
The independent source for health policy research, polling, and news.
As Medicaid Unwinding Concludes in Most States, KFF Finds 25 Million Lost Medicaid Coverage but Enrollment is 10 Million Higher Than Pre-Pandemic Levels
Despite increases in Medicaid/CHIP enrollment overall in most states, 12 states saw child enrollment fall
Over 25 million people were disenrolled from Medicaid and over 56 million had their coverage renewed, according to KFF’s analysis of the outcomes of the Medicaid unwinding, which nearly all states have now completed.
Despite these millions of disenrollments, 10 million more people are currently enrolled in Medicaid and the Children’s Health Insurance Program (CHIP) nationally than at the start of the pandemic. Most states ended the unwinding with higher total Medicaid and CHIP enrollment than they began with in February 2020, including seven states where enrollment levels were at least 30% higher.
During the COVID-19 pandemic, states kept people continuously enrolled in Medicaid in exchange for enhanced federal funding, leading to record growth in Medicaid enrollment. After the continuous enrollment policy ended on March 31, 2023 and under the process referred to as “unwinding,” states were required to complete eligibility renewals for all Medicaid enrollees.
There have always been people eligible for Medicaid but not enrolled, as well as people who get dropped from Medicaid for failing to complete regular renewal processes. During the unwinding period, many states took steps to improve their renewal systems, leading to fewer people getting dropped even though they remain eligible. Five states — Missouri, Nebraska, North Carolina, Oklahoma, and South Dakota – have also adopted Medicaid expansion since the onset of the pandemic, and several states expanded eligibility for other groups, including children. The net effect is that Medicaid enrollment is higher than it was before the pandemic.
However, enrollment among children has nearly returned to pre-pandemic levels (at only five percent higher.) Twelve states saw drops in child enrollment and three states saw enrollment fall for both children and adults relative to pre-pandemic levels.
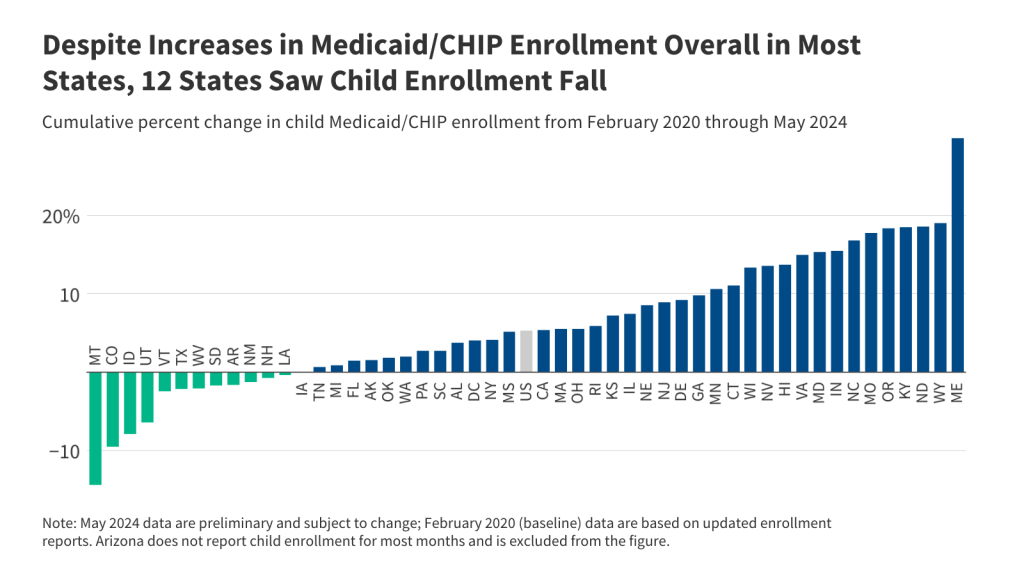
Because Medicaid eligibility levels are more generous for children, these drops in child enrollment – coupled with an increase in the 2023 child uninsured rate – suggest some children may have lost coverage despite being eligible.
Overall, 31% of people whose Medicaid coverage was redetermined during the unwinding were disenrolled, with wide differences across states. Five states had disenrollment rates of more than 50% (Montana, Utah, Idaho, Oklahoma, and Texas), while five states had rates under 20% (North Carolina, Maine, Oregon, California, and Connecticut).
This analysis marks the end of KFF’s independent effort to monitor the Medicaid unwinding using state and federal data. Going forward, the KFF Medicaid Enrollment and Unwinding Tracker will use data from the Centers for Medicare and Medicaid Services to track monthly Medicaid enrollment.