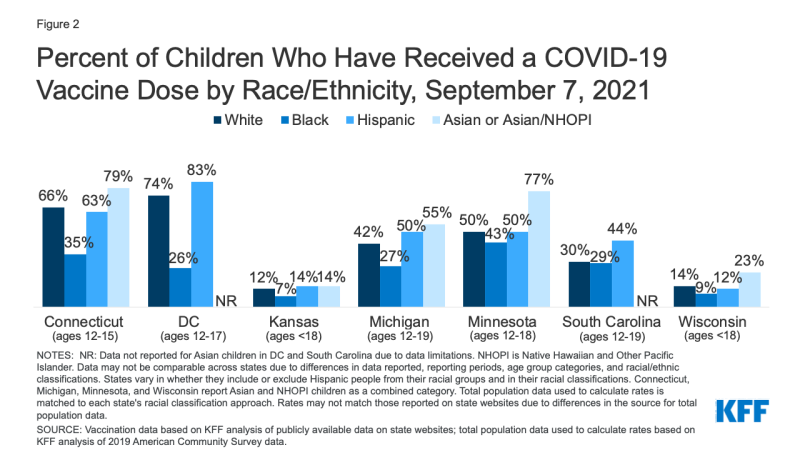
Figure 2: Percent of Children Who Have Received a COVID-19 Vaccine Dose by Race/Ethnicity, September 7, 2021
KFF COVID Vaccine Monitor data show that Hispanic and Black parents are more likely than White parents to report potential access barriers to vaccination. Across racial/ethnic groups, the top concerns about the COVID-19 vaccine for parents of unvaccinated teens center around the potential for long-term or serious side effects in children. However, consistent with surveys of adults, Hispanic and Black parents are more likely than White parents to cite concerns that reflect access barriers to vaccination, including not being able to get the vaccine from a trusted place, believing they may have to pay an out-of-pocket cost, or having difficulty traveling to a vaccination site. A larger share of Hispanic parents than White parents also reports being concerned about needing to take time off work to get their child vaccinated.
Ensuring equity in vaccinations when children under the age of 12 become eligible for vaccination will be particularly important given the size and racial diversity of this group. There are 48 million children under the age of 12 in the United States, almost three times the number of adolescents, aged 12-15, who became eligible in May 2021. About half (50.5%) of children under the age of 12 are children of color, including more than a quarter (25.8%) who are Hispanic. An additional 13.3% are Black, 4.7% are Asian, and the remaining 6.7% are American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, or multiracial Some states have even larger shares of children of color.
Looking Ahead
Together these data suggest that COVID-19 has disproportionately negatively affected the physical and mental health, academic growth, and economic security of children of color. At the same time, the limited data available to date suggest some children of color may be less likely to receive a COVID-19 vaccine, leaving them at elevated risk as the virus continues to spread and as many return to in-person school.
Exposure risk associated with returning to in-person school may be mitigated by policies such as requiring face masks or vaccination among staff and eligible students in schools or by providing options for virtual learning. Because many of these decisions are being made at the local level, there will be wide variation in implementation of these protections across the country. However, some decisions are being made at the state level. For example, as of September 13, 2021, 18 states were requiring face masks in schools, 28 states did not have a face mask requirement in schools, and 5 states prohibited a face mask requirement in schools. Nine states had a vaccine mandate for school employees. While most states (29) are leaving decisions about school instruction mode to the local level, 19 states have a requirement for in-person learning and 3 have a requirement for hybrid learning. This varied implementation of mitigation policies also will have important implication for disparities in COVID-19 impacts among children going forward.
