Medicaid Long-Term Services and Supports: An Overview of Funding Authorities
Medicaid is the primary payer for long-term services and supports (LTSS) for four million Americans – children, adults, and seniors – who experience difficulty living independently and completing daily self-care activities as a result of cognitive disabilities, physical impairments, and/or disabling chronic conditions. Medicaid LTSS are delivered in institutional settings (e.g., nursing facilities) and community-based settings (e.g., private homes). Due in large part to the growth in beneficiary demand for home and community-based services (HCBS) and states’ obligations under the U.S. Supreme Court’s Olmstead decision to provide services to persons with disabilities in community settings rather than institutions, Medicaid HCBS program enrollment and spending have been growing.1 With the aging of the “Baby Boom” generation into older adulthood and the growing need for LTSS, states and the federal government will continue to be challenged to increase access to HCBS while improving service delivery, managing costs, and maintaining beneficiary protections and autonomy.
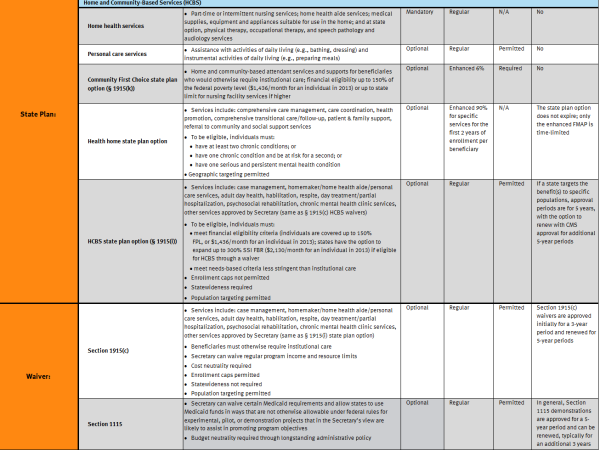
States provide Medicaid LTSS under state plan, waiver, and other authorities. Whereas most HCBS are optional for states, nursing facility care is a mandatory Medicaid state plan service, with the result that states’ LTSS spending historically has been skewed in favor of institutional care. States have been working to rebalance their LTSS spending and can expand HCBS through waivers and options newly established and expanded by the Affordable Care Act; incentives for states to expand the range of HCBS include enhanced federal funding, flexibility in setting financial eligibility levels and needs based criteria, and population targeting. However, navigating the various Medicaid HCBS options and coordinating new options with existing HCBS programs can present administrative complexities for states. In addition, two of the optional provisions – the Balancing Incentive Program and the Money Follows the Person demonstration – are set to expire in 2015 and 2016, respectively, limiting the amount of time that states have to take advantage of these options. This fact sheet summarizes the various Medicaid LTSS provisions by funding authority (See Table 1).
A companion paper, Key Issues in State Implementation of the New and Expanded Home and Community-Based Services Options Available Under the Affordable Care Act, summarizes insights from federal and state officials and experts on state adoption of the ACA HCBS options.2 For more information on state take-up of the ACA LTSS options, please see How is the Affordable Care Act Leading to Changes in Medicaid Long-Term Services and Supports (LTSS) Today? State Adoption of Six LTSS Options.3
Endnotes
- For state-level participant and expenditure data, see Kaiser Commission on Medicaid and the Uninsured, Medicaid Home and Community-Based Services Programs: 2009 Data Update (December 2012), available at http://www.kff.org/medicaid/report/medicaid-home-and-community-based-service-programs/.
- Available at http://www.kff.org/medicaid/issue-brief/key-issues-in-state-implementation-of-the-new-and-expanded-home-and-community-based-services-options-available-under-the-affordable-care-act.
- Available at http://www.kff.org/medicaid/issue-brief/how-is-the-affordable-care-act-leading-to-changes-in-medicaid-long-term-services-and-supports-ltss-today-state-adoption-of-six-ltss-options/; updates are available on the Kaiser Family Foundation’s State Health Facts website, available at: http://www.kff.org/state-category/health-reform/