Coverage of Preventive Services for Adults in Medicaid
The Kaiser Commission on Medicaid and the Uninsured conducted a survey of Medicaid programs in all 50 states and the District of Columbia on coverage of and cost sharing for preventive services. Thirty-nine states and the District of Columbia replied to the survey. States were asked whether they covered 40 services recommended by the USPSTF and ACIP as well as seven additional services recommended for women by HRSA. States were also asked whether they charge cost sharing for services, except for pregnancy-related services.
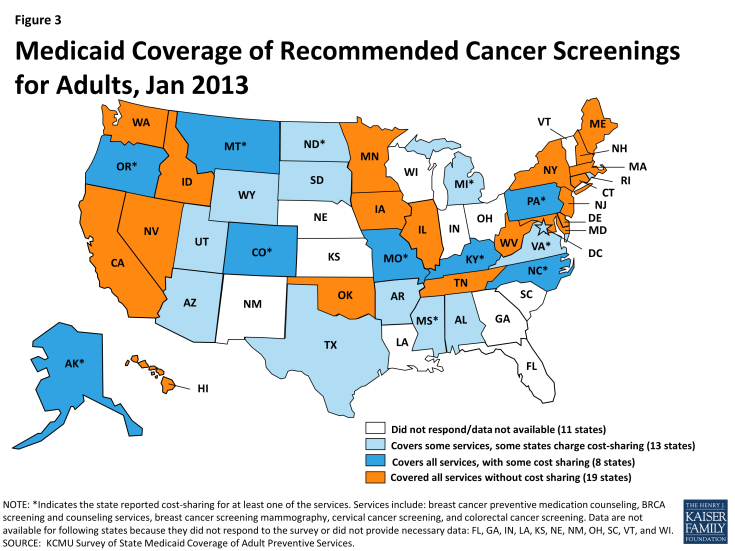
Cancer Screenings (Table 1)
TABLE 1: CANCER-RELATED SERVICES (as of January 2013)
Great strides in early detection and advances in treatment options have improved overall cancer survival rates over many decades. The USPSTF recommends three different services related to breast cancer as well as screening tests for cervical and colorectal cancers.
Breast Cancer Mammography, Cervical Cancer, and Colorectal Cancer Screenings
In total, 19 states cover all of the cancer-related services without cost sharing. Virtually all states responding to the survey indicated that they cover mammograms, cervical cancer screenings, and colorectal cancer screenings as recommended by the USPSTF. Arkansas reported that it does not cover both mammography and colorectal cancer screening, and Michigan noted that it does not cover screening for colorectal cancer. Only a handful of states reported cost-sharing for these services (8 states for colorectal cancer screenings, and 7 states for breast cancer mammography and cervical cancer screenings.)
Some states noted mammograms and cervical cancer screenings were at least in part covered through an optional eligibility pathway adopted by all states under the Breast and Cervical Cancer Prevention and Treatment Act. This option allows states to extend Medicaid coverage for cancer treatment to uninsured women diagnosed with breast or cervical cancer through a federal screening program; states receive a higher matching rate for services reimbursed under this program equivalent to the CHIP matching rate.1 A few states also noted coverage of these services under the family planning benefit, which is reimbursed at a 90 percent matching rate.
Breast Cancer Preventive Medication Counseling, BRCA Screening and Counseling
Coverage for two other services recommended by the USPSTF – breast cancer preventive medication counseling and BRCA screening, are not as commonly covered as the cancer screening tests discussed above. These services are recommended only for women who are deemed at high risk of breast cancer or those with a family history of deleterious mutations of select genes. Twenty-eight states cover both of these services; an additional 7 states cover one of these services but not the other. Ten states charge copays for one or both of these services (Figure 3).
Sexually-Transmitted Infection (STI) Screenings and Counseling (Table 2)
TABLE 2: SEXUALLY-TRANSMITTED INFECTION (STI) SCREENINGS (January 2013)
There are 20 million new sexually-transmitted infections (STIs) every year.2 Undetected and untreated STIs can increase a person’s risk for HIV and can lead to other adverse health consequences, such as infertility. According to the Centers for Disease Control and Prevention (CDC), less than half of people who should be screened for STIs receive recommended screening services.
