Tracking Social Determinants of Health During the COVID-19 Pandemic
The public health and economic effects of the pandemic continue to affect the well-being of many people living in the United States. Over the course of the pandemic, millions have lost jobs or income and have faced difficulty paying for expenses including basic needs like food and housing. These social and economic challenges affect people’s health and well-being. Federal legislation has provided billions in funding to address the public health crisis of the pandemic and to provide economic support to many low-income people struggling to make ends meet. This brief provides an overview of how adults are faring across an array of measures of social determinants of health as of March 2 – March 14, 2022 based on data from the Census Bureau’s Household Pulse Survey, which was designed to quickly compile data about how people’s lives have been impacted by the coronavirus pandemic. For this analysis, we looked at a range of measures over the course of the pandemic. Unfortunately, the Household Pulse Survey does not provide pre-pandemic measures for comparison. While we have tracked data over time and there have been fluctuations at various points since March 2020, patterns of hardship remain largely consistent and changes in measures do not necessarily follow economic indicators or pandemic trends.
What are social determinants of health?
Social determinants of health are the conditions in which people are born, grow, live, work, and age.1 They include factors like socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care (Figure 1).
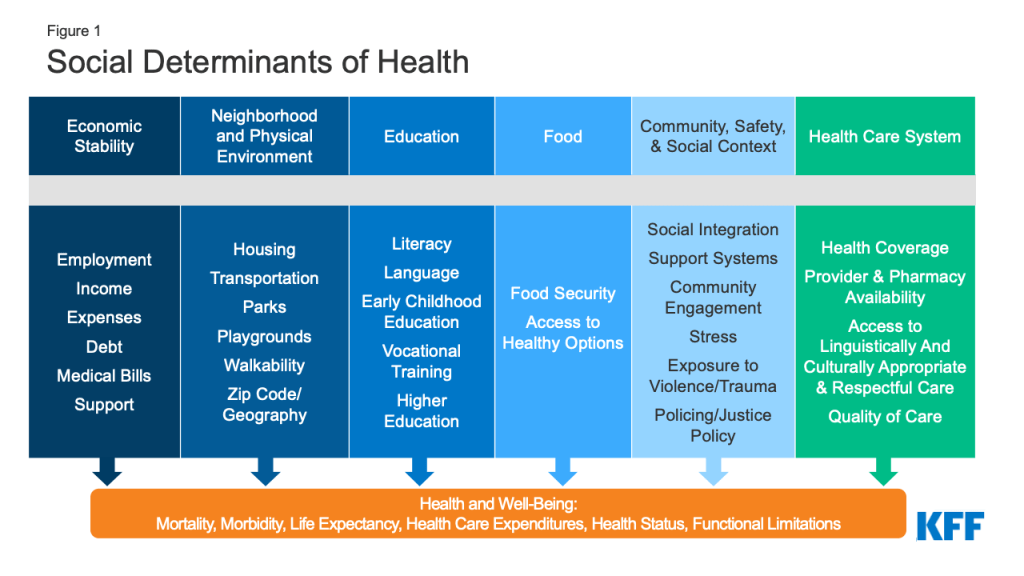
Though health care is essential to health, research shows that health outcomes are driven an array of factors outside the health care system may play an even larger role in shaping health. Extensive research concludes that addressing social determinants of health is important for improving health outcomes and reducing health disparities.2 Prior to the pandemic there were a variety of initiatives underway to address social determinants of health both in health and non-health sectors. The COVID-19 pandemic has not only disproportionately affected the health of people of color and other high-need groups, but also had disproportionate impacts on economic and social factors.
How are adults faring across a range of social determinants of health during the pandemic?
Across a wide range of metrics, large shares of people are experiencing hardship. Data for the most recent period, March 2 – March 14, 2022, show that (Figure 2):
- More than one in eight adults (13.6%) reported that they or someone in their household had experienced a loss of employment income in the past four weeks;
- More than six in ten (61.3%) of adults reported at least a little difficulty paying for usual household expenses in the past 7 days, and 31.8% used credit cards or loans to meet household spending needs;
- 7% of adults had no confidence in their ability to make next month’s housing payment (across renters and owners), and 10.3% reported food insufficiency in their household;
- Nearly one in three (31.4%) adults reported symptoms of depression or anxiety.
Black and Hispanic adults fare worse than White adults across nearly all measures, with large differences in some measures. In early March 2022, three quarters of Black and Hispanic adults (74.4% and 75.2%, respectively) reported difficulty paying household expenditures compared to 55.5% of White adults; 9.6% of Black adults and 8.4% of Hispanic adults reported no confidence in their ability to make next month’s housing payment compared to 4.0% of White adults; and 20.4% of Black adults and 16.2% of Hispanic adults reported food insufficiency in the household compared to 7.1% of White adults. Furthermore, nearly a fifth of Black adults, and about one in four Hispanic adults reported living in a household that experienced a loss of employment income in the last four weeks (17.1% and 23.0%, respectively) compared to 10.2% of White adults.
Patterns of hardship over time indicate both the effects of the pandemic and related policies as well as longstanding disparities in social determinants of health. Data indicate that the share of people experiencing depression or anxiety, food insufficiency, loss of employment income, and having no confidence in paying for their housing peaked in December 2020 but have otherwise remained largely stable (data not shown). Notably however, the share of adults having at least a little difficulty paying usual household expenses in the past 7 days has risen significantly from 50.9% in early September to 61.3%. This could potentially be due to rising prices for many household goods. However, differences in rates of hardship among certain populations have been evident throughout the pandemic and to some extent reflect longstanding disparities that existed even before the pandemic.
While variation across age and gender was not as stark, younger adults (ages 18 to 44) fared worse on many measures compared to older adults. For example, higher shares of younger adults reported symptoms of anxiety and depression as well as having a little difficulty paying for usual household expenses. In addition, higher shares of women reported symptoms of depression or anxiety and difficulty paying usual household expenses in the past seven days compared to men.
Across most measures, adults with children in their household fared worse compared to overall adults. For example, 17.5% of adults with children in the household experienced loss of employment income in the household in the last four weeks compared to 13.6% of adults overall, and over two thirds (69.2%) of adults with children in the household reported difficulty paying for household expenses in the past week compared to the overall population of 61.3%. Adults in households with children were also more likely to report food insufficiency, symptoms of depression or anxiety, having no confidence in ability to make next month’s housing payment than the general population, and borrowing from friends or family to meet household spending.
What to watch going forward
Federal legislation provided billions of dollars to help address the ongoing health and economic effects of the pandemic, including direct economic support for individuals. This federal support may have contributed to some improvements in metrics since peaks early in the pandemic. However, some federal funding has expired, and the trajectory and duration of the pandemic is not clear with new variants and surges despite the availability of vaccines. Congress may consider broader legislative proposals that had been part of the Build Back Better Act which could expand health coverage and help to address health disparities across different demographic groups, but the status and outcome of that legislation is uncertain.
The authors thank former KFF Vice President Rachel Garfield and former KFF Senior Data Analyst Kendal Orgera for their role as authors of previous versions of this report.
- “About Social Determinants of Health,” World Health Organization, http://www.who.int/social_determinants/sdh_definition/en/. ↩︎
- “Healthy People 2020: Social Determinants of Health,” Office of Disease Prevention and Health Promotion, accessed December 4, 2020, https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. ↩︎
