Data Note: Public Awareness Around Antibiotic Resistance
This data note examines the public’s knowledge and concerns about antibiotic resistance, a topic of increasing importance to both the United States and the wider global health community. The World Health Organization ranked antibiotic resistance as one of the top ten threats to global health for the year 2019, and the U.S. Centers for Disease Control and Prevention estimates that antibiotic resistance causes over 2 million infections and 23,000 deaths in the U.S. each year.1,2
- While a majority of the public say they have heard of antibiotic resistance and know what it means (71 percent) and most think the overuse of antibiotics is a major problem (53 percent), public knowledge of the issue is mixed. For example, while three-quarters are aware that bacterial infections can usually be cured with antibiotics, over half either incorrectly say that viral infections can be cured using antibiotics (27 percent) or that they do not know enough to say (28 percent).
- Although the opioid epidemic ranks as the top public health concern among Americans, about one-third of the public says they are “very worried” about the impacts of antibiotic resistance in this country, and about a quarter says they are “very worried” about the impacts of it on them and their family.
- Most of the public are aware of the possible negative implications of the overuse of antibiotics with two-thirds (67 percent) saying they are aware that the overuse of antibiotics will lead to people having to take stronger medications and about six in ten saying it will lead to longer lasting and more dangerous bacterial infections (63 percent) and an increasing number of bacteria resistant to antibiotics (62 percent). Yet, less than half of the public (39 percent) are aware that antibiotic resistance is unrelated to the outbreak of viruses such as measles.
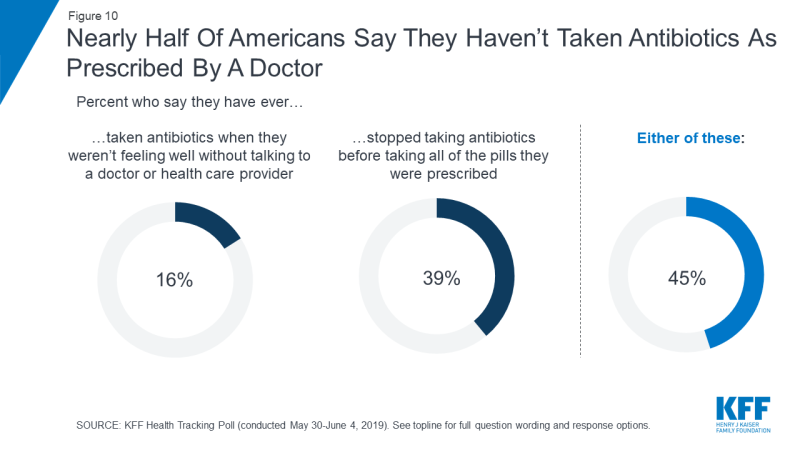
- Nearly half of adults (45 percent) say they have personally not taken their antibiotics as prescribed by a doctor – one of the leading causes of antibiotic resistance. However, when it comes to who has responsibility for fixing the problem of antibiotic resistance, larger shares place responsibility on drug companies and health care providers than on patients.
Public Awareness of Antibiotic Resistance
This data note examines the public’s knowledge and concerns about antibiotic resistance and also gauges the public’s experiences using antibiotics and their interactions with doctor and health care providers. The data for this analysis comes from the June 2019 KFF Health Tracking Poll.
Most Americans say that they have heard various terms used to talk about the issue of the overuse of antibiotics including antibiotic resistance and superbugs. Seven in ten (71 percent) say they have heard of the term “antibiotic resistance” and know what it means, while an additional one in seven say that they have heard of the term but are unsure what it means (14 percent). A similar share (15 percent) say they have never heard of antibiotic resistance. A smaller share, but still a majority (55 percent), say that they have heard the term “superbugs” and know what it means. By comparison, fewer (49 percent) say they know the meaning of the term “anti-vaxxers” (individuals who are opposed to vaccinations), another public health concern that has been in the news recently.