Chlamydia, Gonorrhea, and Syphilis Screenings and STI Counseling
Almost all states participating in this survey reported covering screening tests for Chlamydia, Gonorrhea, and Syphilis as recommended by the USPSTF. Eight states reported that at least one of these STI screenings was subject to cost-sharing. Fewer states cover counseling about STIs as recommended by the USPSTF, though 32 states did report covering this service. Seven states indicated that they charge cost-sharing for STI counseling services. In total, 31 states covered all the STI screenings and counseling services; 22 of these states do so without charging cost-sharing (Figure 4).
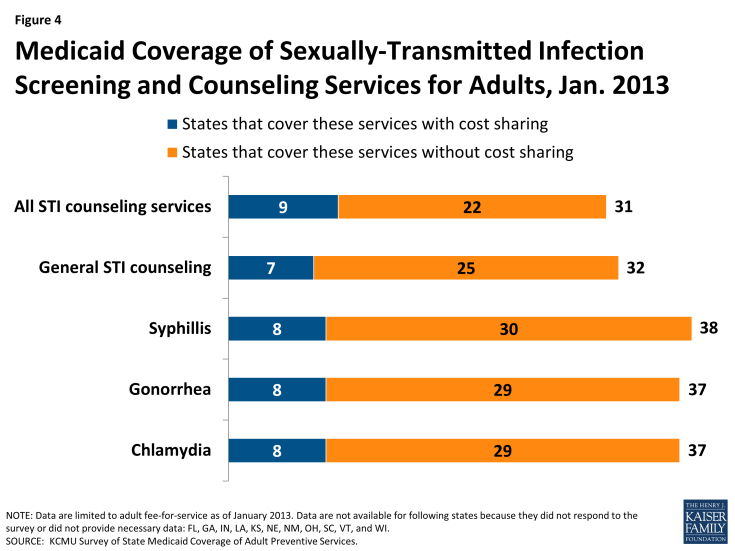
Figure 4: Medicaid Coverage of Sexually-Transmitted Infection Screening and Counseling Services for Adults, Jan. 2013
Some states noted some of these services are at least partially covered as family planning services. Family planning is a mandatory benefit for states; however the services covered under this benefit as well as limitations on those services vary across states, though states cannot charge cost-sharing for these services. States receive a 90 percent federal match on services covered under this benefit. Family planning services are not considered to be a preventive service for purposes of receiving the 1% increase in FMAP.
For non-elderly adults, states were surveyed regarding the coverage of two forms of HIV screenings: HIV for high risk populations and routine HIV screenings for adults. These survey results are reported in more detail on the Kaiser Family Foundation’s website at State Medicaid Coverage of Routine HIV Screening.3
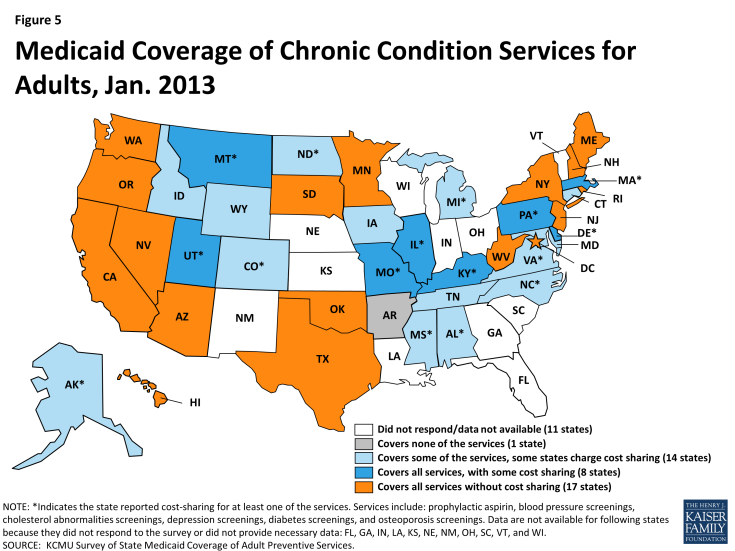
Preventive Services Related to Chronic Conditions (Table 3)
TABLE 3: CHRONIC CONDITION-RELATED SERVICES (January 2013)
Chronic conditions afflict millions of women and men with Medicaid. Nearly one in ten low-income, non-elderly adult Medicaid beneficiaries have been diagnosed with diabetes, more than two in ten with chronic obstructive pulmonary disease, nearly three in ten with heart disease, and over one-third have been diagnosed with a mental health condition.4 Research has shown that increases in the use of preventive services, particularly screenings and treatment related to cardiovascular disease, can lead to the prevention of a significant number of deaths per year.5
Prophylactic Aspirin, Blood Pressure, Cholesterol, Depression, Diabetes, and Osteoporosis Screenings
Overall, 25 states reported covering all of the services in this category; 17 without cost-sharing (Figure 5). Nearly all states reported covering blood pressure screenings and screenings for cholesterol abnormalities (38 states each). Fewer states reported covering prophylactic aspirin (31 states) despite research highlighting in particular its effectiveness in reducing the number of deaths from cardiovascular disease and its potential to yield significant medical savings.6 Copays were also most prevalent for this service compared to others in this category. Additionally, most states reported coverage of diabetes screenings (37 states) and osteoporosis screenings (35 states).
