Medicaid is the primary program providing comprehensive coverage of health care and long-term services and supports to about 80 million low-income people in the United States. Medicaid accounts for one-sixth of health care spending (and half of spending for long-term services and supports) and a large share of state budgets. Medicaid is jointly financed by states and the federal government, but administered by states within broad federal rules. Because states have the flexibility to determine what populations and services to cover, how to deliver care, and how much to reimburse providers, there is significant variation across states in program spending and the share of people covered by the program.

The independent source for health policy research, polling, and news.
Medicaid 101
Published: May 28, 2024
Table of Contents
Introduction
What Is Medicaid?
Medicaid is the primary program providing comprehensive coverage of health care and long-term services and supports to about 80 million low-income people in the United States. Medicaid accounts for one-sixth of health care spending (and half of spending for long-term services and supports) and a large share of state budgets (Figure 1).
Subject to federal standards, states administer Medicaid programs and have flexibility to determine what populations and services to cover, how to deliver care, and how much to reimburse providers. States can obtain Section 1115 waivers to test and implement approaches that differ from what is required by federal statute if the Secretary of Health and Human Services (HHS) determines the waivers would advance program objectives. Because of this flexibility, there is significant variation across state Medicaid programs, and as a result, the share of state residents covered by the program (Figure 2).
How Has Medicaid Evolved Over Time?
Title XIX of the Social Security Act and a large body of federal regulations and sub-regulatory guidance govern the program, defining federal Medicaid requirements and states’ options and authorities. At the federal level, the Centers for Medicare and Medicaid Services (CMS) within the Department of Health and Human Services (HHS) administers Medicaid and oversees states’ programs. States may choose to participate in Medicaid, but if they do, they must comply with core federal requirements. Not all states opted to participate in Medicaid immediately after its enactment in 1965, but by the 1980s, all states had opted in. Medicaid coverage was historically tied to cash assistance—either Aid to Families with Dependent Children (AFDC) or federal Supplemental Security Income (SSI). Over time, Congress expanded federal minimum requirements and provided new coverage requirements and options for states, especially for children, pregnant women, and people with disabilities. In 1996, legislation replaced Aid to Families with Dependent Children with Temporary Assistance to Needy Families (TANF) and severed the link between Medicaid eligibility and cash assistance for children, pregnant women, and low-income parents. The Children’s Health Insurance Program (CHIP) was established in 1997 to cover low-income children above the cut-off for Medicaid with an enhanced federal match rate (Figure 3).
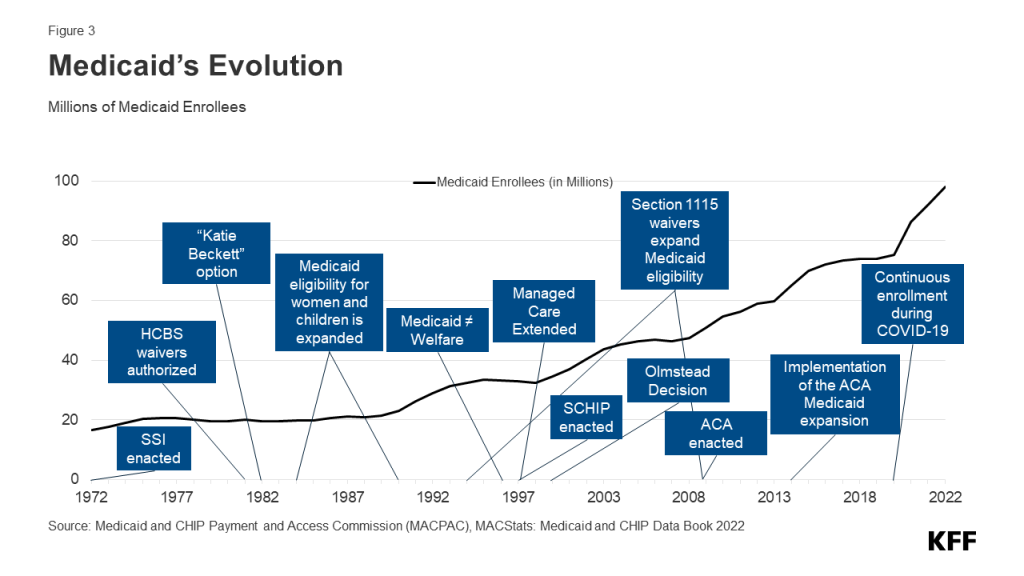
In 2010, the Affordable Care Act (ACA) expanded Medicaid to nearly all nonelderly adults with income up to 138% FPL ($20,780 annually for an individual in 2024) through a new coverage pathway for adults without dependent children who had traditionally been excluded from Medicaid coverage. However, the ACA Medicaid expansion coverage is effectively optional for states because of a 2012 Supreme Court ruling. As of March 2024, 41 states, including Washington, D.C., have expanded Medicaid (Figure 4). States receive a higher rate of federal matching funding for people who are enrolled through the new coverage pathway. Under the ACA, all states were also required to modernize and streamline Medicaid eligibility and enrollment processes to help individuals obtain and maintain coverage.
