Postpartum Coverage Extension in the American Rescue Plan Act of 2021
Usha Ranji, Alina Salganicoff, and Ivette Gomez
Published:
Inside the $1.9 trillion American Rescue Plan Act of 2021 is a less noticed provision that makes a major change to Medicaid coverage for low-income pregnant and postpartum women, addressing a long-standing gap for people who have had their maternity care covered by Medicaid, especially those in states that have not expanded Medicaid as permitted by the ACA. While the Act adds new incentives for states to take up the ACA Medicaid expansion, it also now gives all states the new option to extend the postpartum coverage period under Medicaid from 60 days following pregnancy to a full year. This post explains the new policy and raises some questions that policymakers are likely to grapple with as the implementation unfolds.
What does the new policy do?
- The American Rescue Plan Act of 2021 gives states a new option to extend Medicaid postpartum coverage from 60 days to 12 months. Currently, Medicaid covers almost half of births nationally, with eligibility levels ranging from 138% to 380% of poverty across states. States must cover pregnant women with incomes up to 138% of the federal poverty level (FPL) through 60 days postpartum (the end of the month of the 60th postpartum day). The American Rescue Plan Act allows states to extend the postpartum period to a year by filing a State Plan Amendment (SPA) to their Medicaid program.
- Under the new law, the postpartum coverage duration can also be lengthened under the CHIP program. Currently, six states cover some low-income pregnant women through their CHIP programs. If a state takes up the new option to extend the postpartum period, this will apply to their CHIP coverage in addition to Medicaid.
- States that elect the new option must provide full Medicaid benefits during pregnancy and the extended postpartum period. Currently, states are permitted to cover a more narrow set of pregnancy-related benefits to those who qualify under the pregnancy pathway, although most align their benefits with other Medicaid eligibility groups. States that elect this new option however would have to provide full Medicaid benefits.
- The new option can take effect starting April 1, 2022 and would be available to states for five years. While the new option takes effect next year, currently postpartum women covered by Medicaid can remain on the program beyond 60 days because of a Maintenance of Effort requirement enacted in 2020 that lasts through the COVID public health emergency.
Questions going forward
- Which states will take up this option? While we do not know which states will take up the option, several have shown interest in extending the postpartum coverage period beyond 60 days. Some states have applied and have waivers pending at CMS to extend postpartum coverage. This includes expansion states like Illinois and New Jersey as well as non-expansion states like Georgia (which applied for extension through 180 days postpartum). These states could now file a SPA instead of waiting for approval of their waivers. Some states may decide to change earlier proposals. For example, Missouri has submitted a waiver application to CMS that would extend postpartum coverage to a year just for substance use and mental health services. That proposal would not qualify for the new SPA option because it would not cover full benefits.
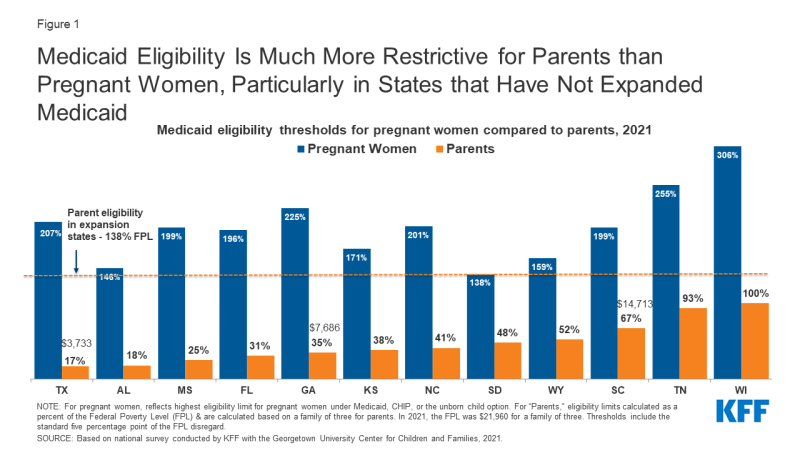
- What will be the impact on women’s coverage in non-expansion states? Non-expansion states that take up the option could see a decrease in the share of low-income mothers who are uninsured. Medicaid income eligibility levels for parents are much lower than for pregnant people (Figure 1). Currently, in non-expansion states, some new mothers fall into the coverage gap where their incomes are too high for Medicaid parent eligibility yet too low for Marketplace subsidies (which are available only at the poverty level or above), putting them at risk for becoming uninsured.
- Will this option be adopted by expansion states? In states that have expanded Medicaid under the ACA, most postpartum women have a pathway to coverage – either Medicaid or subsidized private insurance through the ACA Marketplaces, but a longer postpartum period could allow for greater continuity with Medicaid providers. Studies have documented that new moms who have Medicaid funded childbirths experiencing significant churning in coverage.
- What will be the impact on federal and state budgets? The Congressional Budget Office (CBO) estimates that by 2024, about a quarter of postpartum beneficiaries will live in states that elect the new option. CBO estimates that extended Medicaid coverage will result in almost $6.1 billion in federal spending over the first ten years. States that adopt this extension would also incur costs as the extended coverage would remain at the same federal matching level, which ranges from 56.2% to 84.51%. These estimates take into account potential shifts in private insurance enrollment, including lower ACA subsidy costs. It is not clear if the estimates account for factors such as greater access to preventive services like contraception, which could avert unintended pregnancies that would otherwise be covered by Medicaid.
- What will be the impact on health outcomes? Part of the motivation for postpartum extension is the nation’s high rate of preventable pregnancy-related mortality and morbidity, particularly the stark disparities among Black and Native American women. There is also growing recognition that the postpartum period extends far beyond 60 days. Many of the conditions that account for a significant share of pregnancy-related mortality and morbidity, such as cardiovascular diseases, hypertension, and depression often require care over a longer-term. Providing Medicaid access to low-income mothers for a longer period also promotes continuity and access to preventive services such as contraception and intrapartum care.
–
The role of coverage as a key element of reproductive health care access is well understood. However, maternal health is also heavily connected to a complex set of issues, particularly poverty and systemic racism that pervade the health care system.