There is a high prevalence of diagnosed mental health conditions among Medicaid beneficiaries. The only preventive service specific to mental health in this survey was depression screening, which is covered by most states; 26 of the 34 states that cover this service do not charge cost-sharing.
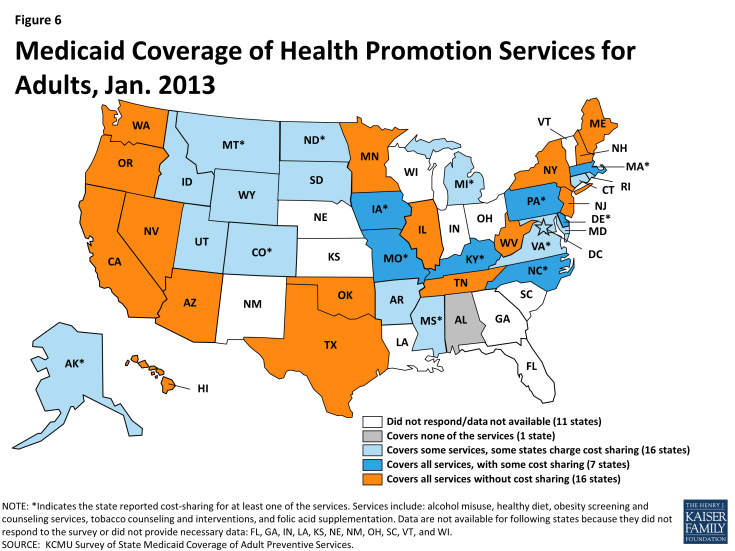
Health Promotion (Table 4)
TABLE 4: HEALTH PROMOTION SERVICES (as of January 2013)
The category of health promotion includes a number of services aimed at promoting healthy behaviors that help prevent chronic illnesses. This includes screening for obesity and counseling on a number of behavioral issues such as diet and nutrition, tobacco use, and alcohol use.
Alcohol Misuse, Healthy Diet, Obesity Screening and Counseling, Tobacco Use Counseling, Folic Acid Supplementation
Twenty-three states covered all of the recommended preventive services that fall under this category; 16 states did so without cost-sharing (Figure 6). One state reported they do not cover any of these preventive services for adults (Alabama).
Nearly every state that covered healthy diet counseling services also covered obesity screening and counseling; the same 7 states also reported cost-sharing for both of these services.7 The obesity-related services are particularly important given the alarming high obesity rates in the United States and obesity’s link to many chronic conditions such as coronary heart disease, stroke, diabetes, and cancer.8
The most commonly covered service was tobacco use counseling and interventions (34 states) with 28 of these states doing so without cost-sharing. Research has highlighted the potential of tobacco use counseling and interventions to yield cost-savings and have large health impacts.9 Most of the surveyed states also cover counseling on alcohol misuse. Thirty-three states reported covering this service and 25 of them do not charge cost-sharing.
The USPSTF also recommends that women of childbearing capability take a daily supplement of folic acid to prevent certain birth defects. Thirty-one states reported covering this service and 21 of them do so without cost-sharing.