The COVID-19 pandemic profoundly affected Medicaid spending and enrollment. At the start of the pandemic, Congress enacted legislation that included a requirement that Medicaid programs keep people continuously enrolled in exchange for enhanced federal funding. As a result, Medicaid/CHIP enrollment grew substantially, and the uninsured rate dropped. The unwinding of these provisions started on April 1, 2023, and have been disenrolled from Medicaid, likely reversing recent improvements in the uninsured rate. In addition to the unwinding, many federal and state policymakers have been focused on how Medicaid can be used as a lever to help address health disparities, expand access to care, improve access to behavioral health and home and community-based services, and address workforce challenges.
How Is Medicaid Financed?
States are guaranteed federal matching dollars without a cap for qualified services provided to eligible enrollees. The match rate for most Medicaid enrollees is determined by a formula in the law that provides a match of at least 50% and provides a higher federal match rate for states with lower per capita income (Figure 5). States may receive a higher match rate for certain services and populations. The ACA expansion group is financed with a 90% federal match rate, so states pay 10%, and the American Rescue Plan Act included an additional temporary fiscal incentive to states that newly adopt the Medicaid expansion. In FY 2022, Medicaid spending totaled $804 billion of which 71% was federal spending. Medicaid spending growth typically accelerates during economic downturns as enrollment increases. Spending growth also peaked after the implementation of the ACA and, more recently, due to enrollment growth tied to the pandemic-related continuous enrollment provision.
Overall, Medicaid accounts for a large share of most states’ budgets and is often central to state fiscal decisions; however, state spending on Medicaid is second to state spending on elementary and secondary education, and the program is also the largest source of federal revenue for states. In state fiscal year 2022, Medicaid accounted for 29% of total state expenditures, 15% of expenditures from state funds (general funds and other funds), and 52% of expenditures from federal funds received by the state.
Social Security, Medicare, and Medicaid are the three main entitlement programs, accounting for 44% of all federal outlays in FFY 2023. Of these three programs, Medicaid is the smallest in terms of federal outlays, though it covers more people than Medicare or Social Security. Overall, federal spending on domestic and global health programs and services accounted for 29% of net federal outlays in FFY 2023, including spending on Medicare (13%), Medicaid and CHIP (10%), and other health spending (6%). Dating back to the 1980s, there have been efforts to limit federal financing for Medicaid either through a block grant to states or through a cap on spending per enrollee as a way to help reduce federal spending. Such efforts may shift costs to states, providers or enrollees and have been blocked to date but could emerge again.
Who Is Covered by Medicaid?
