
The independent source for health policy research, polling, and news.
Timely insights and analysis from KFF staff
Back to the Future? A look back at High-Risk Pools
This week, Senator J.D. Vance suggested moving higher-risk individuals to different insurance risk pools than healthier ones – following up on former President Donald Trump’s “concepts of a plan” for replacing the Affordable Care Act. But what could such a policy mean for health coverage and costs? We can look back to a time before the ACA for some answers.
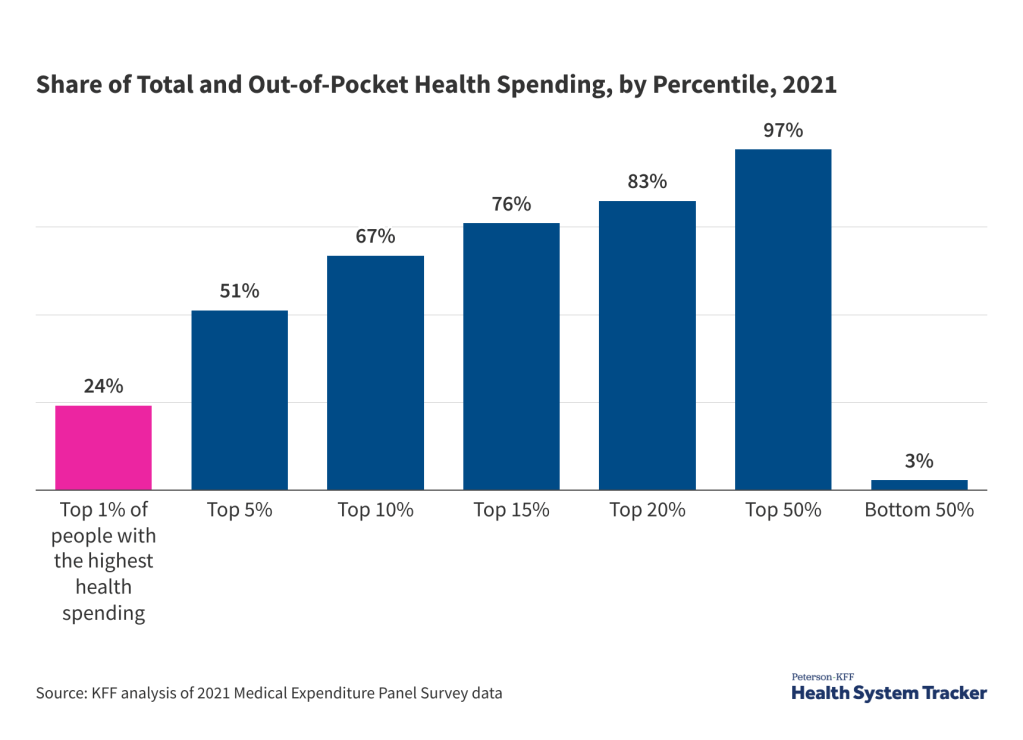
But first, it’s important to know that at any given time, most people are relatively healthy. The 5% of the population with the highest health costs makes up about half of total health spending. Removing the people with the highest health costs could significantly decrease premiums (before subsidies) for the healthier group, while significantly increasing premiums for sicker people.
Before the Affordable Care Act (ACA) mandated insurers cover people with pre-existing conditions, “high-risk pools”, which existed in 35 states starting in the 1970s, provided insurance for some of those who were deemed “uninsurable” by individual market insurers due to their health conditions.
However, these pools were plagued by:
- High costs: Premiums were often double what healthier people paid.
- Exclusions for pre-existing conditions: Nearly all state high-risk pools excluded coverage of pre-existing conditions, usually for 6-12 months.
- Lifetime limits: Most included a lifetime limit on coverage, and some had annual limits.
- Capped enrollment: Some states limited how many people could buy through their high-risk pool.
Much of this was a result of underfunding. States offered subsidies, but even with these subsidies, people with pre-existing conditions often faced inadequate coverage or no coverage at all.
The ACA essentially eliminated the need for high-risk pools because insurers are now prohibited from medical underwriting – the practice of screening people for pre-existing conditions and charging them more or denying them coverage based on their health status. Healthy, sick, young, and old people buying an ACA plan are now in a single risk pool. With ACA subsidies, how much people pay for their premiums is on a sliding scale based on their income.
High-risk pools could theoretically protect people with pre-existing conditions, but only with sufficient government funding, which they’ve never had.