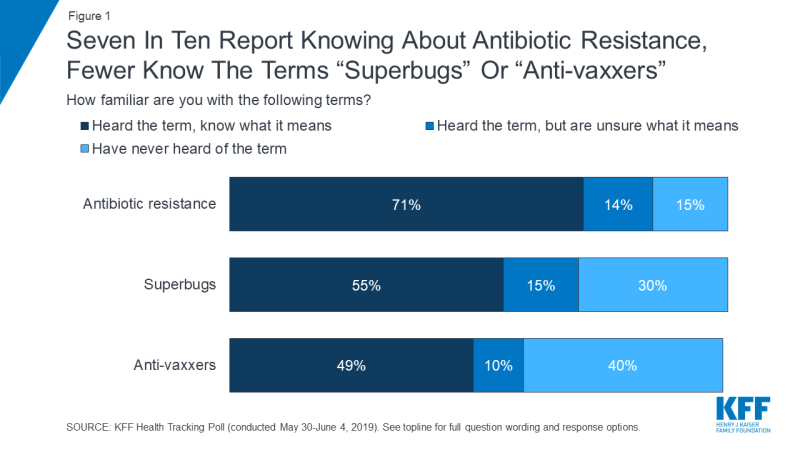
Figure 1: Seven In Ten Report Knowing About Antibiotic Resistance, Fewer Know The Terms “Superbugs” Or “Anti-vaxxers”
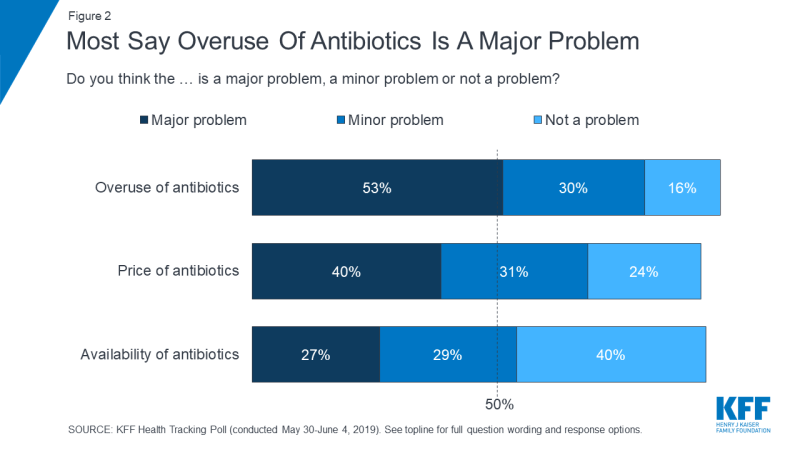
In addition to knowing the term, a majority of the public also believe the overuse of antibiotics is a problem. Half of the public (53 percent) says the overuse of antibiotics is a “major problem” while an additional three in ten say it is a “minor problem.” Smaller shares of the public say the same about the price of antibiotics (40 percent say it is a “major problem” while 31 percent say it is a “minor problem”) or the availability of antibiotics (27 percent and 29 percent, respectively).
While large shares of the public say the overuse of antibiotics is a problem, concerns about the opioid epidemic outrank antibiotic resistance on a list of several public health problems facing the nation at large. Eight in ten (82 percent) report feeling worried about the opioid epidemic, compared to nearly three-fourths who feel worried about outbreaks of preventable diseases like measles and whooping cough (73 percent) or about antibiotic resistance (72 percent). Fewer, about six in ten (63 percent), are worried about global health epidemics like Zika or Ebola.
