Coverage and Care Pathways for People with HIV: A New Baseline
Introduction
This new baseline provides a snapshot of access to care and coverage for people with HIV today and serves as marker for gauging changes going forward. It reflects coverage gains associated with the Affordable Care Act’s (ACA) expansions as well as access through traditional insurance pathways and the Ryan White program.
People with HIV saw significant gains in insurance coverage under the healthcare law,1 through Medicaid expansion, the creation of health insurance marketplaces, and the elimination of insurance barriers, including pre-existing condition exclusions. At the same time, many continue to rely on the traditional Medicaid program, as well as the Ryan White HIV/AIDS program, the nation’s safety net for people with HIV who are underinsured and uninsured. In addition, even with the ACA’s expansions, state decisions have resulted in significant variation in access to coverage across the nation.
As debate over the future of the ACA continues, this baseline offers one tool for assessing changes made to the coverage landscape moving forward.
Methods
To develop the baseline, we identified eight state level variables across the three main pathways of coverage and access to care for people with HIV – Medicaid, private insurance/the marketplace, and Ryan White – and included data from all 50 states and DC. (See Table 1 for a list of all variables and the Appendix for a look at state-by-state status). While all eight variables are important, we further identified a subset of four variables, which, together, have the greatest bearing on access to care and coverage for people with HIV: Medicaid expansion status, Medicaid eligibility levels through the disability pathway, the average number of issuers per county in the state marketplace, and Ryan White ADAP eligibility level. We used these four variables to identify states that had “enhanced levels of access” for people with HIV. Below we provide findings for these four primary variables, followed by detailed findings across all measures.
| Table 1: Variables Examined by Coverage Category (4 Key Variables Discussed in Report Highlighted) |
||
| Medicaid | Marketplace | Ryan White/ADAP |
| Medicaid Expansion Status | Average No. of Issuers per County in State | ADAP Eligibility % FPL (Full Pay Rx) |
| Aged, Blind, Disabled Pathway Eligibility as % FPL | Total No. of Issuers in State | ADAP Eligibility % FPL (Insurance Program) |
| QHP Insurance Purchasing Status | ||
|
Part B Medical Services Eligibility |
||
Findings: The Current Coverage & Access Landscape
Enhanced Access
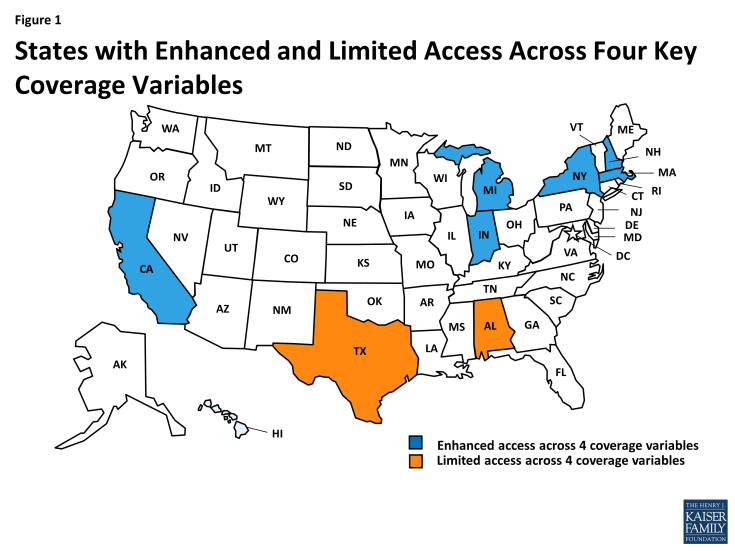
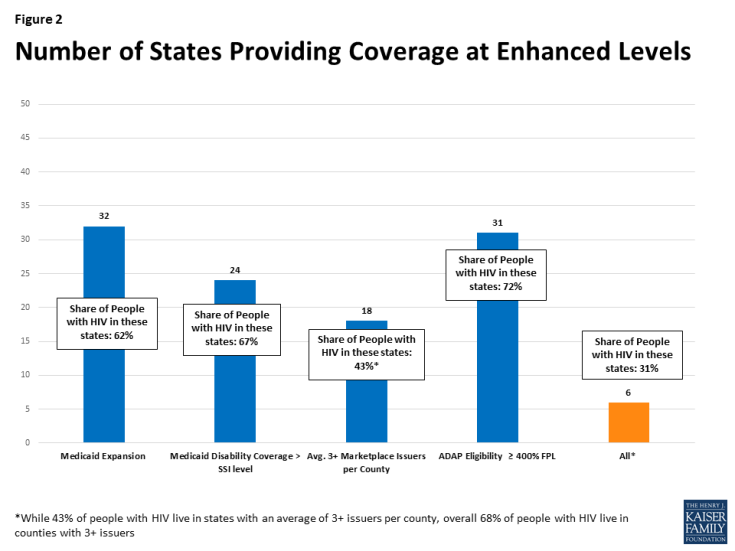
Looking across the four key variables, States were considered to have enhanced levels of access for people with HIV if they: had adopted the Medicaid expansion; offered traditional Medicaid disability coverage above the mandated SSI level (73% FPL); had an average of 3 or more issuers per county in their marketplace; and had an ADAP (medication assistance) eligibility level at or above 400% FPL. Six states (California, Indiana, Massachusetts, Michigan, New Hampshire, and New York) met all of these criteria; together, these six states account for one-third (31%) of all people living with HIV nationwide. None of these six is located in the Southern region of the U.S., a region that that faces significant access challenges and disparities.2 Looking at the two ACA-specific measures (Medicaid expansion and average number of issuers per county), 22 states met enhanced criteria, accounting for 52% of people with HIV. Two states (Alabama and Texas), accounting for 10% of the nation’s HIV prevalence, have the most limited access and did not meet any of these criteria. Looking at the four key variables, we found:
- 32 states, home to 62% of people with HIV, expanded their Medicaid programs.
