The Uninsured at the Starting Line in California: California findings from the 2013 Kaiser Survey of Low-Income Americans and the ACA
Background: The Challenge of Expanding Health Coverage in California
Lack of insurance coverage has been a longstanding policy challenge both nationwide and in California. Not having health insurance has well-documented adverse effects on people’s use of health care, health status, and mortality, as the uninsured are more likely to delay or forgo needed care leading to more severe health problems.1 Lack of insurance coverage also has implications for people’s personal finances, providers’ revenue streams, and system-wide financing.2,3,4 Because public coverage has been extended to many children and Medicare covers nearly all of the elderly, the vast majority of uninsured people are non-elderly adults. To address the challenge of the uninsured, the Affordable Care Act (ACA) includes an expansion of Medicaid (known in California as Medi-Cal) and the creation of new Health Insurance Marketplaces (known in California as Covered California).
California, the nation’s most populous state, has the largest number of uninsured of any state across the country. In 2012, twenty-one percent of the state’s nonelderly population was uninsured, or about 7 million people, which accounts for 15% of the uninsured nationwide.5 Los Angeles County alone, which has a population the size of many states, has a greater number of uninsured residents (2.2 million) than found in any state except New York, Florida, or Texas.6 Therefore, California’s actions to expand coverage through the Medi-Cal expansion and Covered California have implications not only for health coverage and access within the state but also for national goals of reducing the total number of uninsured.
California also is a highly diverse state, with 60% of the state identifying as a race other than White.7 The state is home to more than 10 million immigrants,8 including more than five million non-citizens, and has the largest number of undocumented immigrants in the nation.9 These unique characteristics of the state shape the challenge of extending health coverage and in implementing the ACA.
California’s Health Insurance Environment
Prior to the ACA, California had one of the highest uninsured rates in the nation and, correspondingly, one of the lowest rates of private insurance coverage, which includes group coverage obtained through an employer and individual coverage purchased directly from an insurance company (nongroup).10 One reason for the low rate is coverage is California’s unemployment rate, which at 8.7% is higher than the national average (7.3%).11 However, many workers in California lack health insurance: in 2012, one in four California workers was uninsured.12 Workers lack coverage for a variety of reasons, including not being offered coverage by their employer and not being able to afford coverage. Premiums and copayments for health coverage in California have been steadily rising over the past decade, and average premiums for nongroup coverage in California are higher than the national average ($572 per month in California compared to $490 per month nationally).13
Still, as in other states, private coverage is the main source of insurance among those with coverage in California, and the private insurance market accounts for nearly three quarters of covered lives in California (excluding the elderly population).14 California has a concentrated private insurance market, with six insurers accounting for three-quarters of the market in 2011.15 The state also has a long history of managed care, with the majority of enrollees receiving coverage through a managed care plan.16
Medi-Cal is a large player in the state, accounting for over a quarter of nonelderly covered lives, or about 7.3 million individuals.17 While Medi-Cal covers children in families with incomes up to 250% FPL18, eligibility for parents and adults without dependent children was more limited prior to the ACA and LIHP, leaving many adults without affordable coverage. Specifically, Medi-Cal was available only to parents with incomes up to the poverty level, and non-disabled adults without children were ineligible for coverage. The state also had adopted the option to eliminate the five year waiting period for coverage for eligible lawfully residing pregnant women and children and adopted the unborn child option to provide care to pregnant women, regardless of immigration status.19 However, other lawfully residing immigrants remained subject to a five-year waiting period before they could enroll in coverage, and undocumented immigrants remained ineligible to enroll in coverage.
California has the lowest Medicaid payment rates to physicians in the nation. In 2012, Medi-Cal payment rates to physicians for primary care services were 43% of Medicare rates, compared to a national average of 59%.20 Due to budget shortfalls, the state passed a 10% provider rate cut for most Medi-Cal providers, and this cut was implemented in January 2014.21,22 Simultaneously, under the ACA, California is required to pay certain physicians Medi-Cal fees that are at least equal to Medicare’s for a list of 146 primary care services; this fee increase is in place for 2013 and 2014, and the federal government will pay 100% of the cost of the difference between the increased rate and the state’s rate in place in 2009.23,24 Thus, fees paid to certain physicians for primary care services will be protected from the Medi-Cal rate cut in 2014 (because the federal government will fund the difference between the state’s rates and Medicare rates), but this federal funding and protection from rate cuts ends in 2015.
For uninsured residents in California, health care services are primarily financed and administered at the county level. Under California law, the state’s counties are “providers of last resort” for health services to low-income uninsured adults without other sources of care. California’s counties, therefore, have a history of financing, and in some instances delivering, health care to low-income, underserved, and uninsured individuals. All of California’s 58 counties have at least one health program for Medically Indigent Adults (MIA), and counties vary on the quantity and scope of health services covered.25 California also has a robust network of county hospitals, community health centers, and community clinics that make up a significant share of the state’s safety net system.26 These providers will play an important role in reaching, educating, and enrolling newly eligible individuals into coverage under the ACA.