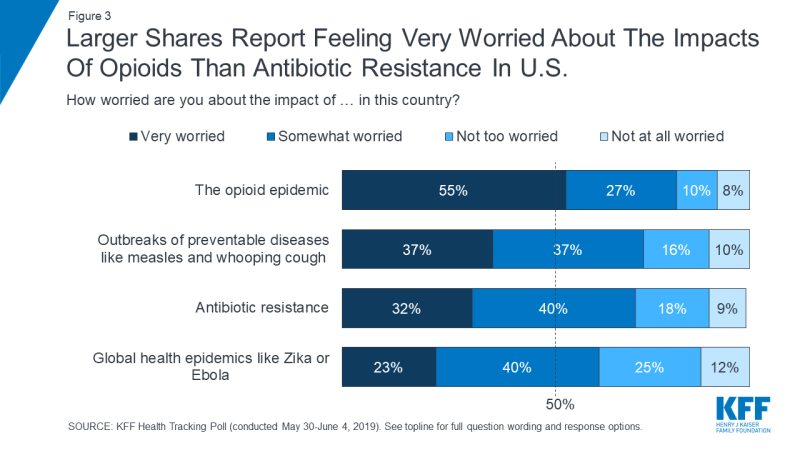
Figure 3: Larger Shares Report Feeling Very Worried About The Impacts Of Opioids Than Antibiotic Resistance In U.S.
When asked about the same problems affecting them and their family, the opioid epidemic ranks among the top worries, but at least half of the public says they are “very worried” or “somewhat worried” about each of these problems affecting them and their family, including six in ten (59 percent) who say they are worried about personally being affected by antibiotic resistance.
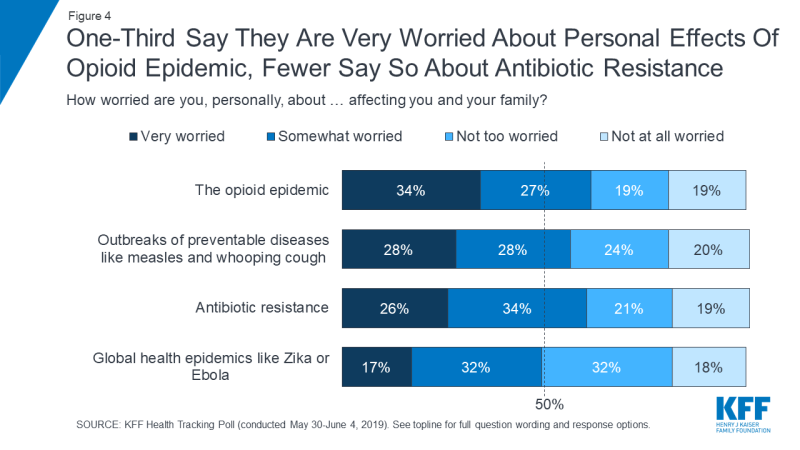
Figure 4: One-Third Say They Are Very Worried About Personal Effects Of Opioid Epidemic, Fewer Say So About Antibiotic Resistance
Public Knowledge On Appropriate Use Of Antibiotics and the Effects Of Antibiotic Overuse
While a majority of the public say they have heard of antibiotic resistance and know what it means (71 percent) and most think the overuse of antibiotics is a major problem (53 percent), public knowledge of the issue is mixed. While the public is mostly aware that antibiotics can help cure bacterial infections (75 percent), this month’s poll indicates there are common misconceptions about what illnesses warrant the use of antibiotic medications. For example, over half (55 percent) say that viral infections can either be cured using antibiotics (27 percent) or that “they do not know enough to say” (28 percent), and nearly half (47 percent) either say the flu can be cured by taking antibiotics (26 percent), or that “they do not know enough to say” (21 percent). When asked about pneumonia, 53 percent say this can be cured by taking antibiotics, but one in ten say it cannot be cured by taking antibiotics and about a third (36 percent) say that “they do not know enough to say.” While some forms of pneumonia are viral and cannot be treated with antibiotics, the most common form of pneumonia is bacterial and can be treated with these medications.
