Will Where You Live Determine Access and Coverage of Emerging Anti-Obesity Drugs?
This document was updated on Sept. 8, 2023 to cite a related analysis.
Key health organizations began recognizing obesity as a disease a decade or more ago and treatment methods for the condition have ranged from behavior change counseling to bariatric surgery. A class of prescription drugs (GLP-1) that can result in substantial weight loss is emerging as a potentially revolutionary treatment for the one-third of U.S. adults who are obese* (having a body mass index of 30 or above). But, health coverage and access in the fragmented U.S. health care system is determined by many actors, and the rate of obesity in the state of residence could factor into coverage, and therefore how accessible and affordable this class of drugs is for patients.
A look at KFF’s State Health Facts indicator of the distribution of adults with a body mass index (BMI) of 30 or more shows that the 20 states with the highest rates of obesity are all in the Midwest and South, as classified by the U.S. Census Bureau (Figure 1).
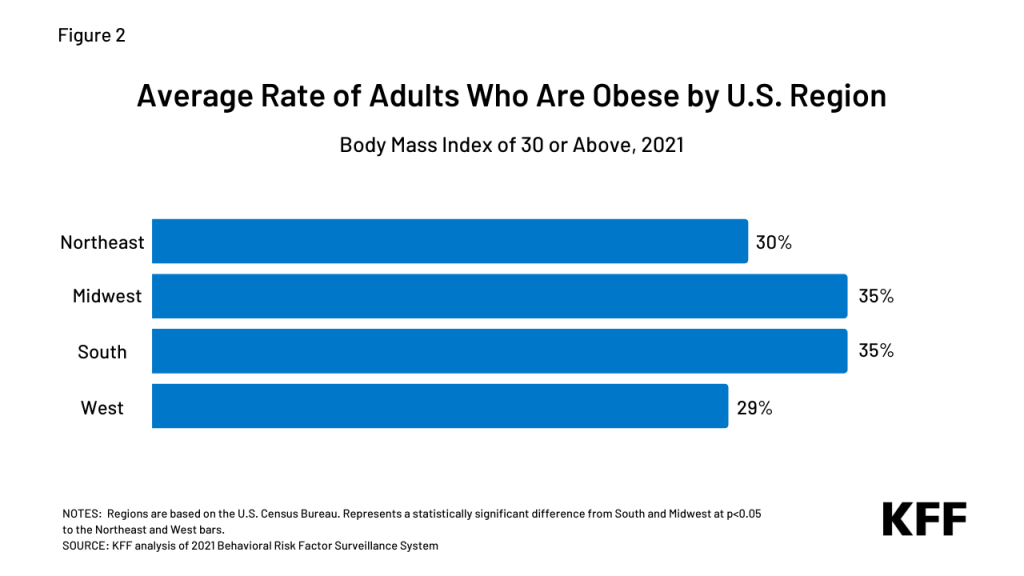
When comparing average obesity rates by region (Figure 2), adult rates in the Midwest and South are about five percentage points higher than the Northeast and six percentage points higher than the West.
The cost of treating adults who are obese with GLP-1 drugs would be substantial in the near term and could impact coverage policies. For state Medicaid programs in the Midwest and South, and employers and insurers with a significant presence in these regions, the higher rates of obesity among residents may factor into their decisions. Also a factor in access to these drugs, seven of ten states that have not adopted the Affordable Care Act’s Medicaid expansion and nearly all (97%) of the people experiencing a coverage gap due to non-expansion are in the South.
Currently, Medicaid coverage for drugs prescribed for weight loss varies by state but is generally limited for GLP-1 drugs, and employer-based and private insurance coverage of weight-loss drugs also varies. The Medicare program does not cover the drugs for weight loss due to a legislative ban.
Recent reports (Business Insider, STAT, WSJ) reveal some employers previously covering GLP-1 drugs are pulling back coverage and health insurers are scrutinizing physicians’ off-label prescribing. With the prospect of a dramatic increase in costs if the class of drugs continues to gain FDA approval, coverage of the drugs could stall, drop, or be restricted, including limiting coverage eligibility to people with a higher body mass index. (Obesity is typically classified into three ranges of BMI. The American Medical Association recently clarified its policy on the role of BMI as a measure of obesity, noting historical problems and its limitations.) Other potential actions include:
- Limiting off-label use,
- Requiring additional treatment like behavioral therapy in conjunction with the drugs,
- Prior authorization, including step-therapy to try less expensive options first, and
- Higher cost-sharing.
The early clinical results and potential of new prescription drugs for weight loss have caught the interest of nearly half of U.S. adults. Federal and state policymakers, employers and insurance coverage providers are in the early stages of considering these drugs’ potential costs and benefits in determining if and how to cover them in insurance plans. The long-term cost savings from a reduction in obesity and its related risks in the country could be substantial. Still, the current U.S. prices of these drugs for weight loss are high and their lifetime use may be required for continued health benefits. It is also important to note that some patients prescribed the drugs are experiencing side effects and their use’s long-term impact remains a question.
With adults in the Midwest and South having higher obesity rates, states’ coverage programs and regional employers could face higher health insurance costs – particularly in the short term – and seek ways to control the use of newer weight-loss drugs. As coverage of GLP-1 prescription drugs develops, regional trends could diverge.
*The Centers for Disease Control and Prevention’s (CDC) National Health and Nutrition Examination Survey, using clinical measurements, estimates about four in ten adults are obese. KFF estimates are based on analysis of state-level Behavioral Risk Factor Surveillance System self-reported data collected by the CDC and state health departments via phone calls.
