The independent source for health policy research, polling, and news.
A Small Share of People with Medicare Advantage or Stand-alone Medicare Part D Coverage Voluntarily Switch Plans During Open Enrollment
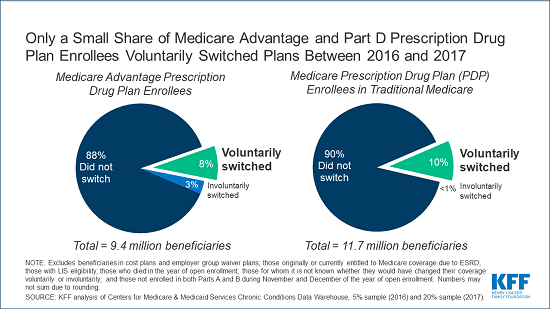
A new KFF analysis finds that a relatively small share of people with Medicare Advantage or stand-alone Medicare Part D prescription drug coverage voluntarily switch plans during Medicare’s open enrollment period, which runs annually from Oct. 15 to Dec. 7.
With less than a week remaining for beneficiaries to make their selections, shopping around among plans is important, since plans can vary significantly and change from year to year, which can have a large impact on enrollees’ coverage and costs.
The analysis finds that, among beneficiaries without low-income subsidies, 8 percent of those in Medicare Advantage plans with prescription drug coverage voluntarily switched to another plan during the 2016 open enrollment period for the 2017 plan year. Similarly, only 10 percent of beneficiaries without low-income subsidies in Part D stand-alone drug plans voluntarily switched to another plan during the 2016 open enrollment period.
The data reflect a longstanding pattern where a substantial majority of Medicare’s private plan enrollees don’t choose to switch plans in any given year. During each of the open enrollment periods between 2007 and 2016, the share of enrollees without low-income subsidies voluntarily switching plans for the coming year ranged between 6 and 11 percent for people in Medicare Advantage drug plans, and between 10 and 13 percent among those in stand-alone drug plans.
According to an analysis of data from the Centers for Medicare & Medicaid Services (CMS), one-third of Medicare beneficiaries living in the community said it was very difficult or somewhat difficult to compare Medicare options in 2017, while nearly half said they rarely or never review or compare their Medicare options.
Low rates of plan switching could indicate that many beneficiaries are generally satisfied with their current plan. Another explanation could be that many beneficiaries may find the process of comparing plans too challenging, are unaware of open enrollment, or have limited confidence in their ability to choose a better plan.
CMS encourages beneficiaries to shop around for plans each year to potentially save money or get new benefits. This is valuable advice, because private plans can vary significantly in premiums, deductibles and other cost sharing, provider and pharmacy networks, and drugs covered, among other features.