Medicaid Reforms to Expand Coverage, Control Costs and Improve Care: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2015 and 2016
Long-Term Services and Supports Reforms
| Key Section Findings |
Additional information on LTSS expansions implemented in FY 2015 or planned for FY 2016 can be found in Tables 13 and 14. These tables are also available in a downloadable PDF. |
Medicaid is the nation’s primary payer for long-term services and supports (LTSS) covering a continuum of services ranging from home and community-based services (HCBS) that allow persons to live independently in their own homes or in the community, to institutional care provided in nursing facilities and intermediate care facilities for individuals with intellectual disabilities (ICF-ID). Long-term services and supports represent at least one-third of Medicaid spending and are an important focus for state policymakers.1 This year’s survey shows that almost all states are employing a variety of tools and strategies to expand HCBS options including traditional Section 1915(c) HCBS waivers, PACE programs,2 and managed LTSS.
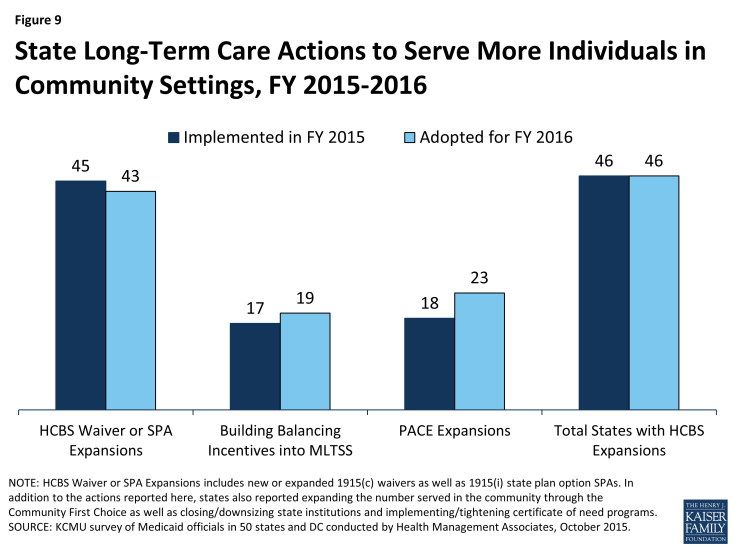
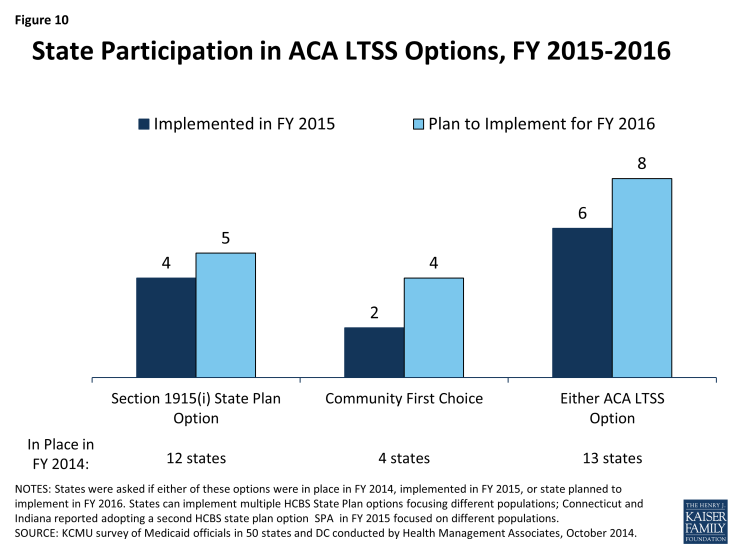
Figure 9: State Long-Term Care Actions to Serve More Individuals in Community Settings, FY 2015-2016
Nearly every state reported actions to expand the number of persons served in community settings in both years (46 states in FY 2015 and in FY 2016). The number of states taking such actions has increased since FY 2012 (26 states) and FY 2013 (22 states). While virtually every state reported using Section 1915(c) waivers or Section 1915(i) state plan authority to expand HCBS, a significant number of states (17 in FY 2015 and 19 in FY 2016) also reported that the incentives built into their managed care programs were expected to increase the availability of HCBS. Also, 18 states in FY 2015 and 23 states in FY 2016 reported implementing or expanding PACE programs. (Figure 9) A number of states (15 states in FY 2015 and 15 in FY 2016) reported closing or downsizing institutions that led to more community placements and several states (four states in FY 2015 and three states in FY 2016) reported implementing or tightening a Certificate of Need program or imposing a moratorium on construction of new institutional beds. States also reported increased take up of ACA options to expand community-based LTSS (discussed below).
