Wide Variations in Flu Vaccination Rates Across States Highlight Challenges as State and Local Authorities Plan to Distribute a COVID-19 Vaccine
When a COVID-19 vaccine becomes available, all or most people living in the country will need to get vaccinated in order to maximize its benefits and provide adequate immunity nationwide.
That could present a daunting challenge for state and local health officials, as a new KFF analysis shows vaccination rates for the annual flu vaccine vary widely across states as well as by race and ethnicity, age, and other demographic characteristics.
The flu vaccine provides a good model for understanding how quickly and broadly a new vaccine could be distributed and administered across the country. For the past decade, it’s been recommended for everyone at least 6 months old and, because of the Affordable Care Act, is available free of charge to people with insurance, as well as uninsured children through the Vaccines for Children Program.
Even so, the analysis finds slightly more than half (52%) of the public received the recommended vaccine during last year’s flu season, well below the federal government’s 70% target vaccination rate. Across states, Rhode Island had the highest (61%) and Nevada the lowest (44%) vaccination rate for seasonal flu.
Other findings include:
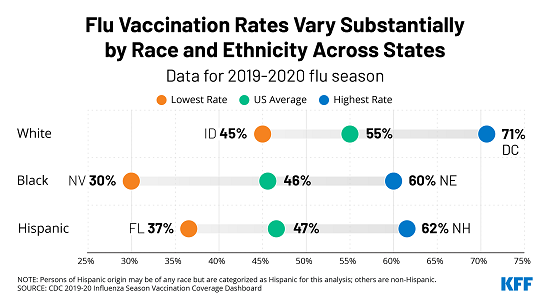
- In most states, Black and Hispanic people had lower flu vaccination rates compared to their White counterparts, but these differences varied across states.
- Vaccination rates were highest for seniors and significantly lower for other adults across states. Children’s vaccination rates generally fall in the middle.
- Across states, adults with underlying health conditions that could put them at heightened risk of severe illness from COVID-19 generally had higher flu vaccination rates than other adults.
The analysis highlights factors that may contribute to the variations in flu vaccination rates across states and could lead to similar variations for any future COVID-19 vaccine. These include lower rates of insurance coverage, particularly for people of color; the lack of dedicated vaccination programs for uninsured adults; whether and for whom states mandate vaccinations; differences in funding and public health infrastructure; and variation in levels of concern or misconceptions about vaccine safety, side effects, and efficacy.