
The independent source for health policy research, polling, and news.
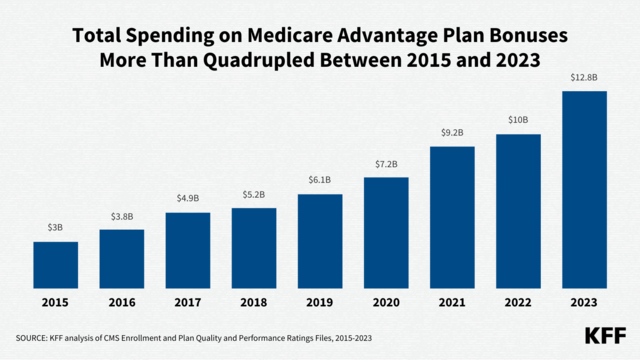
Medicare Advantage Insurers Will Collect at Least $12.8 Billion in Federal Bonus Payments in 2023—a Nearly 30% Increase from 2022
New KFF Analyses Highlight Trends in Enrollment, Benefits and Cost-Sharing, and Bonus Payments for Medicare Advantage Plans
Federal spending on bonus payments to insurance companies that offer Medicare Advantage plans will reach at least $12.8 billion in 2023, according to a new KFF analysis. That is a nearly 30% increase from 2022, and more than quadruple the spending in 2015.
These data come from one of three analyses released today by KFF that examine various facets of the Medicare Advantage program, which provides health insurance coverage to nearly 31 million Americans. KFF examined trends in enrollment, premiums, out-of-pocket limits, cost sharing, supplemental benefits, prior authorization, star ratings and bonus payments.
Bonus payments, which were established by the Affordable Care Act, are based on a five-star rating system and are intended to encourage Medicare Advantage plans to compete for enrollees based on quality. The payments vary substantially across firms, with UnitedHealthcare receiving the largest total payments ($3.9 billion) and Kaiser Permanente the highest payment per enrollee ($523).
Eighty-five percent of Medicare Advantage enrollees are in plans that are receiving bonus payments in 2023. The impact of star ratings on bonus payments lags a year, and several policies in place during the COVID-19 Public Health Emergency have expired, reducing 2023 star ratings relative to 2022, which will likely lead to a smaller share of enrollees in plans that receive bonuses in the 2024 plan year.
Enrollment in Medicare Advantage in 2023 comprises more than 51% of the eligible Medicare population — more than twice the share enrolled in 2007 (19%), as noted in a companion analysis that provides the latest information about Medicare Advantage enrollment, by plan type and firm, and shows how enrollment varies by state and county.
Enrollment continues to be highly concentrated among a handful of firms, with UnitedHealthcare (29%) followed by Humana (18%), comprising nearly half of all Medicare Advantage enrollees nationwide, according to the analysis. Blue Cross Blue Shield (BCBS) affiliates (including Anthem BCBS plans) account for another 14%. And four other firms (CVS Health, Kaiser Permanente, Centene, and Cigna) account for another 23%.
Additional research released by KFF today shows that 73% of Medicare Advantage enrollees are in plans with prescription drug coverage (MA-PDs) that require no premium other than the Medicare Part B premium. KFF also documents that the vast majority of enrollees in Medicare Advantage plans have access to some benefits not covered by traditional Medicare, such as eye exams and/or glasses, hearing exams and/or aids, a fitness benefit, dental care, and reduced cost-sharing.
Plans are able to offer these extra benefits, often for no additional premium, largely due to the current Medicare payment system that provides an additional $2,350 per enrollee above plans’ estimated costs of providing Medicare-covered services, on average.
One tradeoff of enrolling in Medicare Advantage is that many plans routinely require patients to obtain prior authorization for services. Virtually all Medicare Advantage enrollees (99%) are in plans that require authorization for some services, according to the analysis.
For more information, please visit: