The Status of Medicaid Expansion in Missouri and Implications for Coverage and Cost
Madeline Guth, Rachel Garfield, Robin Rudowitz, and Anthony Damico
Published:
On June 23, 2021, a circuit court decision in Missouri put the state’s expansion of Medicaid under the Affordable Care Act (ACA) in limbo. Though a successful 2020 state ballot measure directed the expansion to be in effect by July 1, 2021, the legislature excluded expanded coverage from its fiscal year (FY) 2022 budget and the circuit court judge held that the state was not required to implement expansion. This decision, if upheld, has implications for coverage in the state as well as the availability of federal financing to cover the cost.
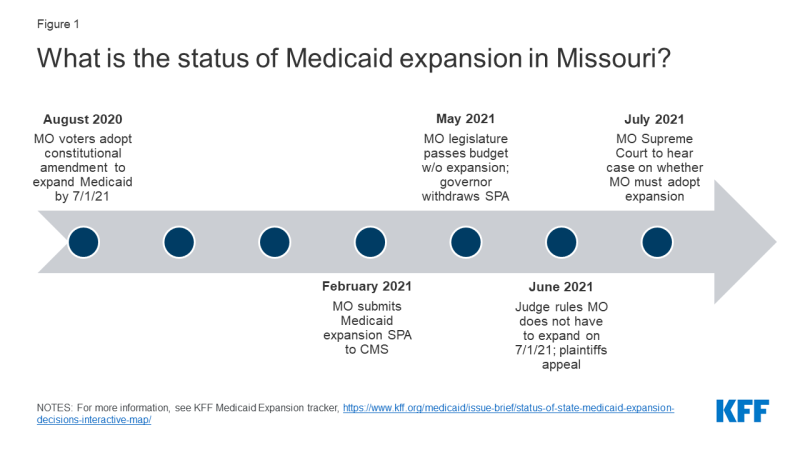
While expansion passed in Missouri through ballot initiative, the governor has since said that the state will not expand Medicaid because the legislature did not include expansion in its FY 2022 budget (Figure 1). On August 4, 2020, Missouri voters approved a ballot measure that added Medicaid expansion to the state’s constitution and required implementation of expansion coverage by July 1, 2021. Language in the constitutional amendment prohibits the imposition of additional burdens or restrictions on eligibility or enrollment for the expansion population (such as work requirements or premiums). In early 2021, Republican Governor Mike Parson included expansion in his proposed FY 2022 budget and the state submitted a State Plan Amendment (SPA) to CMS to implement expansion beginning July 1, 2021. In May, however, Governor Parson announced that the state’s Department of Social Services (DSS) was withdrawing its SPA submission and would not implement expansion as scheduled due to a lack of funding: the ballot measure did not include a revenue source and the Republican-controlled state legislature excluded the program from its final FY 2022 budget. Although advocates subsequently filed a lawsuit in state circuit county court against the DSS, in June a judge ruled that DSS’ refusal to expand Medicaid is lawful because the ballot initiative violated the state constitution by failing to provide a funding source. The plaintiffs appealed this decision and the state Supreme Court is set to hear oral arguments in this appeal on July 13.
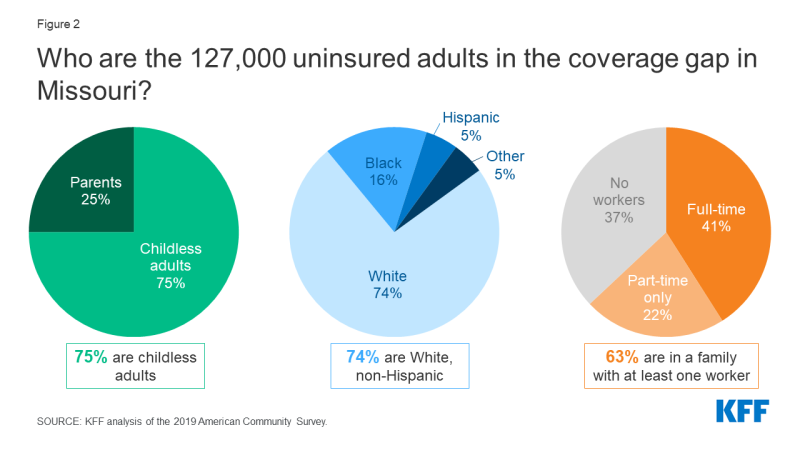
If the ACA Medicaid expansion does not proceed, the nearly 127,000 uninsured nonelderly adults who currently fall into the coverage gap would remain ineligible for coverage (Figure 2). These adults would be eligible if the state expanded but currently have incomes above Missouri’s current Medicaid levels (0% of the federal poverty level (FPL) for childless adults and 21% for parents) but below the 100% FPL ($12,880 for an individual or $21,960 for a family of 3 in 2021) minimum eligibility for tax credits through the ACA marketplace. National estimates by KFF indicate that nearly 2.2 million adults are in the coverage gap across all non-expansion states (these estimates exclude Missouri as the state had previously been scheduled to implement expansion in July). As in other states, most people in the coverage gap in Missouri are adults without dependent children (75%). Though most people in the Missouri coverage gap are White (74%), the gap disproportionately includes people of color when compared to the population of Missouri as a whole (79% White, non-Hispanic). Most (63%) adults in the coverage gap have at least one full-time (41%) or part-time only (22%) worker in their family. Without Medicaid expansion, those in the coverage gap have limited options for affordable health coverage and are likely to face barriers to needed health services.
