The ACA Primary Care Increase: State Plans for SFY 2015
To increase support for physicians providing primary care for Medicaid beneficiaries, and to improve access to primary care as Medicaid coverage expands, the Affordable Care Act (ACA) increased Medicaid payment rates for many primary care services to Medicare fee levels in 2013 and 2014. The rate increase applies only to physicians, serving Medicaid beneficiaries in both fee-for-service and managed care. The federal government funded 100% of the primary care fee increase relative to the rates states were paying as of July 1, 2009. As part of the KCMU’s Annual Medicaid Budget Survey, states were asked about their plans to extend the primary care rate increase beyond December 31, 2014 (at regular FMAP rates).
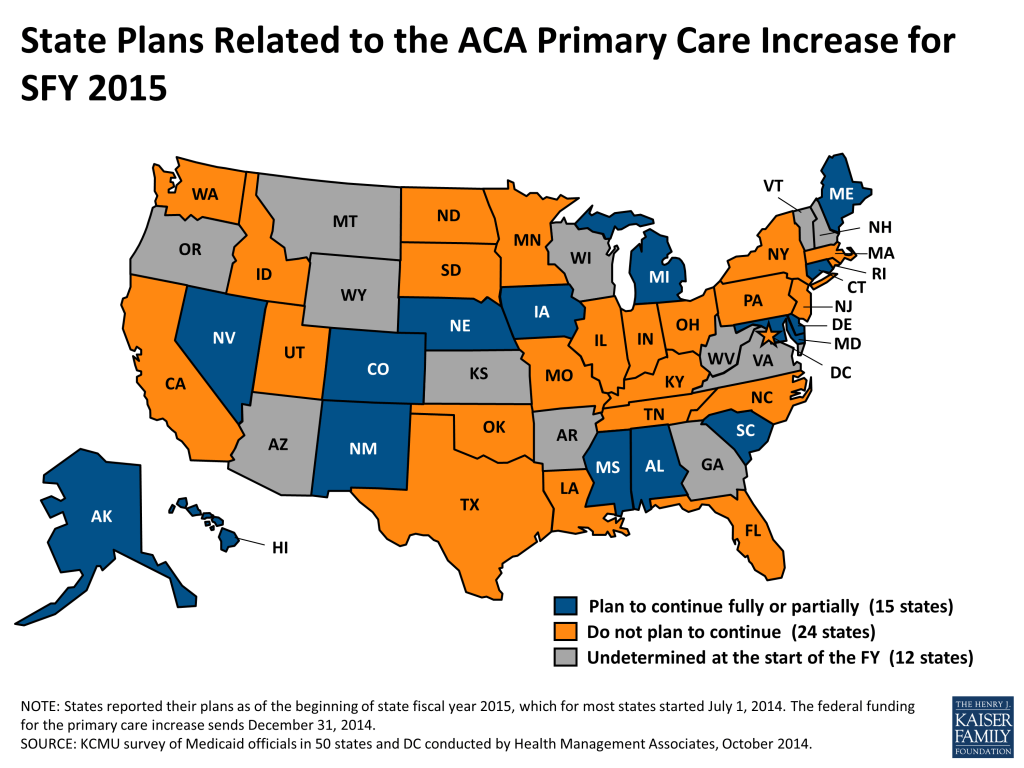
Plan to continue the increase. Fifteen states indicated that they will continue the primary care fee increase in 2015, at least in part. The 100% federal funding for rate increase ends on December 31, 2014, so these states will continue the increase at their regular federal matching rate. For states that were paying primary care physicians close to 100% of Medicare rates even before the ACA (such as Alaska, whose rates were 124% of Medicare rates), extending the ACA increase does not impose significant new costs. However, most states noted a sizable increase in state funds required to continue the primary care increase. In particular, six states (Colorado, Hawaii, Maryland, Maine, Michigan and Nevada) had primary care payment rates in fee-for-service that were at or below 75% of Medicare levels prior to the ACA primary care increase.1 Nine states (Alabama, Alaska, Connecticut, Delaware, Iowa, Mississippi, Nebraska, New Mexico and South Carolina) had fees that were at or above 76% of Medicare fee levels.2 Some states also noted that they were changing the terms of the ACA primary care increase by adding or limiting the types of providers who would receive the increase. For example, Connecticut reported plans to apply the increase to Advanced Practice Registered Nurses (APRNs) in light of a change in the state’s scope-of-practice laws. South Carolina noted plans to limit the increase to specific primary care providers (e.g., general pediatricians, general internal medicine physicians, general family medicine physicians, general obstetricians, and general psychiatrists.) Other states noted plans to finance only part of the increase; for example, Michigan reported plans to fund half of the value of the increase. The survey only asked states about plans for SFY 2015, but some states did note that continuing the increase in future fiscal years was a likely topic of debate for the next legislative session.
