Mental Health
Access and coverage
Mental Health Parity at a Crossroads
More than 25 years after the first federal mental health parity protections were put in place, adequate coverage for behavioral health care remains elusive. This brief explains the federal behavioral health parity requirements and sets out key policy issues.Section 1115 Waiver Watch: Contingency Management
Of the 800,000 Medicaid enrollees aged 12 to 64 with a diagnosed stimulant use disorder in 2019, about 20% were in states that now have approved 1115 Medicaid waivers for contingency management services (California, Delaware, Montana, Washington).
Mental Health Findings from 2022 Women’s Health Survey
This issue brief focuses on the access and coverage of mental health services using data from the 2022 KFF Women’s Health Survey.5 Key Facts about Medicaid Coverage for Adults with Mental Illness
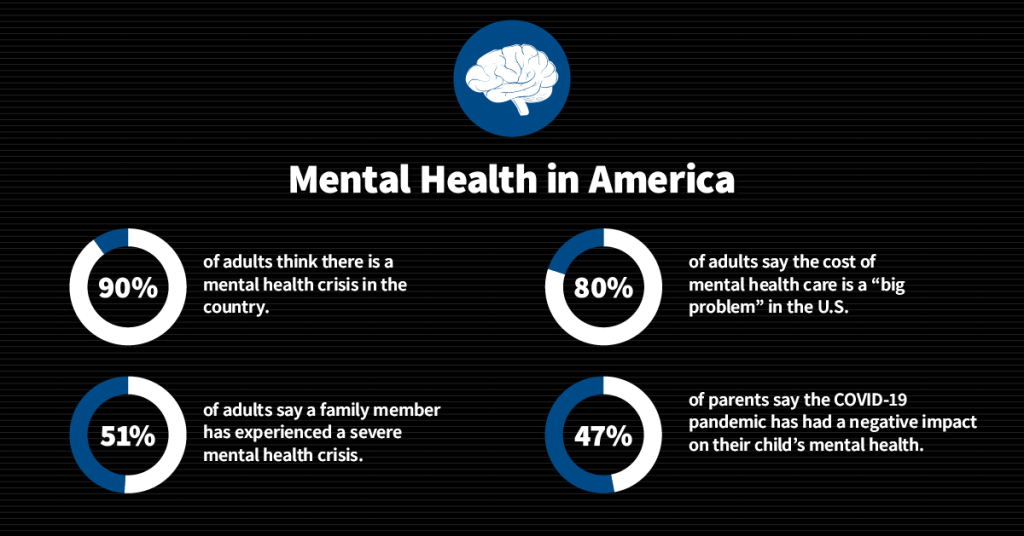
Nationwide, an estimated 52 million nonelderly adults live with mental illness, and Medicaid covers nearly one in three (29%) of them, or about 15 million adults.Examining New Medicaid Resources to Expand School-Based Behavioral Health Services
How does the recent guidance from CMS increase access to behavioral health care services in schools? KFF explores implementation of provisions from the Safer Communities Act of 2022.
Latest News
-

On Autism, Kennedy Turns Against Science and Reality
-

Covid Worsened Shortages of Doctors and Nurses. Five Years On, Rural Hospitals Still Struggle.
-
KFF Health News' 'What the Health?': On Autism, It’s the Secretary’s Word vs. the CDC’s
-

A Call for Comfort Brought the Police Instead. Now the Solution Is in Danger.