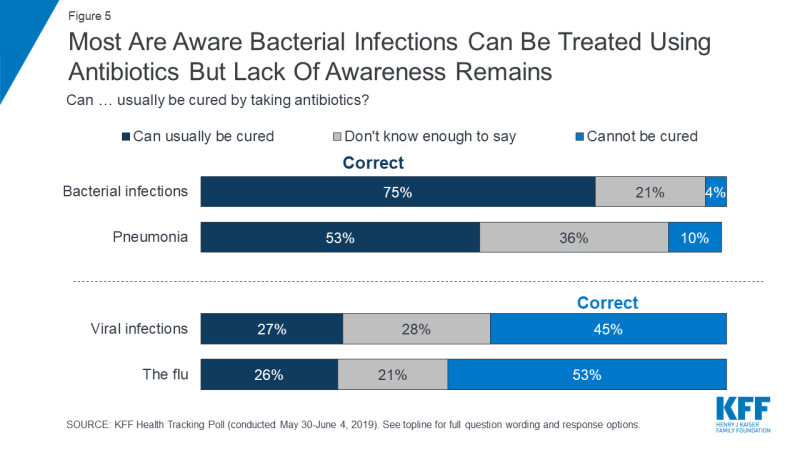
Figure 5: Most Are Aware Bacterial Infections Can Be Treated Using Antibiotics But Lack Of Awareness Remains
Knowledge about which illnesses can usually be cured by taking antibiotics varies based on certain demographic characteristics. For example, while over half of women (54 percent) are aware that viral infections cannot be cured with antibiotics, two-thirds of men either incorrectly think antibiotics can cure these infections (30 percent) or say they don’t know enough to say (34 percent). Adults ages 18-64 are also somewhat more likely to answer this question correctly than those ages 65 and older (47 percent vs 38 percent, respectively). Adults with higher income and higher levels of education are also more likely to be aware that antibiotics are not effective at treating viral infections, with majorities of adults with at least a college education (65 percent) and adults with incomes of at least $90,000 (62 percent) knowing this. By contrast, about three-fourths of adults with a high school diploma or less and seven in ten (69 percent) of those with household incomes less than $40,000 either believe antibiotics can cure viral infections or say they don’t know enough to say.
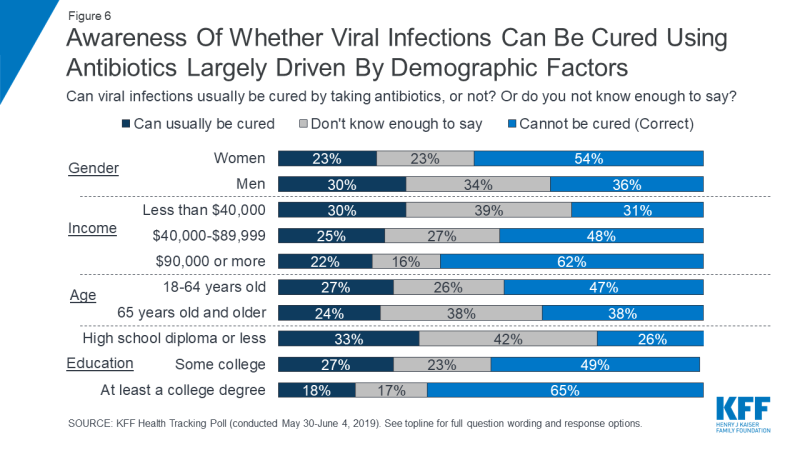
Figure 6: Awareness Of Whether Viral Infections Can Be Cured Using Antibiotics Largely Driven By Demographic Factors
Most of the public are aware of the possible negative implications of the overuse of antibiotics. Two-thirds (67 percent) say they are aware that the overuse of antibiotics will lead to people having to take stronger medications for previously easy-to-treat infections. Similarly, majorities are aware that the overuse of antibiotics will lead to bacterial infections lasting longer and becoming more dangerous (63 percent), an increasing number of superbugs or bacteria resistant to antibiotics (62 percent), as well as increasing costs for treating bacterial infections (57 percent). Roughly half (53 percent) say they know that at-risk groups like infants and seniors getting more life-threatening illnesses may result from the overuse of antibiotics. However, across the board, between a third and nearly half of Americans say overuse of antibiotics will not lead to these consequences, or that that they do not know enough to say.