Medicaid is an entitlement, meaning individuals who meet eligibility requirements are guaranteed coverage. The federal government sets minimum eligibility standards, but states may expand coverage beyond these minimum requirements. Federal minimum eligibility levels for children and pregnant women are set at 133% of the federal poverty level (FPL) ($35,630 for a family of 3 in 2024); however, median eligibility levels for these groups were 255% FPL for children and 207% FPL for pregnant women as of January 2023. As a result of the ACA, the median coverage level for parents and adults without dependent children is 138% FPL, but for states that have not adopted the ACA expansion, the median eligibility for parents was 38% FPL. In non-expansion states, adults without dependent coverage are not eligible for Medicaid coverage and those with incomes below poverty fall into the coverage gap.
Medicaid coverage is also available to certain individuals who qualify on the basis of being age 65 and older or having a disability. These coverage categories are referred to as “non-MAGI” pathways because they do not use the Modified Adjusted Gross Income (MAGI) financial methodology that applies to pathways for pregnant people, parents, and children with low incomes. In addition to considering advanced age, disability status, and income, many non-MAGI pathways also have asset limits. Medicaid generally covers individuals who qualify for Supplemental Security Income (SSI), but nearly all other non-MAGI pathways are optional, resulting in substantial state variation. Each group has different rules about income and assets, making eligibility complex (Figure 6).
Medicaid coverage is limited for immigrants, and except for emergency services, Medicaid coverage is not available for undocumented immigrants. A number of states, however, use state funds to provide coverage to all or some undocumented immigrants.
While Medicaid covers 1 in 5 people living in the United States, Medicaid is a particularly significant source of coverage for certain populations. In 2022, Medicaid covered 4 in 10 children, 8 in 10 children in poverty, 1 in 6 adults, and 6 in 10 nonelderly adults in poverty. Relative to White children and adults, Medicaid covers a higher share of Black, Hispanic, and American Indian or Alaska Native (AIAN) children and adults. Medicaid covers 44% of nonelderly, noninstitutionalized adults with disabilities, who are defined as having one or more difficulty related to hearing, vision, cognition, ambulation, self-care, or independent living (Figure 7).
Medicaid provides coverage for a number of special populations. For example, Medicaid covers 41% of all births in the United States, nearly half of children with special health care needs, 5 in 8 nursing home residents, 23% of non-elderly adults with any mental illness, and 40% of non-elderly adults with HIV. Medicaid pays Medicare premiums and often provides wraparound coverage for services not covered by Medicare (like most long-term services and supports) for nearly 1 in 5 Medicare beneficiaries (13 million). Medicaid is a key source of coverage for individuals experiencing homelessness and those transitioning out of carceral settings, particularly in states that have adopted the Medicaid expansion.
Among the non-elderly covered by Medicaid, nearly half are children under age 19, 6 in 10 are people of color, 57% are female, and three-quarters are in a family with a full- or part-time worker. Even though most adult Medicaid enrollees are working, many do not have an offer of employer-sponsored coverage, or it is not available.
What Benefits Are Covered by Medicaid?
Medicaid covers a broad range of services to address the diverse needs of the populations it serves. In addition to covering the services required by federal Medicaid law, all states elect to cover at least some services that are not mandatory (Figure 8). All states cover prescription drugs, and most states cover physical therapy, eyeglasses, and dental care. Medicaid provides comprehensive benefits for children, known as Early Periodic Screening Diagnosis and Treatment (EPSDT) services. EPSDT is especially important for children with disabilities because it allows children access to a broader set of benefits to address complex health needs than what is traditionally covered by private insurance. Unlike commercial health insurance and Medicare, Medicaid also covers non-emergency medical transportation, which helps enrollees get to appointments, and long-term care, including nursing home care and many home and community-based services (HCBS). Coverage for long-term services and supports is mandatory for nursing facilities, but most coverage of HCBS is optional. In recent years, states have expanded coverage of behavioral health services and benefits to help enrollees address social determinants of health (SDOH) like nutrition or housing.
What Long-term Services and Supports (LTSS) Are Covered by Medicaid?