Do not plan to continue the increase. Twenty-four states reported that they did not plan to continue the ACA primary care increase after the 100% federal funding ends on December 31, 2014. Nine of these states (District of Columbia, Idaho, Kentucky, Massachusetts, North Carolina, North Dakota, Oklahoma, South Dakota and Washington3 ) previously paid most primary care physicians in fee-for-service at or above 76% of Medicare rates, including North Dakota, which paid at 134% of the Medicare rates.4 However, the remaining states reimbursed most primary care physicians at or below 75% of Medicare rates.5 A number of states reported that the cost of extending the rate increase was too high for states to continue it. Additionally, some of the states that did not plan to continue the ACA primary care increase, such as Florida, did note that they planned to increase rates for some primary care providers relative to rates before the ACA increase, but on a more limited basis (e.g., to pediatricians only.)
Undetermined. Tweleve states indicated they had not yet made a decision on this policy and were still evaluating whether the enhanced rates had any impact on provider participation. Many of these states (along with some states that reported no plans to continue the increase) noted that they were waiting to see if any federal action would be taken to extend the 100% federal financing past December 31, 2014.6
Impact on Provider Participation. Given the delayed implementation of the ACA primary care increase, the challenges related to implementation7 and the difficulty of attributing changes in provider enrollment and access to the enhanced payments (particularly for providers in managed care), the impact of the rate increase is difficult to determine. Many states noted that they were still evaluating the impact of the ACA primary care increase on provider participation in their Medicaid programs. While a small number of states noted expectations of little to no effect on provider participation in their states, other states, such as Connecticut, reported significant new provider participation in Medicaid due to the increase.
Additional Resources on the ACA Primary Care Increase
- For more information on the specifics of the ACA increase (such as the providers included and requirements,) please see the following issue brief: https://www.kff.org/health-reform/issue-brief/increasing-medicaid-payments-for-certain-primary-care/
- For more information on what Medicaid physician fees were prior to the ACA primary care increase, see the following issue brief: https://www.kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/
- Stephen Zuckerman and Dana Goin, How Much Will Physician Fees for Primary Care Rise in 2013? Evidence from a 2012 Survey of Medicaid Physician Fees, (Kaiser Family Foundation, December 2012.) https://modern.kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Reimbursement rates reported reflect payment rates in 2012 through fee-for-services, not managed care. ↩︎
- Stephen Zuckerman and Dana Goin, How Much Will Physician Fees for Primary Care Rise in 2013? Evidence from a 2012 Survey of Medicaid Physician Fees, (Kaiser Family Foundation, December 2012.) https://modern.kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Reimbursement rates reported reflect payment rates in 2012 through fee-for-services, not managed care. ↩︎
- Washington state reimbursed most primary care providers in fee-for-service at 76% of Medicare rates before the ACA primary care increase went into effect. However, the state reported that without a continuation of the ACA primary care increase, they expect a drop in some adult codes. ↩︎
- Stephen Zuckerman and Dana Goin, How Much Will Physician Fees for Primary Care Rise in 2013? Evidence from a 2012 Survey of Medicaid Physician Fees, (Kaiser Family Foundation, December 2012.) https://modern.kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Reimbursement rates reported reflect payment rates in 2012 through fee-for-services, not managed care. ↩︎
- Stephen Zuckerman and Dana Goin, How Much Will Physician Fees for Primary Care Rise in 2013? Evidence from a 2012 Survey of Medicaid Physician Fees, (Kaiser Family Foundation, December 2012.) https://modern.kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/. Reimbursement rates reported reflect payment rates in 2012 through fee-for-services, not managed care. ↩︎
- A few states, such as Colorado, which noted plans to continue the ACA primary care increase with some modifications (such as removing attestation) expressed concerns about the federal government extending the federal funding for the ACA increase after December 31, 2014, (with the same requirements) as it would be difficult to undo such modifications. ↩︎
- For more information on the challenges states reported in implementing this provision, please see the relevant section on provider rates of last year’s Annual Medicaid Budget Survey report (page 49): https://modern.kff.org/medicaid/report/medicaid-in-a-historic-time-of-transformation-results-from-a-50-state-medicaid-budget-survey-for-state-fiscal-years-2013-and-2014/ ↩︎