State-by-State Estimates of Reductions in Federal Medicaid Funding Under Repeal of the ACA Medicaid Expansion
The Senate is currently considering the Obamacare Repeal Reconciliation Act of 2017. While there are a number of provisions that affect Medicaid, the primary change would be the elimination of the statutory authority to cover childless adults up to 138% FPL ($16,643 for an individual in 2017) as well as an elimination of the enhanced match rate for the Medicaid expansion.
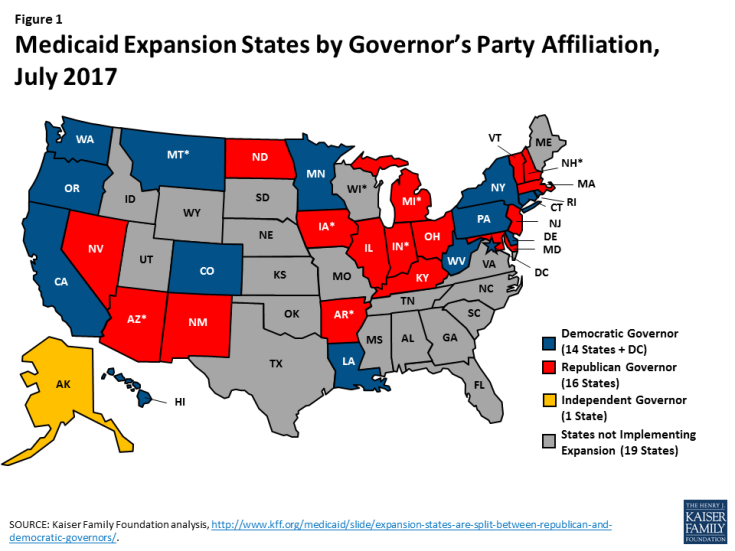
A repeal of the Medicaid expansion would have significant coverage and financing implications for the 31 states and the District of Columbia that have implemented the expansion (Figure 1). We estimated changes in federal Medicaid funds and Medicaid coverage for adults covered through the ACA expansion, assuming that the Medicaid expansion would be repealed as of 2020. We assume all states drop all expansion/Group VIII coverage, and the analysis does not account for continuation of expansion coverage in states that had waivers prior to the ACA (more detail on the methods underlying the estimates is in the Methods box below).
Our analysis shows that states would see a $700 billion reduction in federal Medicaid funds over the 2020-2026 period due to the loss of the ACA expansion (Table 1). In the last year of this analysis, 2026, states would see a reduction in federal Medicaid funds of $121 billion and estimated reductions in coverage of 17.6 million (19% of total Medicaid enrollment that year). In 11 states, the loss of the expansion would reduce Medicaid enrollment by 30% or more in 2026. In the absence of other affordable coverage, it is likely that most of these people would become uninsured, which would affect their access to health care services.
| Table 1: Potential Loss of Federal Medicaid $ and Medicaid Coverage Under Repeal of ACA Medicaid Expansion, 2020-2026 | ||||
| Loss of Federal $ for Expansion, 2020-2026 | Loss of Federal $ for Expansion, 2026 | Loss of Expansion Enrollment, 2026 | ||
| State | $ Millions | $ Millions | # | % Change in Total Enrollment |
| US total | -700,250 | -120,635 | -17,627,000 | -19% |
| Alaska | -2,143 | -369 | -39,000 | -19% |
| Arizona | -21,043 | -3,625 | -496,000 | -21% |
| Arkansas | -12,850 | -2,214 | -360,000 | -19% |
| California | -180,423 | -31,082 | -4,198,000 | -28% |
| Colorado | -12,979 | -2,236 | -504,000 | -29% |
| Connecticut | -12,637 | -2,177 | -246,000 | -24% |
| Delaware | -3,855 | -664 | -80,000 | -31% |
| District of Columbia | -2,925 | -504 | -74,000 | -23% |
| Hawaii | -4,701 | -810 | -130,000 | -31% |
| Illinois | -28,432 | -4,898 | -807,000 | -21% |
| Indiana | -21,078 | -3,631 | -452,000 | -31% |
| Iowa | -6,639 | -1,144 | -177,000 | -23% |
| Kentucky | -25,887 | -4,460 | -525,000 | -32% |
| Louisiana | -12,592 | -2,169 | -481,000 | -24% |
| Maryland | -14,365 | -2,475 | -294,000 | -20% |
| Massachusetts | -15,448 | -2,661 | -472,000 | -19% |
| Michigan | -29,889 | -5,149 | -755,000 | -25% |
| Minnesota | -16,510 | -2,844 | -264,000 | -18% |
| Montana | -2,960 | -510 | -75,000 | -30% |
| Nevada | -8,569 | -1,476 | -242,000 | -34% |
| New Hampshire | -2,756 | -475 | -63,000 | -26% |
| New Jersey | -23,568 | -4,060 | -655,000 | -32% |
| New Mexico | -12,603 | -2,171 | -288,000 | -28% |
| New York | -91,955 | -15,841 | -2,562,000 | -31% |
| North Dakota | -1,375 | -237 | -25,000 | -22% |
