Low-Income and Communities of Color at Higher Risk of Serious Illness if Infected with Coronavirus
The number of confirmed cases of coronavirus in the U.S. has steadily climbed and is now the highest in the world. The Centers for Disease Control and Prevention (CDC) and state and local governments continue to release data about the characteristics of people who have developed serious illness when infected with coronavirus, as well as the number of hospitalizations and deaths due to COVID-19. These emerging national and state-level data suggest that serious illness resulting from coronavirus disproportionately affects people in communities of color, due to the underlying health and economic challenges that they face. Similarly, adults with low incomes are more likely to have higher rates of chronic conditions compared to adults with high incomes, which could increase their risk of serious illness if infected with coronavirus.
To provide greater insight into the characteristics of people at greater risk of illness if infected with the novel coronavirus, we build on a prior analysis of higher risk adults in the U.S. to break down these numbers by race/ethnicity and household income in 2018. Our definition of higher risk includes: non-elderly adults between the ages of 18 and 64 with heart disease, chronic obstructive pulmonary disease (COPD), uncontrolled asthma, diabetes, or a body mass index (BMI) greater than 40, following the risk factors identified by the CDC. See Methods for more information.
Key Findings
Our prior analysis found about one in five adults (21%) ages 18-64 have a higher risk of developing serious illness if they become infected with coronavirus, due to an underlying health condition. This analysis finds:
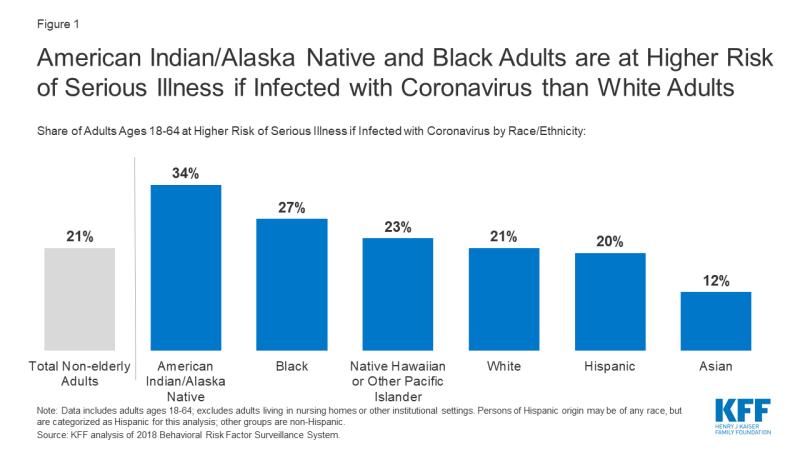
- More than one in three (34%) American Indian/Alaska Native non-elderly adults are at higher risk of serious illness if infected with the coronavirus; this share is greater than all other racial and ethnic groups (Figure 1).
- More than one in four (27%) Black non-elderly adults are at higher risk of serious illness if infected with coronavirus, compared to about one in five (21%) White adults.
- Asian non-elderly adults have the smallest share (12%) of adults at higher risk of serious illness among the racial and ethnic groups included in this analysis.
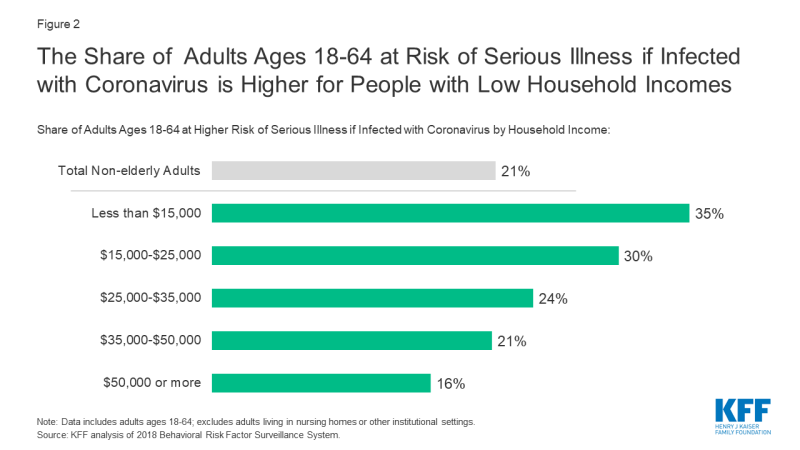
- More than one in three (35%) non-elderly adults with household incomes below $15,000 are at higher risk of serious illness if infected with coronavirus, compared to about one in seven (16%) adults with household incomes greater than $50,000 (Figure 2).