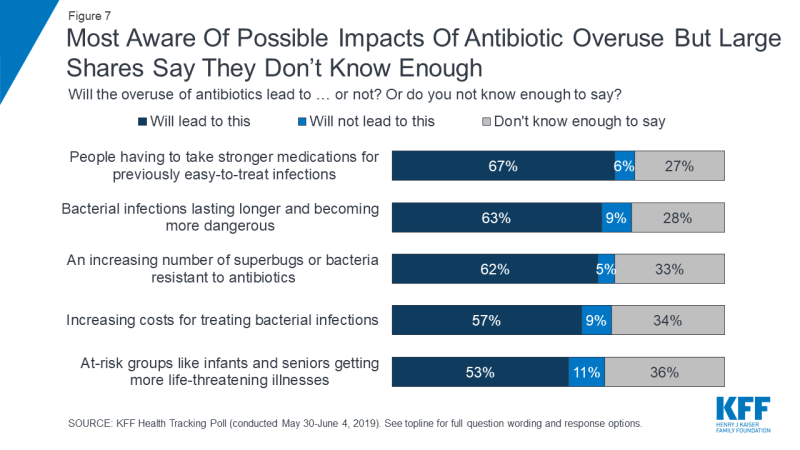
Figure 7: Most Aware Of Possible Impacts Of Antibiotic Overuse But Large Shares Say They Don’t Know Enough
Although many in the public are aware of the possible consequences of antibiotic overuse, some confusion remains. About six in ten (61 percent) either incorrectly say that measles or other contagious viruses will spread due to the overuse of such medications (26 percent) or say that they do not know enough to say whether this will happen (35 percent).
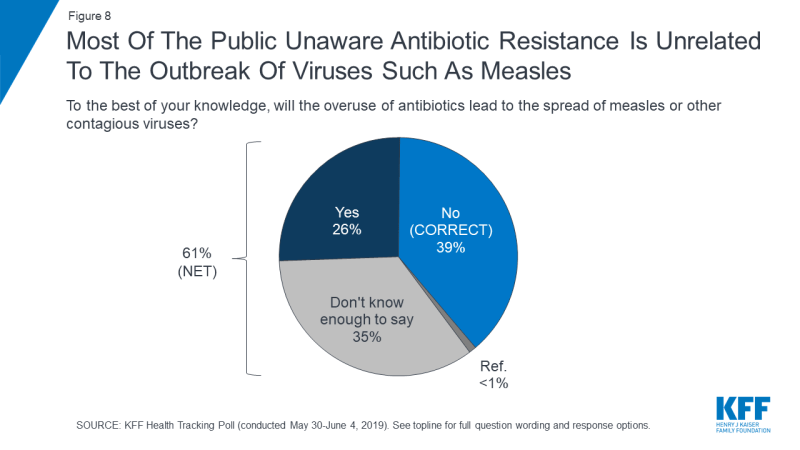
Figure 8: Most Of The Public Unaware Antibiotic Resistance Is Unrelated To The Outbreak Of Viruses Such As Measles
When asked who bears responsibility for fixing the problem of antibiotic resistance, a larger share of the public place the responsibility on drug companies and health care providers than on any other entity, including patients. A majority of the public says that drug and pharmaceutical companies (59 percent) and doctors or health care providers (56 percent) are “very responsible.” Less than half say the same about the federal government (38 percent), patients (30 percent), or the agriculture and farming industry (20 percent).
