Medicaid Enrollment & Spending Growth: FY 2016 & 2017
For FY 2016 and FY 2017, national Medicaid enrollment and total spending continue to grow, but much more slowly after high growth in FY 2015 primarily due to the implementation of the Medicaid expansion in the Affordable Care Act. This brief discusses these trends based on interviews and data provided by state Medicaid directors as part of the 16th annual survey of Medicaid directors in all 50 states and the District of Columbia. Conducted by the Kaiser Commission on Medicaid and the Uninsured (KCMU) and Health Management Associates (HMA), the survey focuses on trends and Medicaid policy actions taken by states in FY 2016 and FY 2017. Key findings are described below and provided in a companion report.
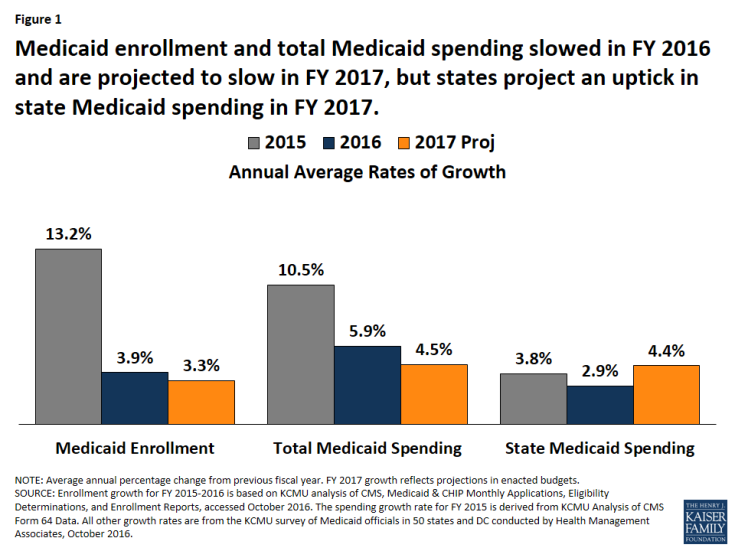
Figure 1: Medicaid enrollment and total Medicaid spending slowed in FY 2016 and are projected to slow in FY 2017, but states project an uptick in state Medicaid spending in FY 2017.
Enrollment and Total Spending. Following significant increases in FY 2015 related to the implementation of the Affordable Care Act (ACA), Medicaid enrollment and total spending growth slowed substantially in FY 2016 and FY 2017 as ACA related enrollment tapered (Figure 1). Medicaid officials identified the high costs of specialty drugs and payment increases for specific provider groups as upward pressures on spending. Slower state revenue growth in FY 2017 added pressure on states to control Medicaid costs.
State Medicaid Spending. Adopted budgets for FY 2017 project an uptick in state Medicaid spending primarily due to the phase-down in the federal share for the expansion population from 100 percent to 95 percent. In FY 2017, state Medicaid spending and total Medicaid spending are projected to grow at the same pace. Eight of the Medicaid expansion states (Arkansas, Arizona, Colorado, Illinois, Indiana, Louisiana, New Hampshire, and Ohio) reported plans to use provider taxes or fees to fund all or part of the state share of costs of the ACA Medicaid expansion.
Looking Ahead. Since 2014, an improving economy and the implementation of the ACA have been the primary drivers of Medicaid enrollment and spending trends. Going forward, ACA-related enrollment is expected to stabilize and trends will be influenced more by the economy, upward spending pressures like rising prescription drug costs, and state policy actions. In addition, federal and state elections will have implications for state decisions about whether to implement the ACA and for the future of the ACA more broadly.