Discussion
Most people who are infected with the novel coronavirus are not expected to become seriously ill, however, about one in five non-elderly adults (21%) have an underlying medical condition which puts them at higher risk of serious illness if they get infected. Among people ages 18-64, American Indian/Alaska Native and Black adults are more likely than White adults to be at a higher risk of serious illness due to underlying health conditions and longstanding disparities in health care and other socio-economic factors. Even though the shares of Hispanic and Native Hawaiian or Pacific Islander nonelderly adults at higher risk for serious illness if infected are similar to that of White adults, these groups face disparities in other health, social, and economic factors that may contribute to barriers to health care associated with coronavirus. Although our analysis finds Asian adults are the least likely to be at higher risk for serious illness, this finding may mask subgroups of Asian adults who may be at higher risk.
A larger share of non-elderly adults with lower household income than higher household income have a greater risk of serious illness if they are infected with coronavirus. This is principally because of underlying health conditions that are more prevalent among non-elderly adults with low incomes. People with low incomes who work in jobs such as grocery story workers, delivery drivers or home health aides that are defined as essential may put themselves at higher risk of contracting coronavirus than others who are able to shelter in place and follow guidelines for social distancing.
Lack of health insurance could pose challenges to people seeking treatment for COVID-19, which could disproportionately affect non-elderly adults with low incomes and people in communities of color. On April 24, 2020, the Paycheck Protection Program and Health Care Enhancement Act was signed into law, adding an additional $100 billion to the Provider Relief Fund, with funding to reimburse providers for treating uninsured patients with COVID-19. However, the large number of providers and services which are eligible for reimbursement could drain available funds, raising questions about coverage for the uninsured, and the costs of their care when such funds are no longer available.
Federal and state governments are strengthening their efforts to collect and report data by demographics on coronavirus testing, hospitalizations, and deaths. Even so, efforts to analyze these data are limited by the large number of missing responses, and limited surveillance in certain communities. Comprehensive nationwide data, broken down by race and ethnicity and income, are needed to understand how COVID-19 is affecting communities in the U.S. and how best to target coronavirus testing and other resources accordingly.
| Methods |
| This brief analyzes data from the nationally-representative, cross-sectional 2018 Behavioral Risk Factor Surveillance System (BRFSS) of adults ages 18 to 64 living in the community. BRFSS is an ongoing, state-based, random-digit-dialed telephone survey of non-institutionalized civilian adults. The 2018 survey has over 430,000 respondents. Information about the BRFSS is available at http://www.cdc.gov/brfss/index.html. For this analysis, we calculated the share of people at risk of serious illness if they get infected with coronavirus, using BRFSS, by race/ethnicity and self-reported annual household income. The estimates of the percentage of adults at higher risk by race/ethnicity and household income use the BRFSS survey weights to account for the complex sampling design. Data exclude missing values for race/ethnicity and income; data also exclude approximately 15 percent of non-elderly adults who did not know or refused to report their household income. Data exclude adults living in Guam or Puerto Rico. Data represent adults who report ever being told by a doctor that they have one of the listed conditions. Because the CDC guidelines suggest that those with moderate or severe asthma are at greater risk than those with mild asthma, we adjusted the overall total to account for the share with uncontrolled asthma, adjusting the overall total by 62 percent, based on CDC prevalence. |