- 24 states, home to 67% of people with HIV, offered Medicaid coverage through the disability pathway above the SSI level.
- 18 states, home to 43% of people with HIV, had an average of 3 or more issuers per county.
- 31 states, home to 72% of people with HIV, provided ADAP (medication assistance) eligibility at or above 400% FPL.
Few states, offered very limited or very robust coverage across all categories. More often, states offered some more expansive coverage across certain indicators and more limited coverage across others.
Medicaid
In assessing access to Medicaid, we look at two key pathways to coverage: the traditional program and the ACA’s Medicaid expansion. Prior to the ACA, to qualify for Medicaid enrollees were required to be both low income and “categorically eligible,” such as being disabled or pregnant. During this period, most people with HIV gained Medicaid coverage through the disability pathway, which in many cases meant developing AIDS before becoming eligible (despite it being a preventable diagnosis). The ACA addressed this by doing away with the categorical eligibility requirement and expanding access to individuals based on income alone. As such, access to Medicaid has grown significantly for people with HIV under the health law but as a result of a Supreme Court decision, some states have opted out of the expansion. For states that did not expand coverage, the disability pathway remains especially critical. Looking at the Medicaid measures, we find that:
- Medicaid expansion: Over half of states including DC (32) have adopted the ACA’s Medicaid expansion; 62% of people with HIV live in an expansion state. Nineteen states do not provide the Medicaid expansion pathway, affecting coverage opportunities for nearly 40% of people with HIV.
- Traditional disability pathway: Nearly half of states (24) provide Medicaid coverage through the disability pathway above the federally mandated SSI level (which is 73% FPL), reaching two-thirds (67%) of people with HIV. Eighteen (18) of these states set eligibility at 100% FPL, the highest level of access through the disability pathway, where 31% of people with HIV live. Twenty-seven states set eligibility at or below the federal minimum. Access to the traditional Medicaid program through the disability pathway is most limited in Connecticut (with an income limit of 53% FPL).3 However, both of these states offer coverage through the expansion, which captures individuals with and without disabilities at higher income limits. (While Alaska’s eligibility level is set at 59% FPL it is tied to the state’s higher FPL and is based on the SSI dollar amount which does not fluctuate by state).
- Expansion & Traditional Medicaid: 12 States (AZ. CA, DC, HI, IL, IN, MA, MI, NM, NJ, PA, and RI) representing 31% of people with HIV, offer the highest levels of Medicaid access providing both the expansion and the disability pathway to individuals up to 100% FPL. Nine States (AL, GA, ID, FL, KS, MS, SD, TN, TX, and WY) representing 18% of people with HIV, have the most limited access (no expansion and disability eligibility at or below the SSI level). With the exception of Tennessee, eligibility for parents with dependents is also very low in these states.
Marketplaces
For assessing marketplace access, we looked at the number of issuers available to consumers within the region. Marketplace participation is an indicator of competitiveness and enrollee choice, which can play an important role in ensuring adequate affordable coverage for high needs enrollees. Because consumer out-of-pocket costs can vary significantly by plan, and provider networks and formularies can differ substantially, having a range of plan choices can help people with HIV adequately meet care and treatment needs. We looked at two indicators by state, finding:
- Over half of states (33) have three or more issuers (a benchmark used to indicate reasonable completion) in their Marketplaces where the great majority (83%) of people with HIV live. Wisconsin had the greatest number of issuers in their Marketplace (15) followed by New York (14) and California (11). Five states (AL, AK, OK, SC, WY) had only one marketplace issuer in 2017.
