CHIP Enrollment Snapshot: December 2013
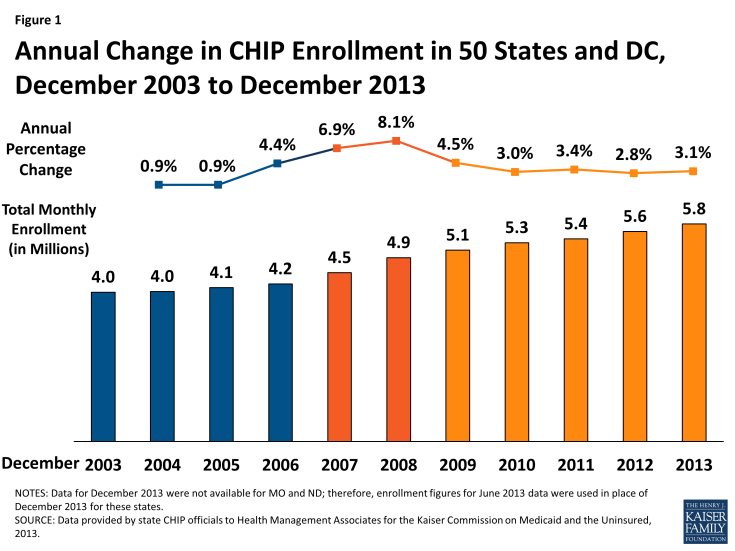
In December 2013, nearly 5.8 million children were enrolled in the Children’s Health Insurance Program (CHIP.) Enrollment in December 2013 increased on net by 175,020 or by 3.1 percent, compared to one year earlier. Since 2011, annual rates of growth have remained fairly steady, hovering around 3 percent. In contrast, during the height of the Recession, enrollment increased annually by 6.9 to 8.1 percent. (Figure 1, Appendix Tables 1 and 2)
CHIP, combined with Medicaid, provides a crucial safety net of coverage for low-income children. Both programs, aided by maintenance of eligibility (MOE) provisions maintained under the Affordable Care Act (ACA) helped to stave off increases in the number of uninsured children. Between 2007 and 2012, the uninsured rate for children dropped from 10.9% to 9.2%, despite a decline in the share of children with employer-sponsored coverage.1 While the MOE provisions for adults ended in January 2014, the MOE provisions for children remain in effect until October 2019. However, the ACA only extended CHIP funding through October 2015; Congress would need to appropriate additional funds in order for allotments to be available after October 2015. This, combined with the advent of new coverage options available through the marketplaces, raises questions about the program’s future role.
This report focuses on changes in monthly CHIP enrollment between December 2012 and December 2013. This is a long standing report that collects monthly CHIP enrollment data for December (and June, not reported here) going back to 2000. The most recent data included in this report predate preliminary data released by CMS that show the early effects of full implementation of the ACA. While the data provided in this report are not directly comparable to the data released by CMS (see methodology for more details,) they provide context for the preliminary data released by CMS, illustrating historical trends in CHIP enrollment.
ACA Eligibility Changes for Children
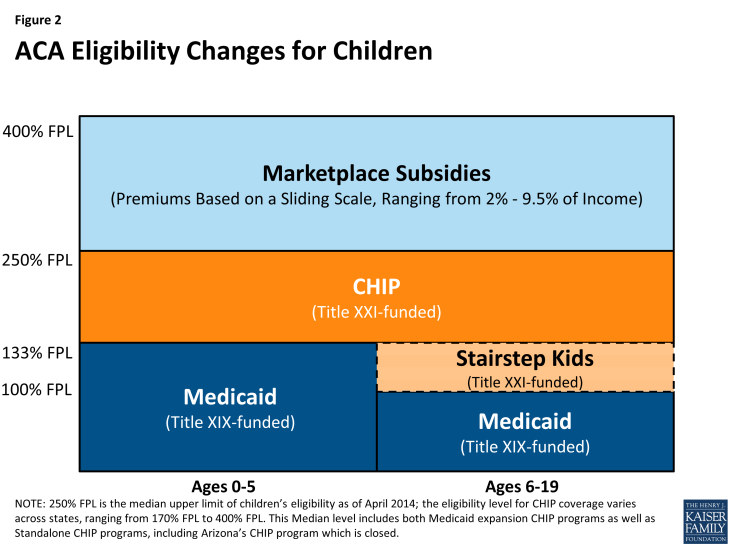
The ACA requires that Medicaid cover children with incomes up to 133 percent of the federal poverty level (FPL) as of January 2014. Before this change, states were required to cover children under the age of six in families with income of at least 133 percent FPL and school-age children and teens with incomes up to 100 percent FPL in Medicaid. Many states already covered children with incomes up to 133 percent FPL in Medicaid, but due to the change in law, 21 states needed to transition some children, mostly school-age children with incomes between 100 and 133 (a.k.a. Stairstep children) from their CHIP state plans to their Medicaid state plans.2 (Figure 2) These children remain eligible for the Title XXI Federal CHIP match rate.