Most people ages 65 and older and many people under age 65 with disabilities have Medicare, but Medicare does not cover most LTSS; instead, Medicaid is the primary payer for LTSS. LTSS encompass the broad range of paid and unpaid medical and personal care services that assist with activities of daily living (such as eating, bathing, and dressing) and instrumental activities of daily living (such as preparing meals, managing medication, and housekeeping). They are provided to people who need such services because of aging, chronic illness, or disability. These services include nursing facility care, adult daycare programs, home health aide services, personal care services, transportation, and supported employment. They may be provided over several weeks, months, or years, depending on an individual’s health care coverage and level of need. There have been longstanding challenges finding enough workers to provide LTSS for all people who need such services, and the COVID-19 pandemic exacerbated those issues considerably. As the population ages and advances in medicine and technology enable people with serious disabilities to live longer, the number of people in need of LTSS is expected to grow.
In 2023, the median annual costs of care in the U.S. were $116,800 for a private room in a nursing home, $64,200 for an assisted living facility, and $75,504 for a home health aide. Medicare provides home health and skilled nursing facility care under specific circumstances, but the Medicare benefit is considered “post-acute” care and generally not available for people needing services on an ongoing basis. Medicaid plays a key role in access to LTSS for people who qualify because LTSS costs are difficult for most people to afford when paying out-of-pocket. In some cases, people only qualify for Medicaid after exhausting their savings on the costs of LTSS. In 2022, Medicaid paid 58% of the $438 billion spent on LTSS in the U.S. (Figure 9).
LTSS may be provided in various settings broadly categorized as institutional or non-institutional. Institutional settings include nursing facilities and intermediate care facilities for people with intellectual disabilities. Services provided in non-institutional settings are known as home and community-based services (HCBS), and these settings may include a person’s home, adult day care centers, assisted living settings, and group homes. Federal Medicaid statutes require states to cover institutional LTSS and home health, but the remainder of HCBS are optional. Even without a mandate to cover HCBS, Medicaid LTSS spending has shifted from institutional to non-institutional settings over time. In 2022, most spending for LTSS in the U.S. was for HCBS. That shift reflects beneficiary preferences for receiving care in non-institutional settings and requirements for states to provide services in the least restrictive setting possible stemming from the Olmstead decision. In 2021, there were 5.7 million people who used Medicaid LTSS, of which 4.3 million (75%) used only HCBS, 1.2 million (21%) used only institutional care, and 0.2 million used both (4%). While, overall, three-quarters of people who used Medicaid LTSS were exclusively served in home and community-based settings, the share varied across states (Figure 10). To qualify for coverage of LTSS under Medicaid, people must meet state-specific eligibility requirements regarding their levels of income, wealth, and functional limitations.
How Much Does Medicaid Spend and on What?
Managed care is the dominant delivery system for Medicaid enrollees with 74% of Medicaid beneficiaries enrolled in comprehensive managed care organizations (MCOs). Medicaid MCOs provide comprehensive acute care and, in some cases, long-term services and supports to Medicaid beneficiaries and are paid a set per member per month payment for these services. In FFY 2022, payments to managed care and health plans accounted for the largest share (55%) of Medicaid spending, with capitated payments to comprehensive MCOs accounting for 52% of Medicaid spending and payments to other Medicaid managed care (e.g. primary care case management (PCCM) arrangements or specialty plans) accounting for another 3% (Figure 11). Smaller shares of total Medicaid spending in FFY 2022 were for fee-for-service acute care (20%), fee-for-service long-term services and supports (19%), Medicaid spending for Medicare premiums on behalf of enrollees who also have Medicare (3%), and disproportionate share hospital (DSH) payments (2%).
Medicaid spending is driven by multiple factors, including the number and mix of enrollees, their use of health care and long-term services and supports, the prices of Medicaid services, and state policy choices about benefits, provider payment rates, and other program factors. During economic downturns, enrollment in Medicaid grows, increasing state Medicaid costs while state tax revenues are declining. Due to the federal match, as spending increases during economic downturns, so does federal funding. During the pandemic-induced recession and the two economic downturns prior to the pandemic, Congress enacted legislation that temporarily increased the federal share of Medicaid spending to provide increased support for states to help fund Medicaid. High enrollment growth rates, tied first to the Great Recession, then ACA implementation, and later the pandemic, were the primary drivers of total Medicaid spending growth over the last two decades (Figure 12).