- In order to make further cross state comparisons we also looked at the average number of issuers per county in a state by HIV prevalence. Forty-three percent (43%) of people with HIV live in one of eighteen (18) states with an average of 3 or more issuers per county. Fifty-seven percent (57%) of people with HIV live in one of thirty-three (33) states with less optimal choice and competition, with an average of only one or two issuers per county, though just 4% are with access to only one issuer.
- While looking at state level indicators allowed us to compare access across states and to include that indicator in our baseline, looking at issuer participation exclusively by county, which is how market participation is parsed, is most representative of what is available to individual consumers. The majority of people with HIV live in a county served by 3 or more marketplace issuers (68%) and one third (32%) live in a county served by 5 or more marketplace issuers. A relatively small share (15%) of people with HIV live in a county served by only one marketplace issuer. The highest number of issuers in any one county was nine which occurred in six counties in New York and Massachusetts and the lowest number was one (occurring in 1,036 counties in 27 states).
Ryan White
The Ryan White HIV/AIDS Program provides outpatient HIV care and treatment to low and moderate income individuals reaching more than half of those diagnosed in the US.4 In the ACA era some individuals may have stopped receiving direct care and treatment through the program, gaining it instead through Medicaid or in the private market. Further, as more people with HIV were able to secure coverage in the private insurance market (given the ACA’s nondiscrimination protections) Ryan White’s role is in assisting clients with the cost of insurance premiums and other out-of-pocket obligations (known as insurance purchasing or insurance assistance) has grown.5 In addition to ADAP, Ryan White also provides a range of outpatient services to people with HIV.
Since Ryan White operates at state and local levels, service eligibility levels and the ability of programs to provide insurance assistance vary. We looked at indicators for the traditional Ryan White Program (medication assistance and HIV care services), those related to assisting individuals with purchasing insurance, and Ryan White’s eligibility for outpatient services more generally.
Currently:
- ADAP eligibility (medication assistance): Across all states, the average eligibility level for ADAP medication assistance (the direct drug program for those without insurance) is almost 400% (386%). The most common level is also 400% which 17 states (representing 24% of people with HIV) use as their limit. Most states (36), representing nearly three-quarters (72%) of people with HIV, have ADAP eligibility at levels at or above the national average for the medication assistance program. About one quarter (28%) of people with HIV live in one of 15 states with more restrictive ADAP eligibility, below the average, in all cases also at or below 300% FPL. Eligibility for ADAP medication assistance ranges from a low of 80% of the area’s median income in Wyoming followed by 200% FPL in three states (ID, IA, and TX) to a high of 550% FPL in South Carolina.
- ADAP eligibility (insurance assistance): ADAPs in all but three states (TX, ID, and MS) are offering insurance purchasing assistance for individual plans. These states without individual market insurance purchasing comprise of 9% of people with HIV. One state (AL) offers insurance purchasing in the individual market for plans purchased outside of the health insurance marketplace whereas the other states offering this benefit, provide assistance with marketplace coverage. In all, 90% of people with HIV live in state where the ADAP will provide some individual market insurance assistance. Insurance assistance eligibility (including but not exclusively in the individual market) ranges from a low of 200% in Texas to a high of 550% FPL in South Carolina. The average eligibility level across the nation is 401% and most common eligibility level is 400%, which 18 states (representing 24% of people with HIV) use as their limit.
- Ryan White Medical services eligibility: Eligibility for state funded medical services through the Ryan White program ranges from a low of 80% of the area’s median income in Wyoming followed by 200% FPL in three states (ID, NB, and TX) to a high of 550% FPL in South Carolina. That national average is 375% FPL and the most common eligibility level is 400%, which 16 states (representing 25% of people with HIV) use as their limit.
Looking Ahead
While recent efforts to repeal and replace the ACA have not been successful, there are still questions about its future, including potential policy and legislative changes. In addition, repeal efforts have included attempts to overhaul the structure and financing of the traditional Medicaid program.6 Depending on their scope, if realized such changes could affect coverage opportunities for people with HIV.78 (For more detailed analysis of the possible impacts of repeal and replace for people with HIV see here.) If such efforts are successful, people with HIV could be forced out of marketplace coverage or off of Medicaid which could cause some to fall out of care. Others may turn to Ryan White for HIV medication and care but the program has limited resources and may not be able to meet all needs. This baseline of coverage access for people with HIV will help us to measure the effect of related policy changes moving forward.