The independent source for health policy research, polling, and news.
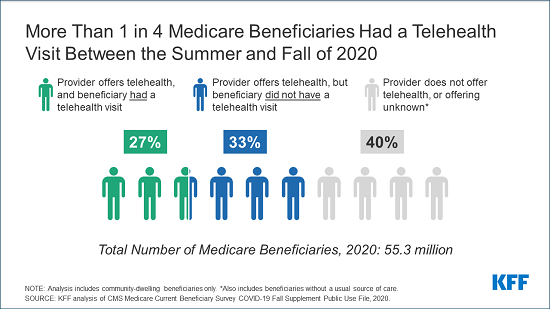
More Than 1 in 4 Medicare Beneficiaries Had a Telehealth Visit Between the Summer and Fall of 2020
Over Half Who Had a Telehealth Visit Used Only a Telephone
As the coronavirus pandemic kept people home last year, just over 1 in 4 Medicare beneficiaries had a telehealth visit with a doctor or other health professional between the summer and fall of 2020, a new KFF analysis finds.
Once limited to beneficiaries living in rural areas, coverage of telehealth services by traditional Medicare has undergone rapid expansion during the pandemic, with new options including allowing some services to be provided via audio-only telephone. Medicare Advantage plans have been able to offer additional telehealth benefits not covered by traditional Medicare outside of the public health emergency, and virtually all do. However, coverage of telehealth services under traditional Medicare would revert to the more limited availability when the public health emergency ends without a change in current rules.
The new analysis provides an overview of the pandemic-driven changes to Medicare’s coverage of telehealth, examines community-dwelling beneficiaries’ use of telehealth services, and discusses issues related to extending telehealth coverage under traditional Medicare beyond the public health emergency.
The new analysis provides an overview of the pandemic-driven changes to Medicare’s coverage of telehealth, examines community-dwelling beneficiaries’ use of telehealth services, and discusses issues related to extending telehealth coverage under traditional Medicare beyond the public health emergency.
The new analysis provides an overview of the pandemic-driven changes to Medicare’s coverage of telehealth, examines community-dwelling beneficiaries’ use of telehealth services, and discusses issues related to extending telehealth coverage under traditional Medicare beyond the public health emergency.
Among the key findings:
• Nearly two-thirds (64%, or 33.6 million) of Medicare beneficiaries with a usual source of care say that their provider currently offers telehealth appointments, up from 18% who said their provider offered telehealth before the pandemic. However, nearly a quarter (23%) of Medicare beneficiaries do not know if their provider offers telehealth appointments, and this share is larger among rural beneficiaries (30%).
• Among Medicare beneficiaries who said their provider offers telehealth, some groups of beneficiaries were more likely than others to report having a telehealth visit with a doctor or other health professional, including Medicare beneficiaries under age 65 with long-term disabilities, Black and Hispanic beneficiaries, Medicare beneficiaries enrolled in both Medicare and Medicaid, and beneficiaries with multiple chronic conditions. At the same time, there was no difference in reported rates of telehealth use between beneficiaries in traditional Medicare and Medicare Advantage.
• A majority (56%) of Medicare beneficiaries who had a telehealth visit report accessing care using only a telephone, while a smaller share had a telehealth visit via video (28%) or both video and telephone (16%).
A number of telehealth-related bills have been introduced in the 117th Congress, including proposals to make permanent the telehealth expansions provided during the public health emergency, expand Medicare coverage of mental health services, and expand the scope of providers eligible for payment for telehealth services covered by Medicare. Other bills are aimed at assessing the impact of expanded telehealth services on the quality of patient care and program spending.
For more data and analyses on telehealth and the pandemic, visit kff.org.