How Much Does Medicaid Spending Vary Across Enrollee Groups and States?
People eligible based on being age 65 or older or based on a disability comprise 1 in 4 enrollees but account for more than half of Medicaid spending, reflecting high health care needs and in many cases, use of long-term services and supports (Figure 13).
Across the states, spending per enrollee ranged from a low of $4,500 in South Carolina to $12,008 in the District of Columbia in 2021. Variation in spending across the states reflects considerable flexibility for states to design and administer their own programs – including what benefits are covered and how much providers are paid — and variation in the health and population characteristics of state residents. Within each state, there is also substantial variation in the average costs for each eligibility group, and within each eligibility group, per-enrollee costs may vary significantly, particularly for individuals eligible based on disability (Figure 14).
In 2021, people who used Medicaid LTSS comprised 6% of Medicaid enrollment but 34% of federal and state Medicaid spending (Figure 15). High per-person Medicaid spending among enrollees who use LTSS likely reflects the generally high cost of LTSS and more extensive health needs among such groups that lead to higher use of other health care services and drugs as well.
How Are Medicaid Services Delivered?
As of July 2023, 41 states (including Washington, D.C.) contract with comprehensive, risk-based managed care plans – often administered by private insurance companies — to provide care to at least some of their Medicaid beneficiaries (Figure 16). Medicaid MCOs provide comprehensive acute care and, in some cases, LTSS to Medicaid beneficiaries and are paid a set per member per month payment for these services. States have traditionally used managed care models to increase budget predictability, constrain Medicaid spending, and improve access to care and value. While the shift to MCOs has increased budget predictability for states, the evidence about the impact of managed care on access to care and costs is both limited and mixed. Children and adults are more likely to be enrolled in MCOs than adults aged 65 and older and people eligible because of a disability; however, states are increasingly including beneficiaries with complex needs in MCOs. States are also increasingly leveraging Medicaid MCOs to help identify and address social determinants of health and to reduce health disparities.
What Is Known About Access in Medicaid?
A large body of research shows that Medicaid beneficiaries have substantially better access to care than people who are uninsured (who are also primarily low-income) and are less likely to postpone or go without needed care due to cost. Key measures of access to care and satisfaction with care among Medicaid enrollees are comparable to rates for people with private insurance (Figure 17). Given that Medicaid enrollees have low incomes, federal rules generally have protections to limit out-of-pocket costs that can help improve access. An analysis of data from a KFF Survey of Consumer Experiences with Health Insurance finds that Medicaid enrollees report fewer cost-related problems relative to those with Marketplace coverage and employer coverage.
Longstanding research shows that Medicaid eligibility during childhood is associated with positive effects on health and have positive impacts beyond health, such as improved long-run educational attainment. Early and updated research findings show that state Medicaid expansions to adults are associated with increased access to care, improved self-reported health status, reduced mortality among adults, and increases in economic security.
Gaps in access to certain providers, particularly psychiatrists and dentists, are ongoing challenges in Medicaid. These and other gaps in access tend to mirror system-wide access problems that affect Medicare and the private insurance market, but they are exacerbated in Medicaid by provider shortages in low-income communities, Medicaid’s lower physician payment rates, and lower provider participation in Medicaid compared with private insurance. In 2021, MACPAC found physicians were less likely to accept new Medicaid patients (74%) than those with Medicare (88%) or private insurance (96%), but these rates may vary by state, provider type and setting. Medicaid acceptance was much higher where physicians practiced in community health centers, mental health centers, non-federal government clinics, and family clinics compared to the average for all settings. Provider participation rates may contribute to findings that Medicaid enrollees may experience more difficulty obtaining health care than those with private insurance. A KFF survey of Consumers shows that Medicaid enrollees report more problems with prior authorization and provider availability compared to people with other insurance types.
How Do Medicaid Demonstration Waivers Work?