Several states reported on a number of other rebalancing initiatives. California reported that its Department of Health Care Services will collaborate with its Department of Housing and Community Development to award rental subsidies to developers and Medi-Cal community-based organizations (CBOs) using grant awards received from the U.S. Department of Housing and Urban Development. The CBOs will use the subsidies to transition institutionalized or homeless Medi-Cal beneficiaries into private independent living settings partnered with home and community-based services.3 Connecticut reported that it was continuing to implement its Strategic Plan to Rebalance Long-Term Services and Supports including a second round of rebalancing grant awards, announced by Governor Malloy in May 2015, to help the state’s nursing home industry diversify services to meet the changing needs of older adults and other people with disabilities. Several states also noted the implementation of conflict-free case management and single points of entry4 and one state commented that it was in the process of developing and testing a uniform assessment tool that, in the future, should have a positive impact on rebalancing the LTSS system.
Three states (Iowa, Illinois and Tennessee) reported new HCBS restrictions or limitations in FY 2015 or FY 2016: Iowa reported that its HCBS waiver for persons with intellectual and developmental disabilities (IDD) had reached its federally approved enrollment cap causing the state to implement a waiting list in FY 2015; Illinois reported that it is planning to change its Level of Care criteria for nursing homes as part of a legislative mandate which will also reduce the number of persons eligible for Section 1915(c) waiver services; and in FY 2016, Tennessee will also begin limiting new enrollment into a Section 1915(i)-like group (offered under Section 1115 authority) to SSI eligible beneficiaries only. People already enrolled in the group under institutional income standards will be grandfathered.5
Long-Term Services and Supports Options in the ACA
The ACA created and expanded several LTSS-related options intended to promote LTSS rebalancing. This year’s survey asked about two LTSS-related options intended to promote LTSS rebalancing that were created or expanded by the ACA: the Community First Choice Option and the Section 1915(i) HCBS State Plan Option. Thirteen (13) states reported having at least one of these options in place in FY 2014; six states reported implementing at least one of these options in FY 2015 and eight reported plans to do so in FY 2016. (Figure 10) State utilization of each of these options is discussed below.
An additional program, the Balancing Incentive Program (BIP) was created under the ACA to provide enhanced Medicaid matching funds to certain states that meet requirements for expanding the share of LTSS spending for HCBS (and reducing the share of LTSS spending for institutional services). The enhanced funding ended in September 2015. For more information on the impact of this program, please see the following brief.6
Section 1915(i) HCBS State Plan Option
This option allows states to offer HCBS through a Medicaid state plan amendment (SPA) rather than through a Section 1915(c) waiver. As a result of changes made in the ACA, income eligibility for this option was extended up to 300 percent of the maximum SSI federal benefit rate and states were permitted to target benefits to specific populations and offer the same range of HCBS under Section 1915(i) as are available under Section 1915(c) waivers. Unlike Section 1915(c) waivers, however, states are not permitted to cap enrollment or maintain a waiting list and, if offered, the benefit must be available statewide. If enrollment exceeds the state’s projections, the state may tighten their Section 1915(i) needs-based eligibility criteria, subject to advance notice and grandfathering of existing beneficiaries. Twelve states reported having an HCBS state plan option in place in FY 2014. Four states (Connecticut, Delaware, DC and Indiana) reported implementing in FY 2015; Connecticut and Indiana already had 1915(i) SPAs in place but implemented additional ones in FY 2015. Five states (Maryland, Minnesota, Mississippi, New York and Texas) reported plans to implement in FY 2016.
States were also asked to describe the target populations for their Section 1915(i) SPAs. Adults with significant mental health needs were identified by the largest number of states (7) followed by persons with intellectual and developmental disabilities (5), children with significant mental health needs (4), the elderly (3) and persons with vision impairments or physical disabilities (1). For some states, the target population included more than one of these categories. Also, two states (Connecticut and Idaho) have two Section 1915(i) SPAs in place, while Indiana implemented a third Section 1915(i) SPA in FY 2015 for adults diagnosed with mental health conditions and have incomes below 300 percent of the supplemental security income benefit rate (SSI), including persons who lost Medicaid coverage when the state’s spend-down program was eliminated.7
Community First Choice (CFC) State Plan Option
States electing this State Plan option to provide Medicaid-funded home and community-based attendant services and supports receive an FMAP increase of six percentage points for CFC services. In this year’s survey, four states (California, Maryland, Montana and Oregon) reported having CFC in place in FY 2014. Two states reported implementing this option in FY 2015 (New York8 and Texas), and four states reported plans to implement in FY 2016 (Connecticut, Delaware, Minnesota and Washington).