As of April 2014, more than half of the states (29, including DC) cover children in families with incomes at or above 250% FPL and 19, including DC, cover children in families with incomes at or above 300% FPL either through Medicaid or CHIP. Thirty-seven states continue to operate standalone CHIP programs, most in combination with CHIP Medicaid expansions, for higher income children.3
A few of the 21 states that covered “Stairstep” children under separate CHIP programs decided to move these children before the requirement was in place. New York and Colorado implemented an early transition of children from CHIP to Medicaid but are maintaining separate CHIP programs. Meanwhile, New Hampshire and most recently California transitioned all CHIP kids to Medicaid, not just these older children with incomes under 133 percent FPL. The remaining 17 states will transition an estimated 13 percent to 48 percent of their CHIP coverage to Medicaid.4
Continued improvement in economic conditions likely resulted in both some growth as children shifted from Medicaid to CHIP and some declines as family incomes continued to increase above CHIP eligibility levels. CHIP offers coverage to low-income children in families who do not have access to affordable coverage but whose incomes are above Medicaid eligibility levels. Therefore, economic pressures provide both upward and downward pressure on enrollment. As the economy continues to improve, as it did during 2013, family income rises, which results in some children shifting from Medicaid to CHIP coverage. However, economic conditions improving can also result in some children leaving the program as income increases above CHIP eligibility levels for higher income families.During the period from December 2012 to December 2013, there were a number of factors likely influencing CHIP enrollment in different directions, most notably:
Successful outreach and enrollment efforts for new Marketplaces likely pushed enrollment up in some states. Implementation of the major coverage provisions of the ACA had begun but had not been completed. Broad outreach efforts to encourage individuals to apply for coverage (through CHIP, Medicaid, or the Marketplaces) were well underway; such efforts in the past have been noted to apply upward pressure on CHIP enrollment. CHIP programs also face the same ACA requirements in terms of enrollment simplifications, coordination with Medicaid and the new Marketplaces, as well as the use of Modified Adjust Gross Income beginning in 2014. The full effect of these changes would occur just after this data collection period.
Problems implementing new enrollment systems for the Federally Facilitated Marketplace (FFM) and State Based Marketplaces (SBM) likely put downward pressure on CHIP enrollment growth. States and the Federal Government faced IT systems challenges, particularly early on in the open enrollment period, which may have applied some downward pressure on CHIP enrollment during this period. States that relied on FFMs had significant problems with “account transfers” from the FFM to agencies handling CHIP enrollment. Many children were assessed or determined eligible for CHIP through the FFMs, but because of system problems, accounts could not be easily transferred to effectuate enrollment. There were also some SBMs that also faced similar issues. Although problems persist, some progress in resolving these issues was made after the timeframe for this report.
Enrollment Trends
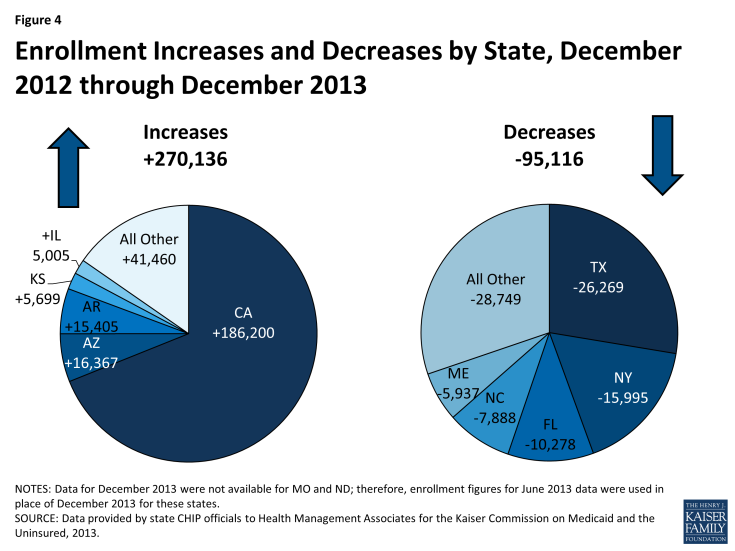
On net, CHIP enrollment increased by 175,020 between December 2012 and December 2013 despite slow enrollment growth in the second half of the period. CHIP enrollment increased to nearly 5.8 million as 175,020 more individuals (on net) were enrolled in coverage in December 2013 compared to December 2012. Enrollment growth over the year was on track with previous trends but slowed in the second half of this 12 month period (June 2013 to December 2013.) There were 144,412 more children on net enrolled in CHIP in June 2013 compared to December 2012; in contrast, CHIP enrollment increased by only 30,608 between June 2013 and December 2013. (Figure 3) The slow growth noted in the second half of the year (June 2013 to December 2013,) may be a reflection of the initial difficulties states and the federal government faced with IT systems and file transfers.