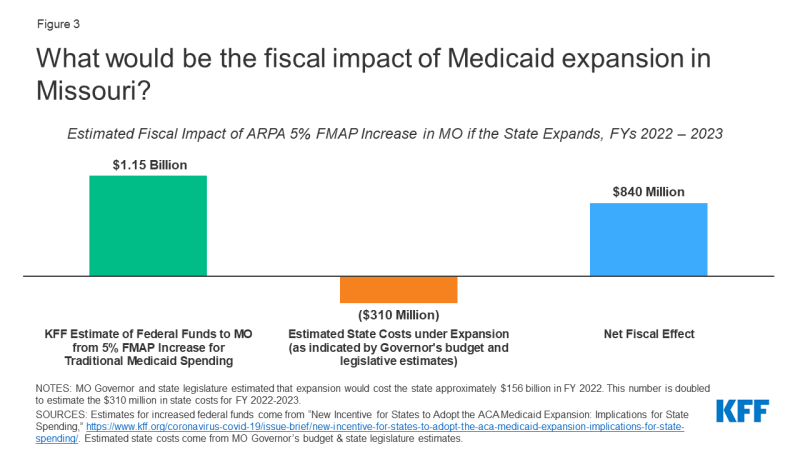
Not expanding Medicaid in Missouri would lead the state to forego more than $1 billion in additional federal funds available under the American Rescue Plan Act (ARPA) (Figure 3). Governor Parson’s proposed FY 2022 budget allocated $1.57 billion in total for the Medicaid expansion; the federal government would cover the vast majority of this cost as states receive a 90% federal matching rate (FMAP) for the expansion population. The Missouri Legislature estimated that state costs of expansion would be $156 million in FY 2022, but ultimately chose not to appropriate these funds. The state has recently seen increasing revenue and an unprecedented budget surplus. ARPA provides a temporary fiscal incentive for states to newly implement the ACA Medicaid expansion by providing a 5 percentage point increase in the state’s traditional FMAP for two years. This increase would more than offset Missouri’s increased costs of expansion: Missouri would receive an estimated $1.15 billion over FY 2022 to 2023 as a result of the ARPA financial incentive. However, the state would ultimately need to cover its 10% share of the cost of expansion over time.
A comprehensive literature review of Medicaid expansion studies identifies positive financial impacts of expansion for state budgets and economies, on top of improvements in coverage, access, and health outcomes for individuals. Excluding Missouri, the other 12 non-expansion states are foregoing an estimated $16.4 billion in additional federal funds available under the ARPA incentive (on top of the existing 90% expansion FMAP). Similar to Missouri, Oklahoma voters approved a Medicaid expansion initiated constitutional amendment in June 2020; unlike Missouri, however, expansion coverage in Oklahoma is scheduled to begin on July 1. Since ARPA was enacted prior to the implementation of the expansion, Oklahoma is eligible for the ARPA fiscal incentive. Enrollment in expansion coverage began June 1 in Oklahoma and neared 100,000 after just one week. While fiscal issues are part of the calculus for states not expanding Medicaid—i.e., the need to cover 10% of the cost over time—opposition to the ACA continues to be a factor as well.