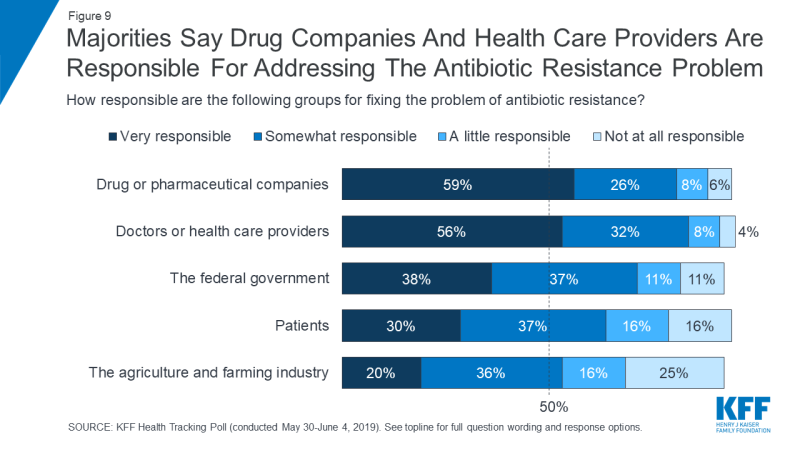
Figure 9: Majorities Say Drug Companies And Health Care Providers Are Responsible For Addressing The Antibiotic Resistance Problem
The Public’s Experiences With Antibiotics
Nearly half of the public (45 percent) report they have ever either taken antibiotics when they weren’t feeling well without talking to a doctor or health care provider (16 percent), or stopped their course of antibiotics before it was finished (39 percent). This experience differs based on certain demographic characteristics. Adults ages 18-64 are more likely than adults ages 65 and older to report having made decisions about their antibiotic medication without consulting a doctor (48 percent vs 32 percent, respectively). Additionally, adults without a college education are more likely than adults with a college education to say they have done either of these things (48 percent vs 39 percent, respectively).
| Table 1: Experiences Making Antibiotic Decisions Without Consulting A Doctor By Age And Education | |||||
| Percent who say: | Total | Age | Education | ||
| Ages 18–64 | Ages 65+ | Less than College | College education or more | ||
| They have ever taken antibiotics when they weren’t feeling well without talking to a doctor or health care provider | 16% | 17% | 9% | 16% | 14% |
| They have ever stopped taking antibiotics before taking all of the pills they were prescribed | 39 | 42 | 28 | 42 | 33 |
| Yes to any of the above | 45 | 48 | 32 | 48 | 39 |
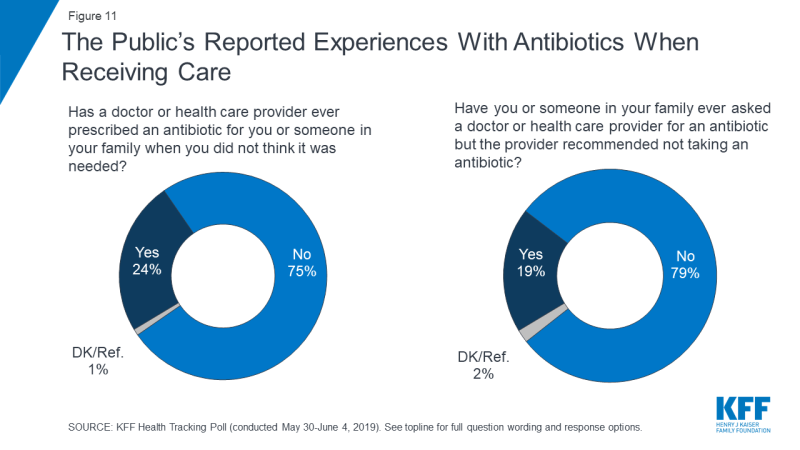
The data also indicates that it is not uncommon for patients to receive antibiotics that they don’t believe are necessary, and on the other hand, to have their requests for an antibiotic denied by a health professional. About a quarter of Americans (24 percent) say that there was a time when a health care provider prescribed an antibiotic for them or someone in their family when they did not think it was needed. Additionally, about one in five (19 percent) say that they or someone in their family has ever asked a provider for an antibiotic but the provider recommended not taking one.