The majority of states have 1115 demonstration waivers to test approaches not otherwise allowed under federal law. Section 1115 demonstration waivers offer states the ability to test new approaches in Medicaid that differ from what is required by federal statute, if CMS determines that such proposals are “likely to assist in promoting the objectives of the Medicaid program.” Section 1115 waivers have been used over time and generally reflect priorities identified by the states and CMS, but they also reflect changing priorities from one presidential administration to another. Under different administrations, waivers have been used to expand coverage, modify delivery systems, and restructure financing and other program elements. Nearly all states have at least one 1115 waiver in place, and many have waivers pending with CMS (Figure 18).
Activity from the Trump Administration and into the Biden Administration has tested how these waivers can be used to advance administrative priorities and has also tested the balance between states’ flexibility and discretion by the federal government. The Trump Administration’s Section 1115 waiver policy emphasized work requirements and other eligibility restrictions, payment for institutional behavioral health services, and capped financing. The Biden Administration withdrew waiver approvals with work requirements, phased out approval of premium requirements, and has instead encouraged states to propose waivers that expand coverage, reduce health disparities, and/or advance “whole-person care.” Recent areas of focus have included leveraging Medicaid to address health-related social needs and to provide health care to individuals transitioning from incarceration back into the community. A few states have also sought approval to provide continuous Medicaid coverage for children and certain adults for periods longer than a year.
Various types of waivers and other emergency authorities can also be used to help respond in emergencies. Such authorities can help expand Medicaid capacity and focus on specific services, providers, or groups of enrollees that are particularly impacted. During the COVID-19 pandemic, all 50 states and Washington, D.C. received approval to make changes using emergency authorities to facilitate access to care by expanding telehealth, eligibility, benefits and help address workforce issues for home- and community-based services.
The expiration of the COVID-19 public health emergency (PHE) in May 2023 had implications across the health care system for costs, coverage and access. States needed to unwind many Medicaid emergency policies that were in place or transition policies to more permanent authorities. For example, a number of states were adopting changes in telehealth and some home- and community-based services more permanently.
Future Outlook
Looking to the future, Medicaid faces a number of challenges, including:
- How has Medicaid enrollment changed since the start of the unwinding of the continuous enrollment provision and how will these changes affect the uninsured and other coverage trends?
- What Medicaid strategies can be used to improve access to services, particularly for behavioral health?
- What policies may help bolster support for Medicaid providers as states experience challenges with reimbursement rates and provider shortages, particularly for LTSS as demand increases?
- What new federal and state efforts will be used to leverage Medicaid to help address racial health disparities and social determinants of health and how effective will these strategies be?
- What federal and state fiscal issues will emerge and how will these issues affect Medicaid financing and federal and state budgets?
Policy changes to Medicaid have implications for the roughly 80 million people who rely on the program for health coverage, state and federal budgets and spending, and health care providers, including nursing facilities and home and community-based service providers. Changes in Medicaid enrollment also typically have implications for overall coverage trends. When more people have Medicaid coverage, the uninsured rate typically falls, and when individuals lose Medicaid coverage, the number of uninsured typically increases.
Resources
- 10 Things to Know About Medicaid
- Medicaid: What to Watch in 2024
- Medicaid Financing: The Basics
- 10 Things to Know About Medicaid Managed Care
- 10 Things About Long-Term Services and Supports (LTSS)
- 50-State Medicaid Budget Survey Archives
- 10 Things to Know About the Unwinding of the Medicaid Continuous Enrollment Provision
- Medicaid Enrollment and Unwinding Tracker
- Status of State Medicaid Expansion Decisions: Interactive Map
- Medicaid Waiver Tracker: Approved and Pending Section 1115 Waivers by State
Citation
Rudowitz, R., Tolbert, J., Burns, A., Hinton, E., & Mudumala, A., Medicaid 101. In Altman, Drew (Editor), Health Policy 101, (KFF, May 28, 2024) https://www.kff.org/health-policy-101-medicaid/ (date accessed).