| Ohio | -30,915 | -5,326 | -809,000 | -21% |
| Oregon | -23,335 | -4,020 | -653,000 | -47% |
| Pennsylvania | -36,748 | -6,331 | -833,000 | -25% |
| Rhode Island | -4,027 | -694 | -72,000 | -21% |
| Vermont | -2,362 | -407 | -75,000 | -33% |
| Washington | -28,249 | -4,867 | -705,000 | -31% |
| West Virginia | -6,436 | -1,109 | -214,000 | -29% |
| NOTE: Assumes all states drop all expansion/Group VIII coverage starting in 2020. Does not account for any continuation of expansion coverage in states that had waivers prior to the ACA.
SOURCE: Kaiser Family Foundation estimates, July 2017. |
||||
| Methods |
| This analysis is based on Kaiser Family Foundation estimates using data from the Medicaid Statistical Information System (MSIS), Medicaid Budget and Expenditure System (MBES), CMS-64, and CMS Office of the Actuary (OACT) and Congressional Budget Office (CBO) projections about future Medicaid spending.
2016 Base. We generated estimates of Medicaid enrollment and spending for expansion enrollees in FY2016 based on Kaiser Family Foundation analysis of the FY2015 MSIS. We adjusted MSIS spending to CMS-64 spending to account for MSIS undercounts of spending. Because FY2015 MSIS data was missing some or all quarters for some states, we also adjusted the enrollment data using secondary data to represent a full fiscal year of enrollment. We accounted for a state’s expansion status, the number of quarters of missing data, and the state’s historical patterns of spending and enrollment in making state-by-state adjustments, using similar methods we used for estimates for earlier years. Because MSIS does not identify adults who are eligible through the ACA expansion versus pre-ACA pathways, we used the FY2015 MBES data to break out enrollment and spending for Group VIII (ACA expansion) enrollees. We then inflated to FY2016 based on the OACT estimates of annual changes in enrollment and spending by eligibility group, with the exception of enrollment for Group VIII, which was obtained from the available FY2016 MBES data. In some cases (e.g., states that expanded after FY2015), we made state-specific adjustments to the data. Baseline Projections. We used the FY2016 base year data to project future Medicaid enrollment and spending. Because there is uncertainty around future growth rates in Medicaid and estimates vary widely, we used the average of OACT and CBO predictions of future growth in Medicaid enrollment and spending per enrollee by eligibility group. We applied the same growth rates to all states. We calculated the federal/state split in spending by enrollment group for each year based on the relevant FMAP for the eligibility group and year. For non-expansion groups, we used the most recent FMAPs available (FY2018) for all years; for expansion groups, we used the FMAPs for each year as specified under current law, though we did not account for differential match rates for Group VIII enrollees who are not newly eligible and may qualify for a different match rate. Since these projections use national data and uniform growth rates, state individual state estimates may have more detailed data. ACA Repeal. For purposes or repealing the ACA, we assume all spending and coverage in the expansion group (Group VIII) are eliminated starting in 2020. These estimates do not assume that states make other changes to maintain this coverage (even for states that had waiver coverage prior to the ACA). |