| Texas LTSS Transformation Initiatives |
|
In the last two years, Texas has implemented a number of initiatives to transform delivery of long-term care services and supports. Through managed care, the state has expanded its managed LTSS program statewide, carved nursing facility services into its managed care contracts and shifted acute care health services for individuals in its Section 1915(c) ICF/IDD waivers into managed care. Texas has also nearly completed implementation of the structural changes required under the Balancing Incentive Program (e.g., statewide expansion of the Aging and Disability Resource Centers and the automated LTSS Screening and Referral System) and implemented the Community First Choice Option. These initiatives combined with implementation of the Department of Labor rule on minimum wage and overtime for direct care workers and the HCBS settings final rule amount to the state undergoing an unprecedented transformation in a short timeframe. Texas is planning additional initiatives to further transform its delivery of long-term care services and supports. For example, the state is planning to implement the STAR Kids managed care program for children with disabilities, to do a pilot program for serving individuals with IDD in managed care, and eventually to carve into managed care long-term care services for those in the state’s IDD waiver. As part of the nursing facility carve-in initiative, Texas is also developing performance measures to monitor admissions and readmissions to nursing facilities with the goal of ensuring appropriate utilization of nursing facility services and reducing unnecessary institutionalizations. |
| HCBS Settings Rule |
| In January 2014, CMS issued a new HCBS regulation (the “HCBS Rule”) making a number of significant program changes including the addition of new requirements that define the qualities of settings that are eligible for Medicaid reimbursement under Section 1915(c) waivers, the Section 1915(i) HCBS State Plan Option and the Community First Choice Option.9 The HCBS Rule includes a transitional process for states to ensure that their waivers and state plans meet the HCBS settings requirements including a requirement for each state to submit a Statewide Transition Plan. In this year’s survey, states were asked to comment on significant issues, concerns or opportunities that have emerged to date related to the implementation of their HCBS Statewide Transition Plans.
States expressed concerns around the administrative cost and staffing challenges associated with implementation of the Statewide Transition Plan as well as evaluating and completing on-site provider assessments and validating provider self-assessments. States also highlighted challenges in terms of provider compliance and consumer impact concerns including loss of providers and services valued by consumers and the potential for service disruptions when consumers are transitioned to compliant settings. A few states commented on delays in CMS feedback on submitted plans while three states indicated that more CMS guidance would be helpful. A few states also expressed concerns about the challenges faced in rural areas and those associated with specific sub-populations (e.g. beneficiaries with behavioral issues that pose a risk to the public). On the other hand, some states cited opportunities presented by the HCBS Rule for increasing consumer choice and autonomy, increasing HCBS quality, ensuring more person-centered and person-directed service planning and provision, and providing new opportunities to work across state agencies and divisions. |
Table 13: Long-Term Care Expansions in all 50 States and DC, FY 2015 and 2016
| HCBS Waiver or SPA Expansions | Building Balancing Incentives in MLTSS | PACE Expansions | Total States with HCBS Expansions | |||||
| 2015 | 2016 | 2015 | 2016 | 2015 | 2016 | 2015 | 2016 | |
| Alabama | X | X | X | X | ||||
| Alaska | ||||||||
| Arizona | ||||||||
| Arkansas | X | X | ||||||
| California | X | X | X | X | X | X | X | X |
| Colorado | X | X | X | X | X | |||
| Connecticut | X | X | X | X | ||||
| Delaware | X | X | X | X | X | X | X | |
| DC | X | X | X | X | X | |||
| Florida | X | X | X | X | X | X | X | X |
| Georgia | X | X | ||||||