Health Reform in California
Under the ACA, California will extend Medi-Cal coverage to citizens and eligible legal immigrants (those who have been U.S. residents for more than five years) with incomes up to 138% FPL ($16,105 for an individual or $27,210 for family of three in 2014). It is estimated that between 990,000 and 1.4 million Californians will enroll in Medi-Cal under the expansion by 2019.27
To assist the state in preparing for the Medi-Cal expansion in 2014, the federal government approved California’s five-year “Bridge to Reform” Section 1115 Medicaid Demonstration Waiver in November 2010.28 The waiver provides the opportunity for California’s safety net hospitals, including county and University of California hospitals, to draw down federal matching funds to develop new programs and innovative approaches to improve quality of care through the creation of the Delivery System Reform Incentive Program (DSRIP). Federal funds are available for four priority areas, including (1) infrastructure development, (2) innovation and redesign, (3) population-focused improvement, and (4) urgent improvement in care.29 Twelve of California’s 21 designated safety net hospitals are participating in DSRIP, and each has developed a plan that describes specific improvement projects and related milestones. Milestones are reported to the state through semi-annual reports, incentive payments are tied to achieving each milestone.30
In addition to DSRIP and authority to transition Medi-Cal-only seniors and persons with disabilities (SPDs) to managed care arrangements,31 the Bridge to Reform waiver allowed the state to draw down federal matching funds to expand coverage to low-income uninsured adults through the creation of a county-based Low-Income Health Program (LIHP). LIHP consisted of two programs: the Medicaid Coverage Expansion (MCE) for non-elderly, non-pregnant adults with family incomes at or below 133% FPL and the Health Care Coverage Initiative (HCCI) for non-elderly, non-pregnant adults with family incomes between 133-200%.32 Counties could elect to participate in LIHP and, if participating, decide whether to expand coverage to individuals with family incomes up to 133% FPL or up to 200% FPL (or a lower threshold set by the county). As of September 2013, 53 of the state’s 58 counties were participating in the LIHP program, and over 667,000 adults were enrolled.33,34 The state worked with the counties to transition LIHP enrollees to coverage options available under the ACA as of January 2014, transitioning nearly 644,000 beneficiaries to Medi-Cal and 24,000 beneficiaries to Covered California coverage in 2014.35,36
Also under the ACA, people with incomes up to 400% FPL who do not have an affordable offer of coverage are eligible to receive tax credits to purchase coverage through Health Insurance Marketplaces; citizens and legal immigrants who are not eligible for tax credits can purchase unsubsidized coverage. California was the first state in the country to pass legislation to create a state-based Marketplace under the ACA. The Marketplace, called Covered California, is governed by an appointed five-member board and operates as an independent public agency. Since its inception, Covered California has actively pursued grant funding to assist with planning and operations and received about $910 million in federal grants.37 Covered California enrollees can select among the plans offered by the participating 13 commercial health plans.38 Over three million Californians are estimated to be eligible to purchase coverage through Covered California, with about two million of those individuals eligible for premium tax credits.39
California’s early efforts enabled the state to reach many uninsured targeted for coverage expansions early in ACA implementation. For example, by September 2013, nearly all (almost 70,000) individuals eligible for the Medi-Cal expansion had enrolled in LIHP in Alameda County.40 However, many eligible uninsured remain across the state. For these individuals, outreach and enrollment efforts are essential to help educate them about coverage options and help them successfully complete an application. There are a range of outreach and education efforts underway in the state, including statewide marketing campaigns, community mobilization to reach people at the local level, provider training, outreach to transition people from LIHP coverage to Medi-Cal, and targeted efforts to reach vulnerable populations who may be newly-eligible for Medi-Cal.41 For example, the California Department of Health Care Services and The California Endowment, a private grant-making foundation, have been awarded federal matching funds for a $23 million Outreach and Enrollment Grant to enhance outreach and increase Medi-Cal enrollment, including support for Certified Enrollment Counselors.42 The funds will be distributed by the state to 36 county and regional organizations that must use the funds to target uninsured people who are difficult to reach or enroll, such as those with mental health needs, substance abuse disorders, the homeless, young men of color, as well as people with limited English proficiency.43 In addition, 125 health centers operating over 1,000 sites throughout the state received $25.1 million in federal grants in fiscal years 2013 and 2014 to help with outreach and enrollment assistance.44
Covered California is also investing heavily in outreach and enrollment efforts. For example, Covered California is using federal funding for an Outreach and Education Grant Program to engage the state’s uninsured population and increase awareness and understanding of health coverage options.45,46 The program has allocated $43 million in grants to 48 community organizations, including $37 million that was distributed in 2013 and $6 million allotted for 2014.47 These grants were primarily to organizations targeting individuals but also include some organizations targeting small businesses or providers.48 Covered California also established an Assisters Program and is working with community organizations to provide direct assistance to consumers to help them enroll in coverage. To further expand marketing and outreach, especially efforts aimed at uninsured young adults and uninsured Hispanics to bolster enrollment assistance and to sustain Marketplace operations, Covered California was awarded a $155 million federal grant in January 2014.49 These efforts overlay other state and local campaigns and ongoing outreach and enrollment activities.