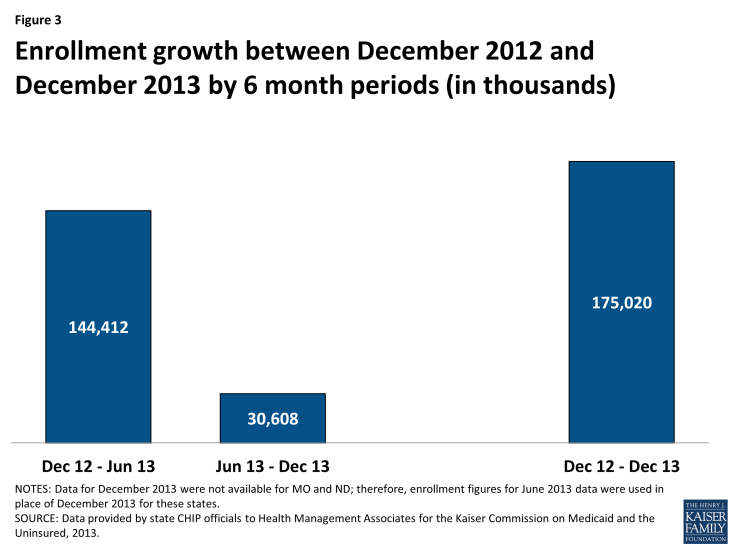
Figure 3: Enrollment growth between December 2012 and December 2013 by 6 month periods (in thousands)
The net CHIP enrollment growth includes increases in 29 states and decreases in 22 states. Over half of states (29) reported enrollment increases during this period as 270,136 more children were enrolled in CHIP in these states in December 2013 compared to one year earlier. In contrast, 22 states saw enrollment declines as 95,116 fewer children were enrolled in these states in December 2013 compared to one year earlier. (Figure 4)
The three states that were driving these increases include:
- California’s CHIP enrollment increased in California by 16.4 percent as 186,200 additional children were enrolled in December 2013 compared to December 2012. It is important to note that the transition of children previously enrolled in the Title XXI Healthy Families to Medi-Cal (Medicaid) would not affect CHIP enrollment numbers reflected in this report because these children are still included in the CHIP counts. The increase in the number of children enrolled in CHIP may be related to outreach and enrollment efforts tied to expanded Medicaid and CHIP coverage programs in California, and also to the improving economy with children moving up the income scale between Medicaid and CHIP.
- Arizona saw CHIP enrollment growth of 54 percent as an additional 16,367 children were enrolled in CHIP in December 2013 compared to one year earlier due to a new temporary program, KidsCare II, that began enrolling children in May 2012. This program ended January 31, 2014; the state sent out notices to approximately 14,000 families with incomes over 133% FPL that they would need to apply for coverage through the Marketplace. The original KidsCare program still exists, but enrollment remains frozen, meaning no new applications are being accepted and children who lose this coverage due to failure to pay premiums will not be able to reenroll later. According to the state, just over 2,600 children remain enrolled in the original KidsCare program.5 The original KidsCare has been closed to new enrollment since December 2009 due to state budget shortfalls. CHIP enrollment steadily declined for several reporting periods, reaching its lowest level in over a decade in June 2012, when enrollment totaled only 12,238 (compared to over 64,000 before the enrollment freeze was first implemented.)
- Arkansas saw a 20 percent increase in CHIP enrollment between December 2013 and December 2012 as enrollment increased by 16,367. All of this enrollment growth occurred in the second half of the period; Arkansas actually saw a small decline in CHIP enrollment in the first six months of this period (December 2012 to June 2013.) It is likely that the sharp increase in enrollment was due in part to the state’s adoption of fast track enrollment options made available through CMS in an effort to help states launch the Medicaid expansion and efficiently enroll eligible individuals. Specifically, Arkansas was one of five states that implemented the fast track enrollment option allowing states to enroll individuals based on existing data from their Supplemental Nutrition Assistance Program. Arkansas, along with West Virginia, used this process to not only enroll adults but also children who were eligible but not enrolled.6
The largest declines in CHIP enrollment occurred in Texas, New York, and Flordia; the factors underlying these declines however are not readily apparent.
CONCLUSION
Overall, CHIP enrollment growth remained on track with previous trends, despite much slower growth seen in the second half of this period (June 2013 to December 2013.) Economic improvements apply both upward and downward pressure on CHIP enrollment; as income increases some children shift from Medicaid to CHIP while others transition off the program as their income rises above CHIP eligibility levels. Like Medicaid, CHIP programs also saw some upward (through increased outreach) and downward pressure (from enrollment systems issues) related to the implementation of the ACA. CHIP programs, along with state Medicaid programs continue to play a critical role in assuring health coverage for uninsured children. However, the future of the program remains uncertain as funding is slated to end in October 2015 unless Congress acts.