The independent source for health policy research, polling, and news.
50-State Survey Finds States Have Upgraded Medicaid Enrollment and Eligibility Systems and Begun Resolving Initial ACA Implementation Issues, Although Challenges Remain
Over its first two years, the Affordable Care Act (ACA) has triggered increases in Medicaid eligibility levels and upgrades in states’ Medicaid eligibility and enrollment systems, making it easier for individuals to enroll in Medicaid and producing faster eligibility decisions, according to a new Kaiser Family Foundation survey of Medicaid and Children’s Health Insurance Program eligibility levels and enrollment, renewal and cost-sharing policies.
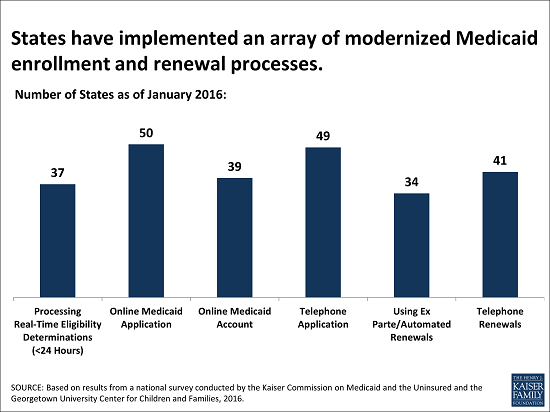
The 14th annual 50-state survey, conducted by the Foundation’s Kaiser Commission on Medicaid and the Uninsured and Georgetown University’s Center for Children and Families, finds that as of January 2016, many states have revised enrollment and renewal processes in accord with the ACA (Chart). Online applications are now standard in virtually all states. Notably, 37 states can make Medicaid eligibility determinations for low-income children, pregnant women, and non-disabled adults within 24 hours.
The survey also shows that, in 2015, states began resolving many of the challenges they faced when the new systems and processes were first launched in 2014. After many states postponed renewals and delayed implementing new renewal procedures during 2014, states took up this task in 2015. As of January 2016, 47 states are up to date processing Medicaid renewals and 34 states can process automated renewals using information from electronic data sources. Moreover, coordination between state Medicaid agencies and marketplaces improved in 2015. Nearly all of the 38 states that rely on the Federally-Facilitated Marketplace (FFM), healthcare.gov, for marketplace eligibility and enrollment functions can send and receive electronic data transfers between the state Medicaid agency and Marketplace. However, 20 states are still reporting they are having problems or delays with the transfers, although the scope of these problems varies.
These higher-functioning systems and processes are helping states to enroll more eligible low-income people in Medicaid, keep eligible individuals enrolled, reduce paperwork burdens on people and program administrators, and are contributing to increased administrative efficiencies. They also are providing new tools to support program management, such as increased data reporting.
In addition, the survey report, Medicaid and CHIP Eligibility, Enrollment, Renewal, and Cost Sharing Policies as of January 2016: Findings from a 50-State Survey, provides 2016 eligibility levels in all 50 states and the District of Columbia for children, pregnant women and non-disabled adults in Medicaid and CHIP. Eligibility levels vary significantly across groups and by state, as well as by state Medicaid expansion status.
These and other findings from the survey were discussed today at a public briefing at the Foundation’s Washington, D.C. offices. An archived webcast of the briefing, as well as copies of presentation slides and other materials, will be available on kff.org later today. Also available is an updated issue brief, Trends in Medicaid and CHIP Eligibility Over Time.