
The independent source for health policy research, polling, and news.
Medicare Advantage Plans Denied a Larger Share of Prior Authorization Requests in 2022 Than in Prior Years
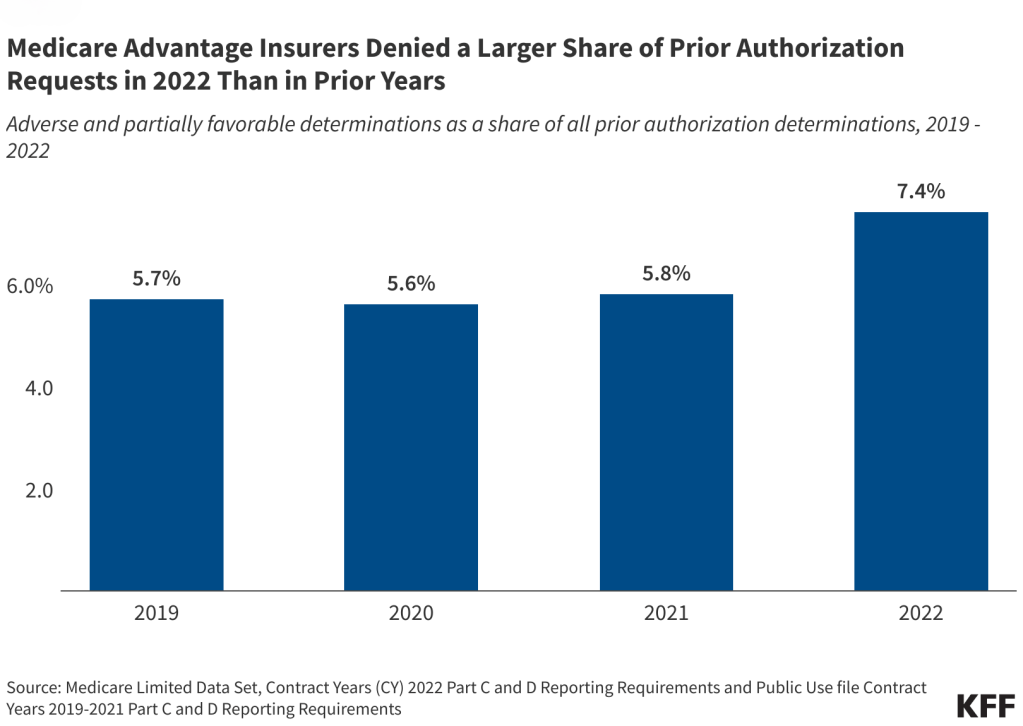
Medicare Advantage plans denied 3.4 million prior authorization requests for health care services in whole or in part in 2022, or 7.4% of the 46.2 million requests submitted on behalf of enrollees that year, according to a new KFF analysis of federal data.
That was a higher share of denials than in recent years. The share of all prior authorization requests denied by Medicare Advantage plans increased from 5.7% in 2019, 5.6% in 2020 and 5.8% in 2021.
Prior authorization is intended to ensure that health care services are medically necessary by requiring providers to obtain approval before a service or other benefit is covered. While prior authorization has long been used to contain spending and prevent people from receiving unnecessary or low-value services, it also has been subject to criticism that it may create barriers to receiving necessary care. (Traditional Medicare does not require prior authorization except for a limited set of services.)
Prior authorization practices have attracted the attention of the Biden Administration and lawmakers in Congress. The administration recently finalized rules to increase the timeliness and transparency of prior authorization decisions and require Medicare Advantage plans to evaluate the effect of prior authorization policies on people with certain social risk factors. Lawmakers have introduced bills to codify many of these changes into law.
Other key takeaways from the KFF analysis include:
- Just one in 10 (9.9%) prior authorization requests that were denied were appealed in 2022. That represents an increase since 2019, when 7.5% of denied prior authorization requests were appealed.
- The vast majority of appeals (83.2%) in 2022 resulted in overturning the initial decision, similar to the shares overturned and in each year between 2019 and 2021.
- Patients may have different experiences depending on the Medicare Advantage plan in which they are enrolled. The volume of prior authorization determinations varied across Medicare Advantage insurers, as did the share of requests that were denied, the share of denials that were appealed, and the share of decisions that were overturned upon appeal.
Two other KFF analyses released today also examine the latest data about Medicare Advantage.
- The first provides information and trends about current Medicare Advantage enrollment, by plan type and firm, and by state and county. It shows that in 2024, more than half (54%) of eligible Medicare beneficiaries are enrolled in Medicare Advantage. The share of beneficiaries in Medicare Advantage plans varies across states ranging from 2% in Alaska to 63% in Alabama, Connecticut and Michigan. Medicare Advantage enrollment is highly concentrated among a small number of firms, with UnitedHealthcare and Humana accounting for nearly half (47%) of all Medicare Advantage enrollment nationwide.
- The second companion analysis describes Medicare Advantage premiums, out-of-pocket limits, supplemental benefits offered, and prior authorization requirements. In 2024, three quarters (75%) of enrollees in individual Medicare Advantage plans with prescription drug coverage pay no premium other than the Medicare Part B premium, which is a big selling point for many beneficiaries. Most Medicare Advantage enrollees are in plans that offer supplemental benefits not covered by traditional Medicare, such as vision, hearing and dental. And nearly all Medicare Advantage enrollees (99%) are in plans that require prior authorization for some services.