A Profile of The Uninsured in California
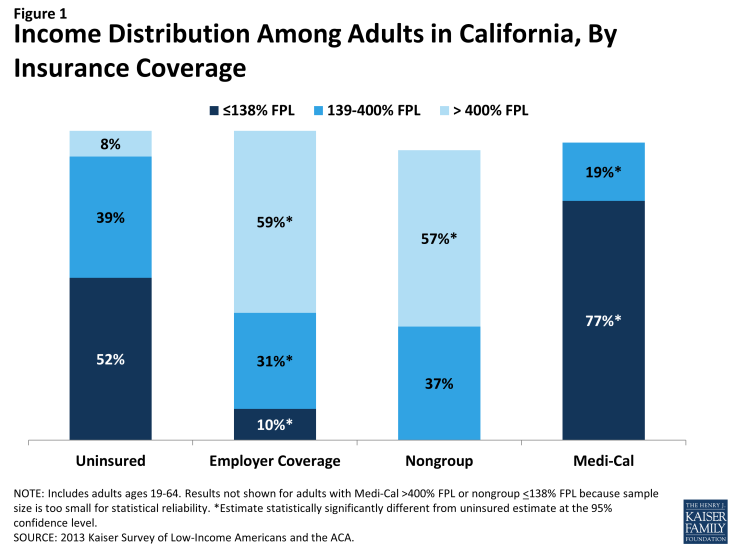
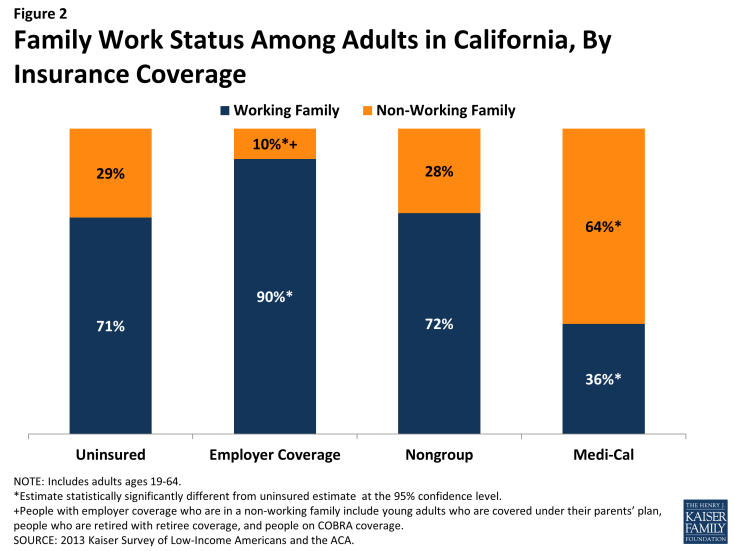
Barriers to coverage in the past and state demographics are reflected in the characteristics of the uninsured population in California. For example, a majority of uninsured adults (52%) are low-income, in contrast to 10% of adults with employer coverage (Figure 1 and Appendix Table A1). Adults with Medi-Cal are the most likely of any coverage group to be low-income, reflecting the fact that prior to the ACA, adult income eligibility was limited. Further, the majority of uninsured Californians live in families where they or their spouse are working (71%)(Figure 2). However, not surprisingly, uninsured adults in California are less likely than adults with employer coverage to be in a working family.
Uninsured adults in California also differ from insured adults with regards to demographic characteristics, often reflecting association with income or work status. Uninsured adults are likely to be younger than insured adults, as younger adults have lower incomes and looser ties to employment than older adults. Two-thirds (66%) of uninsured adults are ages 19-44 as compared to 56% of adults with employer coverage or 52% with Medi-Cal (Appendix Table A1). There also are significant racial and ethnic differences in health coverage among nonelderly adults, primarily reflecting differences in income by race/ethnicity. For example, uninsured adults are more likely to be Hispanic – 52% of uninsured adults are Hispanic – than adults with employer coverage (26%). Over one third of uninsured adults in the state are noncitizens (36%), compared to 20% of adults with Medi-Cal or 10% of adults with employer coverage. Citizenship status may leave many uninsured adults ineligible for assistance, increasing the likelihood they will remain uninsured.
As efforts continue to reach, educate, and enroll individuals into health coverage under the ACA, it is important to remember who the ACA aims to help and how their characteristics and previous interactions with the health system may inform efforts to connect with them.