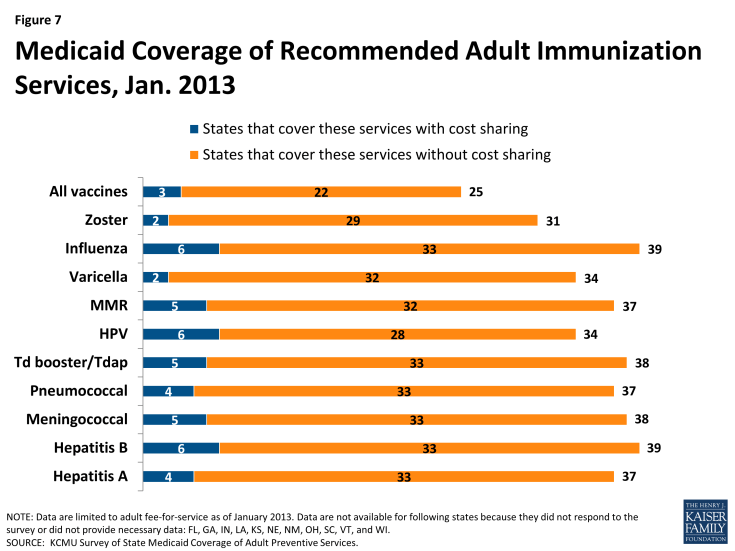
Immunizations (Tables 5A and 5B)
TABLE 5A: IMMUNIZATIONS RECOMMENDED IF OTHER RISK FACTORS ARE PRESENT (as of January 2013)
TABLE 5B: IMMUNIZATIONS RECOMMENDED FOR ALL PERSONS MEETING AGE AND GENDER REQUIREMENTS WHO LACK EVIDENCE OF IMMUNITY (as of January 2013)
There are ten immunizations recommended for adults by the Advisory Committee on Immunization Practices (ACIP). Six of the immunizations (Td booster/Tdap, MMR, Influenza, Varicella, Zoster and HPV) are recommended for all individuals who meet select age and gender criteria and who show no sign of immunity. Four (Hepatitis A, Hepatitis B, Meningococcal, and Pneumococcal) are recommended for those when additional risk factors are present.
Td booster/Tdap, MMR, Influenza, Varicella, Zoster, HPV, Hepatitis A and B, Meningococcal, and Pneumococcal
In total, 22 states reported covering all the recommended immunizations without cost-sharing (Figure 7). While 25 states indicated that they covered all of the recommended immunizations for non-elderly adults, some charged cost sharing. A number of other states reported coverage of the immunizations, but for a narrower age range than is recommended (i.e. for those 18 years and younger).
The most commonly covered immunizations were for Influenza and Hepatitis B (39 states). Both immunizations for MMR and Td booster/Tdap were covered for non-elderly adults by most states (37 and 38 states, respectively). However, fewer states cover Varicella (34 states) and Zoster (31 states). Another less commonly covered immunization was HPV; 34 states covered this immunization for women age 26 and under, and some of these 34 states reported covering the immunization for males as well.
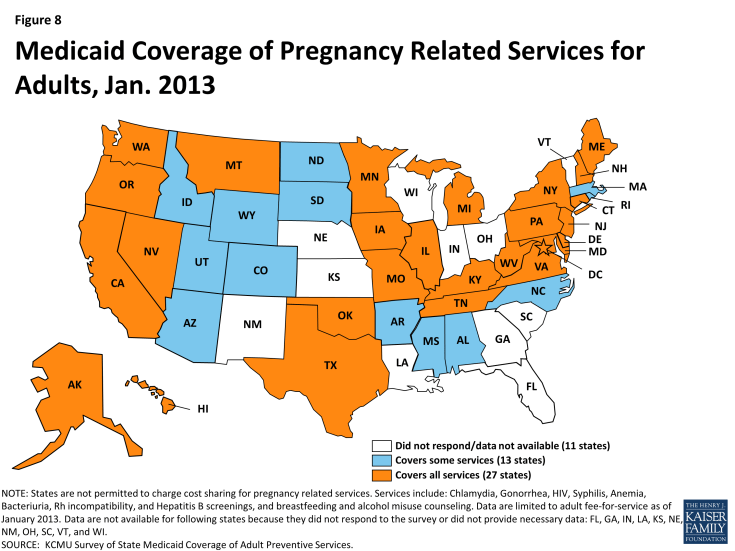
Pregnancy-Related Preventive Services
Approximately half of all births in the U.S. are paid for by Medicaid, making it the single largest payor for maternity care.10 Responses to the survey showed that preventive services recommended by the USPSTF for pregnant women were well-covered under state Medicaid programs in January 2013. Because pregnancy-related services are exempted from cost-sharing, states were not asked about cost-sharing for these services. (Figure 8).
