Leveraging Medicaid in a Multi-Payer Medical Home Program: Spotlight on Rhode Island's Chronic Care Sustainability Initiative
Appendix 1: CSI Common Developmental Contract, April 2012
Performance Targets
Target 1: Structural Improvements (Practice Metric): Hire a nurse care manager; establish a compact with four specialists including a hospitalist; establish a plan/policy for after-hours care; have an electronic medical record and achieve Level 1 meaningful use; comply with the Quality Partners of Rhode Island Hospital and community physician best practices; demonstrate best practices for outpatient transitions of care; demonstrate use of evidence-based care; submit quality data
Target 2: Clinical Process Measures (Provider Metric): Achieve benchmark goals on specified CAHPS survey items; meet benchmark goal or achieve 50 percent improvement on at least four of seven metrics: Diabetes HbA1C <8, Diabetes BP<140/90,Diabetes LDL <100,Hypertension <140/90,Tobacco Cessation, Adult BMI (18-64), Adult BMI (65+)
Target 3: Outcome Measures (Provider Metric): CSI practices, in aggregate, to reduce emergency department and all-cause inpatient hospital admission rates by 7.5% and 5% respectively, relative to a comparison group
Staging
- Start-up Year
- Payments support transformation and measure development
- $4.50 PMPM to practices who attain NCQA Level 1 PCMH recognition, report common quality metrics, and achieve a number of process requirements.
- Practices are required to participate in project governance, evaluation and CSI learning collaborative.
- Transition Year
- Payment commits practices to use data measurement to drive performance
- $5.50 PMPM for demonstrating evidence of data-driven performance and attaining NCQA Level 2 recognition
- Performance Year 1
- Pay practices based on performance
- $5.00 PMPM if 0-1 performance targets are met
- $5.50 PMPM if 2 performance targets are met
- $6.00 PMPM if all 3 performance targets are met
- Practices agree to attain NCQA Level 3 PCMH recognition by end of performance year 2
- Performance Year 2
- Pay practices based on performance
- $5.00 PMPM if 0-1 performance target is met
- $5.50 if two performance targets are met
- $6.00 if all three performance targets are met
- Practices must attain NCQA Level 3 PCMH recognition by end of year
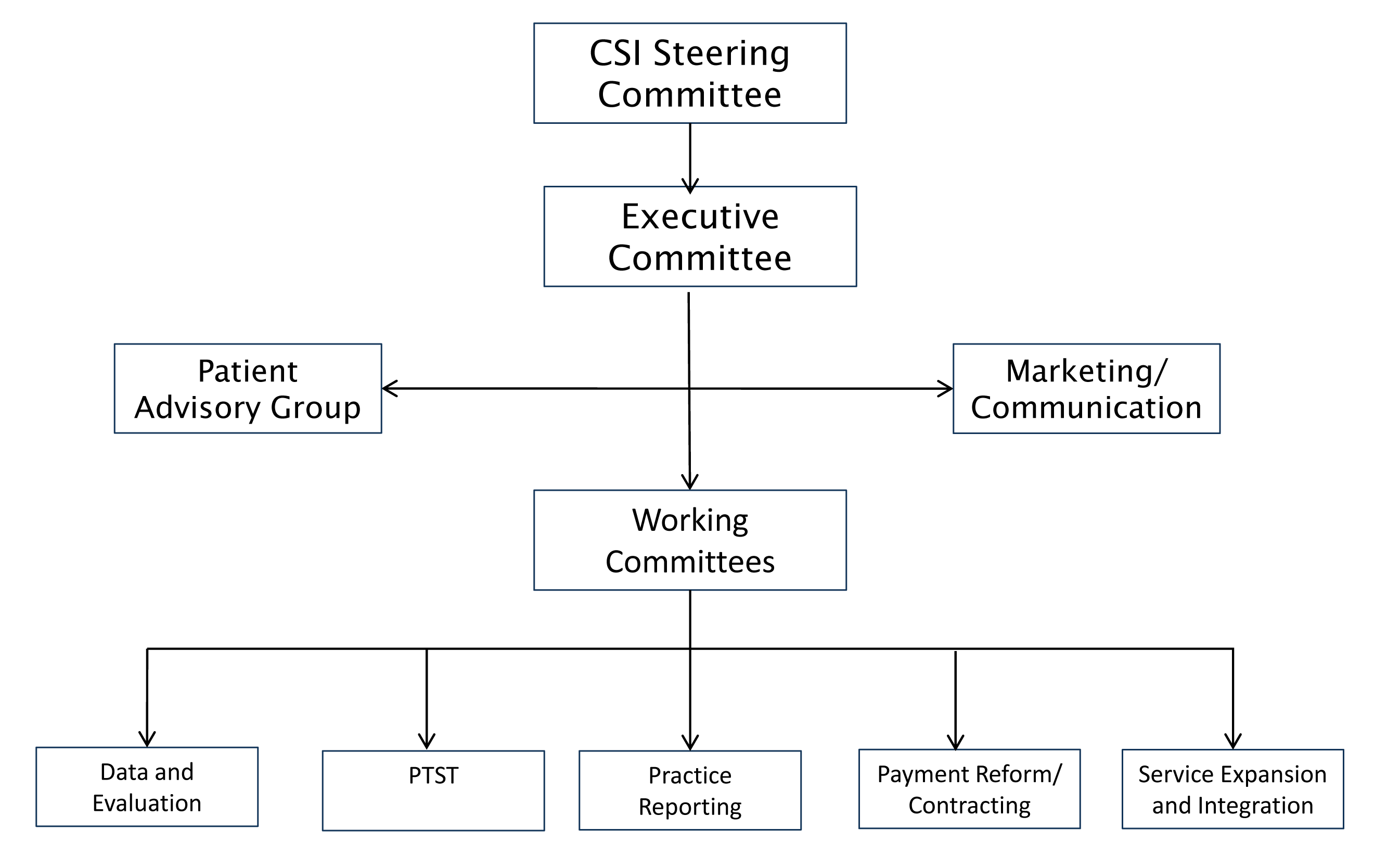
Appendix 2: CSI Governance Structure
Source: CSI-RI: Strategic Planning, Final Plan, February 21, 2013.
http://www.pcmhri.org/files/uploads/CSI_Strategic_Plan_Summary%20March%202013.pdf
Appendix 3: CSI Working Committees: Purpose and Scope
- Data and Evaluation– performance improvement; measure selection; measurement definition/harmonization; goals and benchmarks; evaluation; research; and liaison with other committees
- Practice Training Support and Transformation– conferences, learning collaboratives, coaching, and other forms of assistance
- Practice Reporting– review of quarterly practice data, data validation and public reporting, support for practice improvement and data sharing, support with EHR/IT issues
- Payment Reform/Contracting– contract development, patient attribution, alternative payment models, issues associated with PCMH as part of a delivery system
- Service Expansion and Integration– develop additional service capabilities (e.g., behavioral health, transitional care, oral health) and expand to additional populations (e.g., dual eligibles, children)
Source: CSI-RI: Strategic Planning, Final Plan, February 21, 2013.
http://www.pcmhri.org/files/uploads/CSI_Strategic_Plan_Summary%20March%202013.pdf