| Hawaii | X | X | X | X | ||||
| Idaho | X | X | X | X | ||||
| Illinois | X | X | X | X | X | X | ||
| Indiana | X | X | X | X | X | X | ||
| Iowa | X | X | X | X | X | |||
| Kansas | X | X | X | X | ||||
| Kentucky | X | X | X | X | ||||
| Louisiana | X | X | X | X | X | X | ||
| Maine | X | X | X | X | ||||
| Maryland | X | X | ||||||
| Massachusetts | X | X | X | X | X | X | X | X |
| Michigan | X | X | X | X | X | X | X | X |
| Minnesota | X | X | X | X | X | X | ||
| Mississippi | X | X | X | X | ||||
| Missouri | X | X | X | X | ||||
| Montana | X | X | X | X | ||||
| Nebraska | X | X | X | X | X | |||
| Nevada | X | X | X | X | ||||
| New Hampshire | X | X | X | X | ||||
| New Jersey | X | X | X | X | X | X | X | X |
| New Mexico | X | X | X | X | X | X | ||
| New York | X | X | X | X | X | X | X | X |
| North Carolina | X | X | ||||||
| North Dakota | X | X | X | |||||
| Ohio | X | X | X | X | X | X | ||
| Oklahoma | X | X | X | X | X | X | ||
| Oregon | X | X | X | X | X | X | ||
| Pennsylvania | X | X | X | X | X | X | ||
| Rhode Island | X | X | X | X | X | X | X | X |
| South Carolina | X | X | X | X | X | X | X | |
| South Dakota | X | X | X | X | ||||
| Tennessee | X | X | X | X | X | X | ||
| Texas | X | X | X | X | X | X | X | X |
| Utah | X | X | X | X | ||||
| Vermont | X | X | X | X | ||||
| Virginia | X | X | X | X | X | X | X | X |
| Washington | X | X | X | X | X | X | ||
| West Virginia | X | X | ||||||
| Wisconsin | X | X | X | X | X | X | ||
| Wyoming | X | X | X | X | X | X | ||
| Totals | 45 | 43 | 17 | 19 | 18 | 23 | 46 | 46 |
| NOTES: “HCBS Expansion” includes both expansions of 1915(c) waivers as well as 1915(i) State Plan Options SPAs. In addition to the actions reported here, states also reported expanding the number served in the community through the ACA Community First Choice Option as well as closing/downsizing state institutions and implementing/tightening certificate of need programs.
SOURCE: Kaiser Commission on Medicaid and the Uninsured Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2015. |
||||||||
Table 14: State Adoption of ACA LTSS Options in all 50 States and DC, FY 2014 – 2016
| 1915(i) State Plan Option | Community First Choice | Any ACA LTC Option | |||||||
| In Place | New in: | In Place | New in: | In Place | New in: | ||||
| 2014 | 2015 | 2016 | 2014 | 2015 | 2016 | 2014 | 2015 | 2016 | |
| Alabama | |||||||||
| Alaska | |||||||||
| Arizona | |||||||||
| Arkansas | |||||||||
| California | X | X | X | ||||||
| Colorado | X | X | |||||||
| Connecticut | X | X | X | X | X | X | |||
| Delaware | X | X | X | X | |||||
| DC | X | X | |||||||
| Florida | X | X | |||||||
| Georgia | |||||||||
| Hawaii | |||||||||
| Idaho | X | X | |||||||
| Illinois | |||||||||
| Indiana | X | X | X | X | |||||
| Iowa | X | X | |||||||
| Kansas | |||||||||
| Kentucky | |||||||||
| Louisiana | X | X | |||||||
| Maine | |||||||||
| Maryland | X | X | X | X | |||||
| Massachusetts | |||||||||
| Michigan | |||||||||
| Minnesota | X | X | X | ||||||
| Mississippi | X | X | |||||||
| Missouri | |||||||||
| Montana | X | X | X | ||||||
| Nebraska | |||||||||
| Nevada | X | X | |||||||
| New Hampshire | |||||||||
| New Jersey | |||||||||
| New Mexico | |||||||||
| New York | X | X | X | X | |||||
| North Carolina | |||||||||
| North Dakota | |||||||||
| Ohio | |||||||||
| Oklahoma | |||||||||
| Oregon | X | X | X | ||||||
| Pennsylvania | |||||||||
| Rhode Island | |||||||||
| South Carolina | |||||||||
| South Dakota | |||||||||
| Tennessee | |||||||||
| Texas | X | X | X | X | |||||
| Utah | |||||||||
| Vermont | |||||||||
| Virginia | |||||||||
| Washington | X | X | |||||||
| West Virginia | |||||||||
| Wisconsin | X | X | |||||||
| Wyoming | |||||||||
| Totals | 12 | 4 | 5 | 4 | 2 | 4 | 13 | 6 | 8 |
| NOTES: States were asked if each of these options were in place in FY 2014, implemented in FY 2015, or state planned to implement in FY 2016. States can implement multiple HCBS State Plan options focusing different populations. New York reported implementing the Community First Choice option in FY 2015, but was awaiting final SPA approval at the time of the survey.
SOURCE: Kaiser Commission on Medicaid and the Uninsured Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2015. |
|||||||||