
The independent source for health policy research, polling, and news.
Gross Medicare Spending on Ozempic and Other GLP-1s Is Already Skyrocketing – Even Though Medicare Cannot Cover The Drugs for Weight Loss
A KFF analysis shows that gross total Medicare spending on Ozempic and other similar drugs has increased dramatically in recent years – even though Medicare is explicitly prohibited by law from covering the drugs for obesity.
That’s because Medicare now covers the drugs, known as GLP-1s, for other medically accepted indications, including to treat diabetes. This week the Centers for Medicare & Medicaid Services (CMS) informed Medicare drug plans that they can cover Wegovy, another drug in this class, for its newly approved use of preventing heart attacks and strokes for people who are obese or overweight.
In 2022, Medicare gross total spending reached $5.7 billion on Ozempic (semaglutide), Rybelsus (semaglutide), and Mounjaro (tirzepatide), all of which it covered for diabetes that year, according to just-released Medicare drug spending data. That was up from $57 million in 2018. (Gross spending does not account for any rebates paid by drug manufacturers to pharmacy benefit managers, which would result in lower net Medicare spending.)
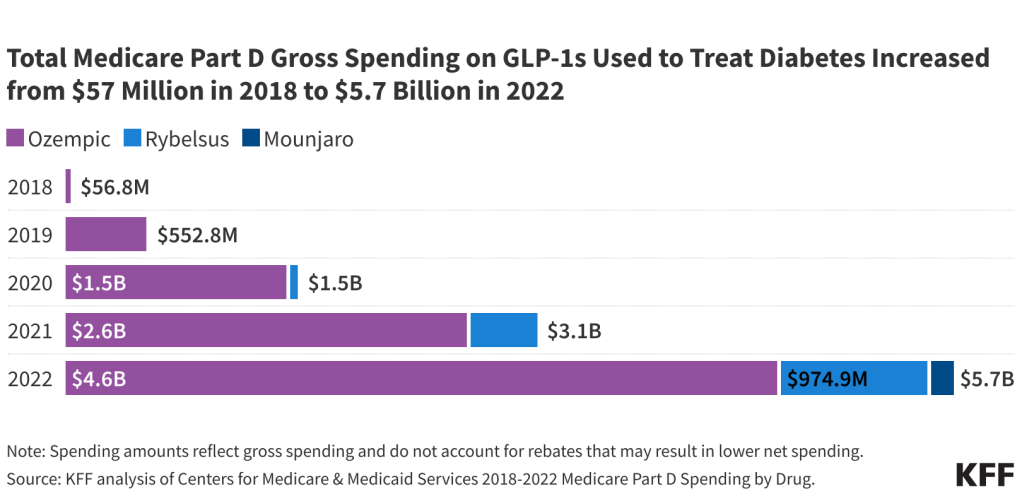
Gross spending on Ozempic alone increased from $2.6 billion in 2021 to $4.6 billion in 2022, pushing it to 6th place among the top-selling drugs in Medicare Part D that year, up from 10th place the year before.
The fact that covering GLP-1s under Medicare Part D for authorized uses is already making a mark on total Part D program spending could be a sign of even higher spending to come as Part D plans are now able to cover Wegovy for its heart health benefits, and if new uses for GLP-1s are approved.
These drugs offer substantial potential health benefits, but the combination of intense demand, new uses, and high prices for these treatments is likely to place tremendous pressure on Medicare spending, Part D plan costs, and premiums for Part D coverage.