STI and HIV Screenings (Table 6A)
TABLE 6A: SEXUALLY-TRANSMITTED INFECTION (STI) SCREENINGS FOR PREGNANT WOMEN (January 2013)
All states responding to the survey reported covering STI screenings for Chlamydia, Gonorrhea and Syphilis, which matches data reported on STI screenings covered for non-elderly adults in an earlier section. All states reported covering HIV screening for pregnant women as well.
Hepatitis B, Anemia, Bacteriuria, Rh Incompatibility Screenings, Breast Feeding Counseling, and Alcohol Misuse Counseling (Table 6B)
TABLE 6B: PREGNANCY-RELATED SCREENINGS AND COUNSELING SERVICES (as of January 2013)
All states responding to the survey reported covering screenings for Hepatitis B, as well as Rh incompatibility at both the first prenatal visit and again at 24-28 gestational weeks. All but two states also covered bacteriuria and anemia screenings. While not as common, the majority of states also cover breastfeeding counseling (29 states) and alcohol misuse counseling (36 states).
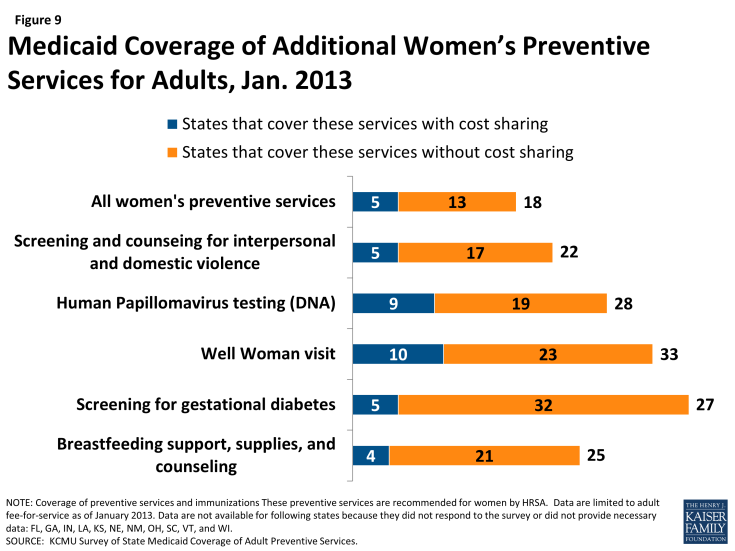
Women’s Preventive Services Recommended by the Health Resources and Services Administration
In addition to the preventive services recommended by the USPSTF and ACIP, Section 2713 of the ACA called for the formation of a committee to study and recommend whether any additional preventive services for women should be covered by private insurance plans. A committee of the IOM recommended eight additional preventive services for women11 and these recommendations were subsequently adopted by HRSA.12 As a result, all new private plans must cover these services without cost sharing. However, the additional women’s preventive services are not included as part of the Medicaid enhanced match for preventive services. Nonetheless, we surveyed states about Medicaid coverage of these services and found that all states covered most or some of the additional services. Of the 39 states and DC that responded, 18 covered all of these services and 13 of these states do not charge cost sharing for any of the services (Figure 9).
Screening for Gestational Diabetes and Breastfeeding Support, Supplies, and Counseling (Table 7A)13
TABLE 7A: ADDITIONAL WOMEN’S SERVICES
Most states (32) cover screening for gestational diabetes in pregnant women without cost sharing. Coverage for breastfeeding supports is not as common, with only 21 states reporting they cover these supports without cost sharing. While the USPSTF has recommended breastfeeding counseling prior to the passage of the ACA, the recommendation from HRSA is more expansive as it recommends coverage of counseling as well as supplies, in particular breast pumps.
Well Woman Visit, Human Papillomavirus DNA Testing, and Screening and Counseling for Interpersonal and Domestic Violence (Table 7B)
TABLE 7B: WOMEN’S PREVENTIVE SERVICES
HRSA also recommends coverage for at least one annual well woman visit, DNA testing for HPV, and screening and counseling for interpersonal and domestic violence. More than half of states cover well woman visits (33 states) and HPV testing (28 states), but that is not the case for interpersonal and domestic violence screening (22 states). However, many states charge cost sharing for these services and overall, of the 20 states that report covering all three of these services, 15 states cover them without cost-sharing.
Summary
The ACA provides a number of opportunities to improve access to and quality of care for many adults currently in Medicaid programs and those that are newly eligible since January 1, 2014. Medicaid coverage of preventive services for adults has historically been considered optional, meaning states can elect whether to cover preventive services in their Medicaid programs for adults. Furthermore, states are permitted to charge cost sharing for some beneficiaries, in the low-income population that Medicaid serves, where even nominal charges can pose a barrier to obtaining services.14
To date, at least eight states have taken up the ACA incentive for an enhanced match for preventive services. While all of the individual preventive services were covered by most state Medicaid programs in 2013, many states charged cost sharing for at least some of the services. Overall, 12 states reported covering all of the services included in the survey; eight of them did so without cost-sharing. Another 16 states reported covering at least 40 of the recommended services. In general, there was more variation in cost-sharing policies; 10 states reported cost-sharing for at least ten of the services.
While the ACA requires states to cover preventive services without cost sharing for newly eligible Medicaid populations in the Alternative Benefit Plans (ABPs), coverage of preventive services is provided at state option for those eligible for Medicaid prior to the ACA’s coverage expansion. As these plans are developed, additional states could align the benefits in their traditional Medicaid programs with the ABPs, and thus expand coverage of preventive services without cost sharing to previously eligible populations as well through amendments to their state Medicaid plans. This would reduce differences in benefits between different groups of Medicaid beneficiaries and would also extend coverage for preventive services to a broader group of individuals on the program.
Methodology
The data in this report reflect results from a survey fielded April through June 2013 that asked states about coverage and related cost-sharing for those preventive services recommended for non-elderly adults by the USPSTF (services that received a grade “A” or “B”,) some services under review by USPSTF at the time of the survey, some services recommended by HRSA and immunizations recommended by the ACIP; 47 services in total were included in the survey, which are detailed in Appendix A. These data do not reflect coverage for children or those over the age of 65 in Medicaid programs. Data are reported for 39 states and the District of Columbia that responded to the survey; data are not reported for the 11 states that did not respond or did not provide complete data: Florida, Georgia, Indiana, Kansas, Louisiana, Nebraska, New Mexico, Ohio, South Carolina, Vermont, and Wisconsin.
The survey instrument (a copy of which is provided in Appendix B) asked states if they had submitted or planned to submit a state plan amendment to receive the enhanced match for covering all the recommended services without cost sharing; if a state responded that they in fact did, they were assumed to have covered all preventive services with no cost-sharing asked about in the survey. All of the states that reported that they either submitted or planned to submit a SPA at the time of the survey have been approved (CA, NH, NJ, and NY) except for LA. While LA reported plans to submit a SPA, to date, there is no SPA submission posted for this state and documentation from the state’s website indicates that they do not cover at least some of the preventive services asked about in this survey. Therefore, data are not reported for LA. Some states did not respond to all questions; these cases are noted as “NR” in the appendix tables.
Coverage
The survey asked if the state Medicaid program covered any of the recommended preventive services. Many states responded with service-specific caveats, most notably that service was covered only if medically necessary or that the service was covered but only as part of an office visit and not as a distinct service. For purposes of this report, states reporting such caveats were counted as covering these services.
Cost-sharing
This survey asked states to report if they charged cost-sharing for the recommended preventive services. States were asked to include cost-sharing that applied to 1) the service when billed separately from the related office or clinic visit and 2) the visit if the preventive services was the primary purpose of the visit and the services and visit are not billed separately.